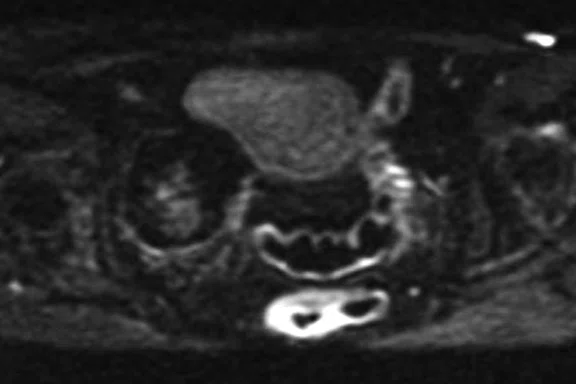
A
Figure 4.
Four slices from a MUSE acquisition (b800 s/mm2) in the pelvis of a 71-year-old female. The images show a right adnexal lesion (arrow) that may represent an ectopic fibroid.
B
Figure 4.
Four slices from a MUSE acquisition (b800 s/mm2) in the pelvis of a 71-year-old female. The images show a right adnexal lesion (arrow) that may represent an ectopic fibroid.
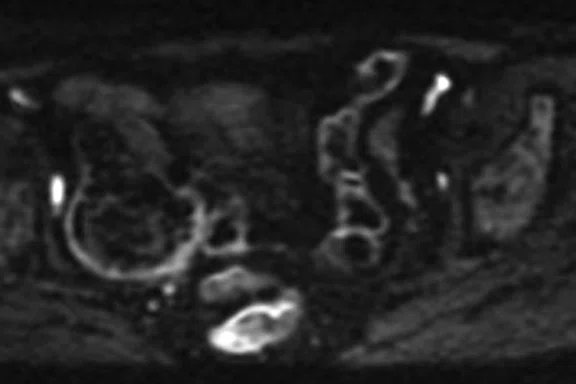
C
Figure 4.
Four slices from a MUSE acquisition (b800 s/mm2) in the pelvis of a 71-year-old female. The images show a right adnexal lesion (arrow) that may represent an ectopic fibroid.
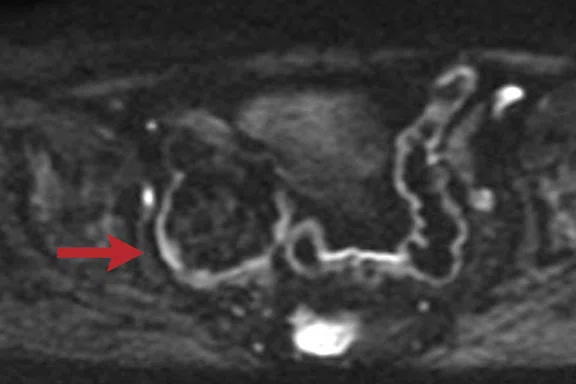
D
Figure 4.
Four slices from a MUSE acquisition (b800 s/mm2) in the pelvis of a 71-year-old female. The images show a right adnexal lesion (arrow) that may represent an ectopic fibroid.
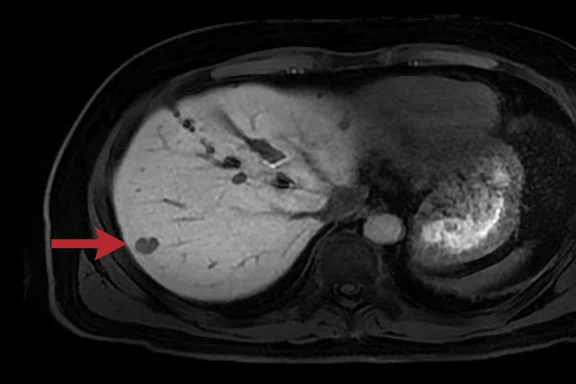
A
Figure 1.
Male patient with a hemangioma in segment 7 of the liver (arrow) 20 minutes after injection of a hepatospecific contrast agent. (A) Original breath-hold LAVA Flex protocol with a voxel size of 1.2 x 1.8 x 2.2 mm; (B) revised protocol with a voxel size of 1.4 x 1.4 x 1.4 mm; and (C, D) sagittal and coronal reformats of the isotropic 1.4 mm data.
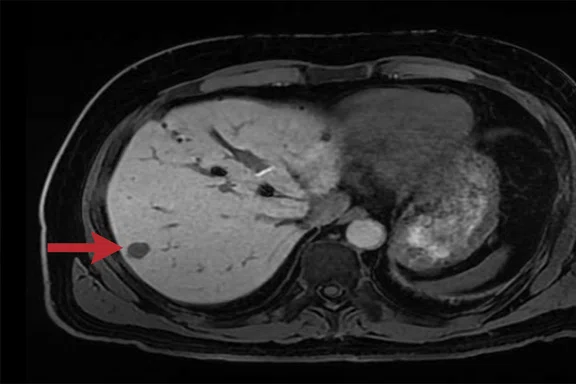
B
Figure 2.
Male patient with a hemangioma in segment 7 of the liver (arrow) 20 minutes after injection of a hepatospecific contrast agent. (A) Original breath-hold LAVA Flex protocol with a voxel size of 1.2 x 1.8 x 2.2 mm; (B) revised protocol with a voxel size of 1.4 x 1.4 x 1.4 mm; and (C, D) sagittal and coronal reformats of the isotropic 1.4 mm data.
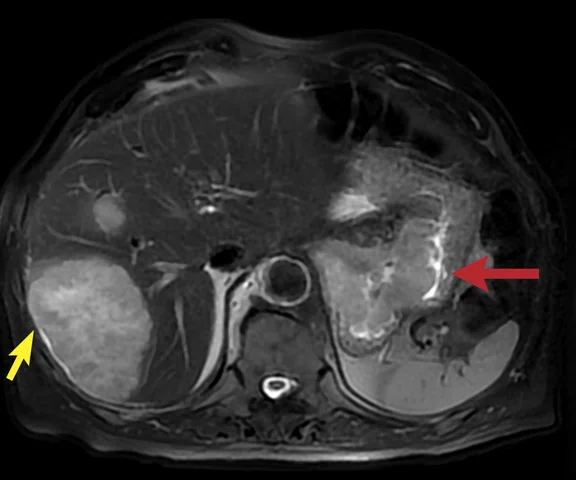
A
Figure 2.
A 75-year-old male with a gastric tumor (red arrow) and large liver metastases (yellow arrow). (A) Axial navigated PROPELLER T2w FatSat with a voxel size of 1.4 x 1.4 x 6 mm; (B) axial navigated DWI with b600 s/mm2 and voxel size of 5 x 3.1 x 6 mm; and (C, D) two axial slices from the delayed phase free-breathing (navigated) DISCO LAVA with a voxel size of 1.6 x 2.1 x 2.2 mm.
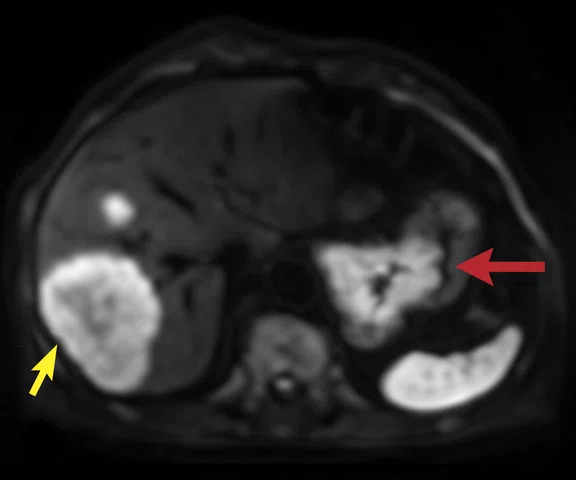
B
Figure 2.
A 75-year-old male with a gastric tumor (red arrow) and large liver metastases (yellow arrow). (A) Axial navigated PROPELLER T2w FatSat with a voxel size of 1.4 x 1.4 x 6 mm; (B) axial navigated DWI with b600 s/mm2 and voxel size of 5 x 3.1 x 6 mm; and (C, D) two axial slices from the delayed phase free-breathing (navigated) DISCO LAVA with a voxel size of 1.6 x 2.1 x 2.2 mm.
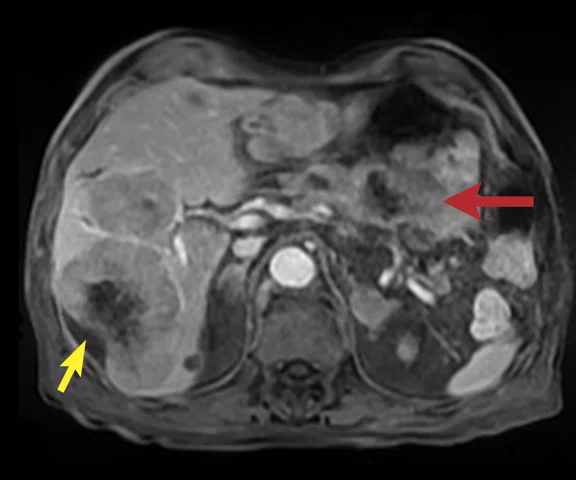
C
Figure 2.
A 75-year-old male with a gastric tumor (red arrow) and large liver metastases (yellow arrow). (A) Axial navigated PROPELLER T2w FatSat with a voxel size of 1.4 x 1.4 x 6 mm; (B) axial navigated DWI with b600 s/mm2 and voxel size of 5 x 3.1 x 6 mm; and (C, D) two axial slices from the delayed phase free-breathing (navigated) DISCO LAVA with a voxel size of 1.6 x 2.1 x 2.2 mm.
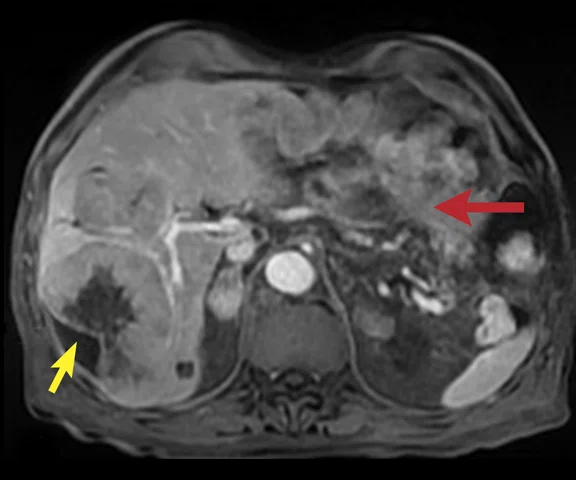
D
Figure 2.
A 75-year-old male with a gastric tumor (red arrow) and large liver metastases (yellow arrow). (A) Axial navigated PROPELLER T2w FatSat with a voxel size of 1.4 x 1.4 x 6 mm; (B) axial navigated DWI with b600 s/mm2 and voxel size of 5 x 3.1 x 6 mm; and (C, D) two axial slices from the delayed phase free-breathing (navigated) DISCO LAVA with a voxel size of 1.6 x 2.1 x 2.2 mm.
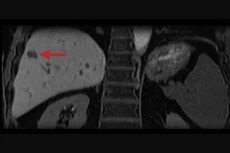
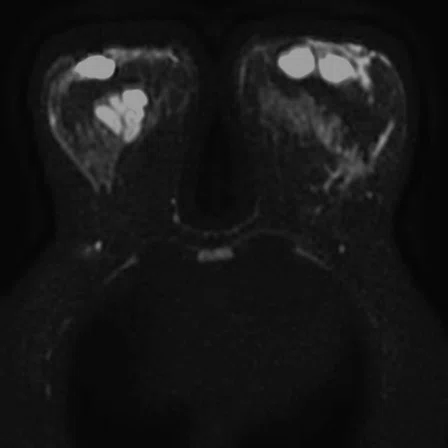
C
Figure 3.
Patient referred for breast cancer staging. (A) Axial DWI with b800 s/mm2 using our original protocol with a voxel size of 3.7 x 2.8 x 3.5 mm; (B) axial slice acquired using a 2-shot MUSE acquisition with a voxel size of 2.2 x 2.2 x 3.5 mm; (C) coronal reformat of the axial DWI data acquired in 6 min.; and (D) coronal reformat of the 2-shot MUSE data acquired in 9 min.
D
Figure 3.
Patient referred for breast cancer staging. (A) Axial DWI with b800 s/mm2 using our original protocol with a voxel size of 3.7 x 2.8 x 3.5 mm; (B) axial slice acquired using a 2-shot MUSE acquisition with a voxel size of 2.2 x 2.2 x 3.5 mm; (C) coronal reformat of the axial DWI data acquired in 6 min.; and (D) coronal reformat of the 2-shot MUSE data acquired in 9 min.
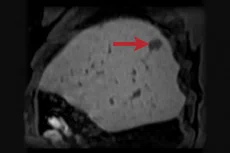
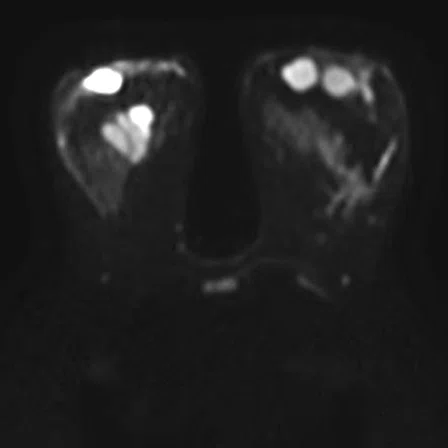
A
Figure 3.
Patient referred for breast cancer staging. (A) Axial DWI with b800 s/mm2 using our original protocol with a voxel size of 3.7 x 2.8 x 3.5 mm; (B) axial slice acquired using a 2-shot MUSE acquisition with a voxel size of 2.2 x 2.2 x 3.5 mm; (C) coronal reformat of the axial DWI data acquired in 6 min.; and (D) coronal reformat of the 2-shot MUSE data acquired in 9 min.
B
Figure 3.
Patient referred for breast cancer staging. (A) Axial DWI with b800 s/mm2 using our original protocol with a voxel size of 3.7 x 2.8 x 3.5 mm; (B) axial slice acquired using a 2-shot MUSE acquisition with a voxel size of 2.2 x 2.2 x 3.5 mm; (C) coronal reformat of the axial DWI data acquired in 6 min.; and (D) coronal reformat of the 2-shot MUSE data acquired in 9 min.
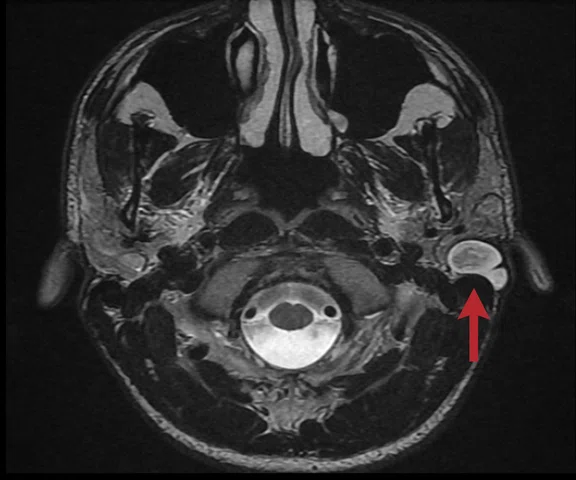
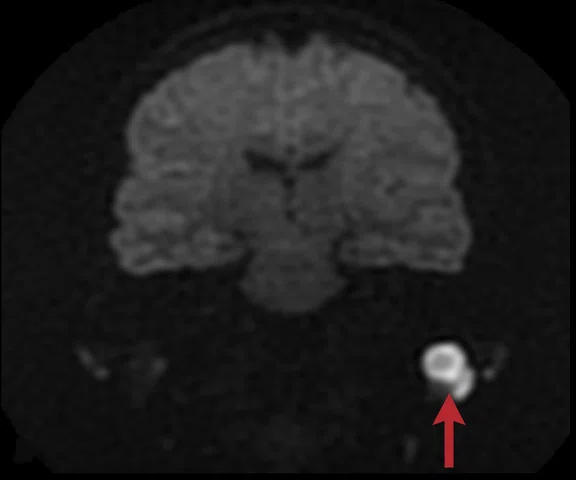
A
Figure 5.
A 17-year-old male with a left cholesteatoma (arrow). (A) Axial fast recovery FSE sequence with a voxel size of 0.4 x 0.7 x 2.0 mm and (B) true coronal of the FSE-based diffusion, PROPELLER DWI, with a voxel size of 2.0 x 2.0 x 2.0 mm.
B
Figure 5.
A 17-year-old male with a left cholesteatoma (arrow). (A) Axial fast recovery FSE sequence with a voxel size of 0.4 x 0.7 x 2.0 mm and (B) true coronal of the FSE-based diffusion, PROPELLER DWI, with a voxel size of 2.0 x 2.0 x 2.0 mm.
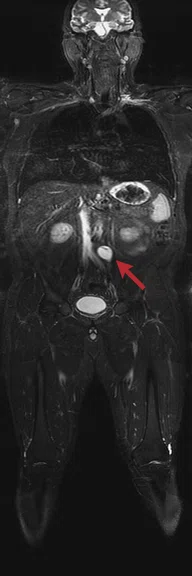
A
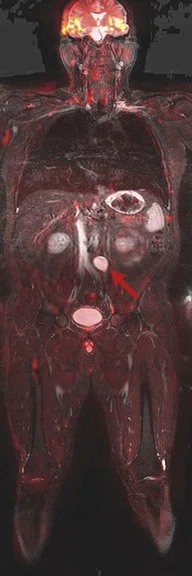
Figure 8.
Claustrophobic 39-year-old male with Li-Fraumeni syndrome. The patient had previous treatment for Burkitt lymphoma. Whole-body MR was performed with the Head/Neck Unit, AIR™ Coil and peripheral vascular MRA coil. A tumor is seen in the retroperitoneum (arrows). (A) DWI (b800 s/mm2) in a total scan time of 30 min.; (B) coronal IR-FSE with a total scan time of 15 min.; and (C) fused DWI and IR-FSE.
B
Figure 8.
Claustrophobic 39-year-old male with Li-Fraumeni syndrome. The patient had previous treatment for Burkitt lymphoma. Whole-body MR was performed with the Head/Neck Unit, AIR™ Coil and peripheral vascular MRA coil. A tumor is seen in the retroperitoneum (arrows). (A) DWI (b800 s/mm2) in a total scan time of 30 min.; (B) coronal IR-FSE with a total scan time of 15 min.; and (C) fused DWI and IR-FSE.
C
Figure 8.
Claustrophobic 39-year-old male with Li-Fraumeni syndrome. The patient had previous treatment for Burkitt lymphoma. Whole-body MR was performed with the Head/Neck Unit, AIR™ Coil and peripheral vascular MRA coil. A tumor is seen in the retroperitoneum (arrows). (A) DWI (b800 s/mm2) in a total scan time of 30 min.; (B) coronal IR-FSE with a total scan time of 15 min.; and (C) fused DWI and IR-FSE.
C
Figure 1.
Male patient with a hemangioma in segment 7 of the liver (arrow) 20 minutes after injection of a hepatospecific contrast agent. (A) Original breath-hold LAVA Flex protocol with a voxel size of 1.2 x 1.8 x 2.2 mm; (B) revised protocol with a voxel size of 1.4 x 1.4 x 1.4 mm; and (C, D) sagittal and coronal reformats of the isotropic 1.4 mm data.
D
Figure 1.
Male patient with a hemangioma in segment 7 of the liver (arrow) 20 minutes after injection of a hepatospecific contrast agent. (A) Original breath-hold LAVA Flex protocol with a voxel size of 1.2 x 1.8 x 2.2 mm; (B) revised protocol with a voxel size of 1.4 x 1.4 x 1.4 mm; and (C, D) sagittal and coronal reformats of the isotropic 1.4 mm data.
A
Figure 7.
A 33-year-old male with a large ulceration on his left forearm. The AIR™ Coil was wrapped around his forearm and elbow. (A) Coronal IR-FSE; (B) axial T1w FSE with a voxel size of 0.6 x 0.6 x 4.5 mm; and (C) axial IR-FSE with a voxel size of 0.7 x 0.6 x 4.5 mm. The images show a large ulcer on the dorsal aspect of the forearm. There is edema of the dorsal compartment of the forearm muscles and of the deep anterior muscles proximal of the elbow. There is high water sensitive signal within the ulna and radius. The images suggested reactive osteitis.
B
Figure 7.
A 33-year-old male with a large ulceration on his left forearm. The AIR™ Coil was wrapped around his forearm and elbow. (A) Coronal IR-FSE; (B) axial T1w FSE with a voxel size of 0.6 x 0.6 x 4.5 mm; and (C) axial IR-FSE with a voxel size of 0.7 x 0.6 x 4.5 mm. The images show a large ulcer on the dorsal aspect of the forearm. There is edema of the dorsal compartment of the forearm muscles and of the deep anterior muscles proximal of the elbow. There is high water sensitive signal within the ulna and radius. The images suggested reactive osteitis.
C
Figure 7.
A 33-year-old male with a large ulceration on his left forearm. The AIR™ Coil was wrapped around his forearm and elbow. (A) Coronal IR-FSE; (B) axial T1w FSE with a voxel size of 0.6 x 0.6 x 4.5 mm; and (C) axial IR-FSE with a voxel size of 0.7 x 0.6 x 4.5 mm. The images show a large ulcer on the dorsal aspect of the forearm. There is edema of the dorsal compartment of the forearm muscles and of the deep anterior muscles proximal of the elbow. There is high water sensitive signal within the ulna and radius. The images suggested reactive osteitis.
A
Figure 7.
A 33-year-old male with a large ulceration on his left forearm. The AIR™ Coil was wrapped around his forearm and elbow. (A) Coronal IR-FSE; (B) axial T1w FSE with a voxel size of 0.6 x 0.6 x 4.5 mm; and (C) axial IR-FSE with a voxel size of 0.7 x 0.6 x 4.5 mm. The images show a large ulcer on the dorsal aspect of the forearm. There is edema of the dorsal compartment of the forearm muscles and of the deep anterior muscles proximal of the elbow. There is high water sensitive signal within the ulna and radius. The images suggested reactive osteitis.
B
Figure 7.
A 33-year-old male with a large ulceration on his left forearm. The AIR™ Coil was wrapped around his forearm and elbow. (A) Coronal IR-FSE; (B) axial T1w FSE with a voxel size of 0.6 x 0.6 x 4.5 mm; and (C) axial IR-FSE with a voxel size of 0.7 x 0.6 x 4.5 mm. The images show a large ulcer on the dorsal aspect of the forearm. There is edema of the dorsal compartment of the forearm muscles and of the deep anterior muscles proximal of the elbow. There is high water sensitive signal within the ulna and radius. The images suggested reactive osteitis.
C
Figure 7.
A 33-year-old male with a large ulceration on his left forearm. The AIR™ Coil was wrapped around his forearm and elbow. (A) Coronal IR-FSE; (B) axial T1w FSE with a voxel size of 0.6 x 0.6 x 4.5 mm; and (C) axial IR-FSE with a voxel size of 0.7 x 0.6 x 4.5 mm. The images show a large ulcer on the dorsal aspect of the forearm. There is edema of the dorsal compartment of the forearm muscles and of the deep anterior muscles proximal of the elbow. There is high water sensitive signal within the ulna and radius. The images suggested reactive osteitis.
A
Figure 6.
A 64-year-old female post-surgery. (A) Patient’s right knee wrapped in the AIR™ Coil; (B) sagittal T2w FSE; and (C, D) axial T2w with a voxel size of 0.6 x 0.8 x 4 mm. There is edema in the subcutaneous fat and adjacent muscles in keeping with the surgical intervention and radiotherapy. No evidence of a mass lesion.
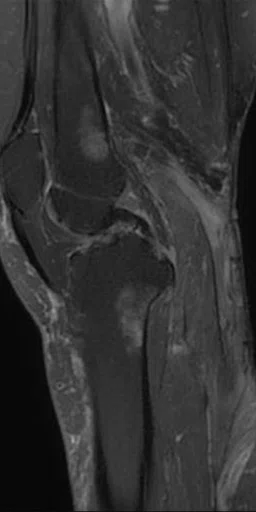
B
Figure 6.
A 64-year-old female post-surgery. (A) Patient’s right knee wrapped in the AIR™ Coil; (B) sagittal T2w FSE; and (C, D) axial T2w with a voxel size of 0.6 x 0.8 x 4 mm. There is edema in the subcutaneous fat and adjacent muscles in keeping with the surgical intervention and radiotherapy. No evidence of a mass lesion.
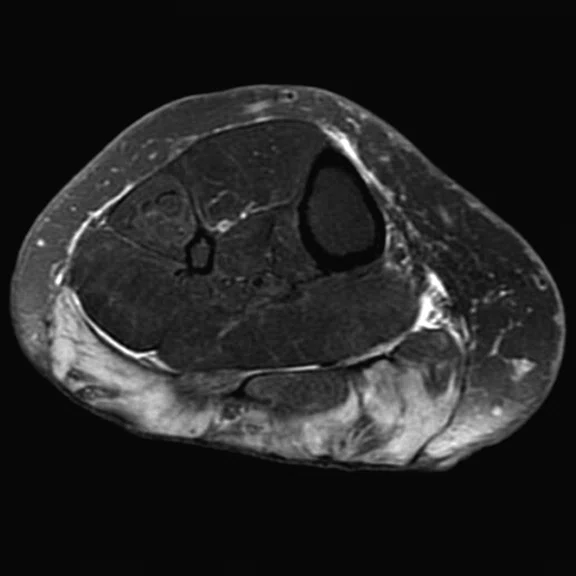
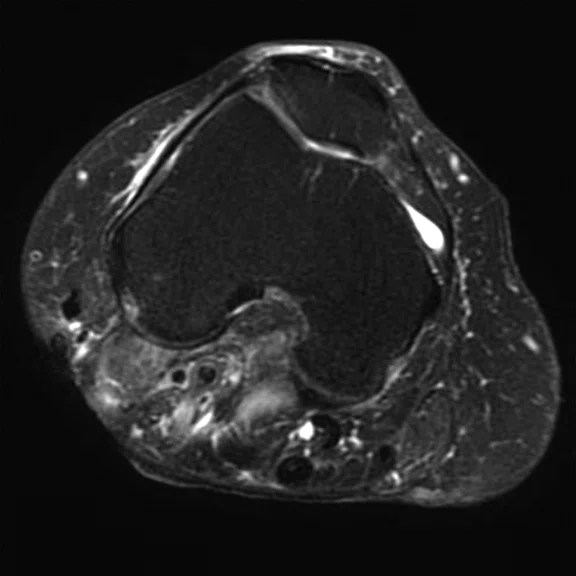
C
Figure 6.
A 64-year-old female post-surgery. (A) Patient’s right knee wrapped in the AIR™ Coil; (B) sagittal T2w FSE; and (C, D) axial T2w with a voxel size of 0.6 x 0.8 x 4 mm. There is edema in the subcutaneous fat and adjacent muscles in keeping with the surgical intervention and radiotherapy. No evidence of a mass lesion.
D
Figure 6.
A 64-year-old female post-surgery. (A) Patient’s right knee wrapped in the AIR™ Coil; (B) sagittal T2w FSE; and (C, D) axial T2w with a voxel size of 0.6 x 0.8 x 4 mm. There is edema in the subcutaneous fat and adjacent muscles in keeping with the surgical intervention and radiotherapy. No evidence of a mass lesion.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
IN PRACTICE
Cambridge experiences a breath of fresh AIR
Cambridge experiences a breath of fresh AIR
By Martin Graves, PhD, Consultant Clinical Scientist, and Rhys Slough, MSc, MRI Operations Manager, Cambridge University Hospitals, Addenbrooke’s Hospital, Cambridge, UK
Cambridge University Hospitals (CUH) recently chose to upgrade one of its Optima™ MR450w systems to the SIGNA™ Artist via the SIGNA™ Lift Program. This was a very time- and cost-effective means to ensure that Cambridge remains at the forefront of MR imaging technology. Clinical benefits are seen through improvements in image quality, particularly with more challenging patients. The improved RF chain, automated coil selection, reconstruction and new applications delivered with the SIGNA™Works software release in 2019 were the main clinical drivers, together with access to the latest AIR™ Coil technology.
Cambridge University Hospitals (CUH) recently chose to upgrade one of its Optima™ MR450w systems to the SIGNA™ Artist via the SIGNA™ Lift Program. This was a very time- and cost-effective means to ensure that Cambridge remains at the forefront of MR imaging technology. Clinical benefits are seen through improvements in image quality, particularly with more challenging patients. The improved RF chain, automated coil selection, reconstruction and new applications delivered with the SIGNA™Works software release in 2019 were the main clinical drivers, together with access to the latest AIR™ Coil technology.
SIGNA™ Artist is a clinical workhorse used for a wide range of examinations including neuro, cardiovascular, musculoskeletal, breast and abdominal imaging. We were impressed with the notable improvement in image quality from the outset with the hardware upgrade. For example, we were previously using a breath-hold LAVA Flex with a slice thickness of 4.4 mm for our 20-minute delayed phase hepatospecific contrast agent imaging. Using SIGNA™ Artist, we were able to obtain high-quality images with a slice thickness of 2.8 mm, interpolated to 1.4 mm in approximately the same 15-second breath hold. This allowed us to perform high-quality reformats of the near isotropic volumetric data (Figure 1). While LAVA Flex is still our gold-standard method for contrast enhanced liver imaging, we have found that when imaging difficult patients who struggle to hold their breath, the use of the free-breathing (navigated) DISCO LAVA with SPECIAL fat suppression reduced the acquisition time to around 16 seconds for each of the arterial, venous and equilibrium phases (Figure 2). Previously, without DISCO LAVA, it would not have been possible to obtain diagnostic-quality images.
Figure 1.
Male patient with a hemangioma in segment 7 of the liver (arrow) 20 minutes after injection of a hepatospecific contrast agent. (A) Original breath-hold LAVA Flex protocol with a voxel size of 1.2 x 1.8 x 2.2 mm; (B) revised protocol with a voxel size of 1.4 x 1.4 x 1.4 mm; and (C, D) sagittal and coronal reformats of the isotropic 1.4 mm data.
Figure 2.
A 75-year-old male with a gastric tumor (red arrow) and large liver metastases (yellow arrow). (A) Axial navigated PROPELLER T2w FatSat with a voxel size of 1.4 x 1.4 x 6 mm; (B) axial navigated DWI with b600 s/mm2 and voxel size of 5 x 3.1 x 6 mm; and (C, D) two axial slices from the delayed phase free-breathing (navigated) DISCO LAVA with a voxel size of 1.6 x 2.1 x 2.2 mm.
The MUSE sequence has been particularly well-received by our breast radiologists who appreciate the improved spatial resolution and reduced distortion achievable with this multi-shot technique (Figure 3). Our gynecological radiologists have similarly been impressed by the quality of the MUSE images in the pelvis (Figure 4).
C
D
Figure 3.
Patient referred for breast cancer staging. (A) Axial DWI with b800 s/mm2 using our original protocol with a voxel size of 3.7 x 2.8 x 3.5 mm; (B) axial slice acquired using a 2-shot MUSE acquisition with a voxel size of 2.2 x 2.2 x 3.5 mm; (C) coronal reformat of the axial DWI data acquired in 6 min.; and (D) coronal reformat of the 2-shot MUSE data acquired in 9 min.
Cholesteatoma imaging was previously impossible using standard echo planar DWI. The use of diffusion-weighted PROPELLER substantially improved the image quality, but we were limited by the inability to acquire images in the coronal plane.
With the SIGNA™ Artist, we now have access to the improved PROPELLER DWI sequence, which is compatible with all imaging planes.
Figure 5 shows the superb image quality achievable in the coronal plane. The ability to combine the sequence with spatial saturation bands, a Flexible No Phase Wrap option and the ability to achieve a 2 mm slice thickness also contributes to the outstanding image quality.
While the SIGNA™ Artist upgrade together with the SIGNA™Works software upgrade has driven the improvements in image quality, we were particularly excited about receiving one of the first AIR™ Anterior Array (AA) Coils. We were not disappointed. From the moment the coil was removed from its shipping box we could see the potential. Over the years we have used so-called "flexible" coils and we came to accept the limitations of the concept of flexibility in this context.
However, once you handle an AIR™ Coil you really understand that flexible means flexible and not some semi-rigid pseudo-interpretation.
So, while it delivered on all its ergonomic promises, what did the patients think and what was the image quality like?
The first question can be most dramatically answered by two of our patients scanned using the AIR™ AA Coil shortly after delivery. The first was a woman who had recently had chest surgery. She had an MR examination prior to surgery with a standard torso array coil. When she arrived, she was extremely anxious about the scan, as her chest was very sensitive. When she was positioned using the AIR™ AA Coil, her relief was obvious. She completed the examination without complaint. The second patient was a 64-year-old woman who had a sarcoma surgically removed from the posterior aspect of her right knee. Her surgical team requested an MR to assess her right knee post-surgery and radiotherapy.
The posterior aspect of her right knee was very painful and she was very worried about placing her knee in our hard shell 8-channel transmit/receive knee coil. Our large 16-channel GEM Flex Coil didn’t cover the surgical area. The radiographer decided to try wrapping the AIR™ AA Coil around her knee (Figure 6A). The patient completed the exam without pain and, therefore, without moving (Figure 6). After the exam she said, "The [AIR™] coil was very comfortable; it was like wrapping a blanket around my knee. I found this exam to be a better experience than my previous MRI." Note in Figure 6 that the image quality is not visually compromised by the coil having been wrapped tightly around the leg and there are no observable interactions between the coil elements, despite some of them being overlapped.
Figure 6.
A 64-year-old female post-surgery. (A) Patient’s right knee wrapped in the AIR™ Coil; (B) sagittal T2w FSE; and (C, D) axial T2w with a voxel size of 0.6 x 0.8 x 4 mm. There is edema in the subcutaneous fat and adjacent muscles in keeping with the surgical intervention and radiotherapy. No evidence of a mass lesion.
The AIR™ AA Coil also proved invaluable in scanning another patient who was a former drug addict with a large ulceration on his left forearm around his previous injection sites. Unfortunately, due to his history he had very restricted movement of his forearm. He was successfully scanned with his arm positioned across his abdomen and the AIR™ AA Coil wrapped around his forearm and elbow (Figure 7).
Figure 7.
A 33-year-old male with a large ulceration on his left forearm. The AIR™ Coil was wrapped around his forearm and elbow. (A) Coronal IR-FSE; (B) axial T1w FSE with a voxel size of 0.6 x 0.6 x 4.5 mm; and (C) axial IR-FSE with a voxel size of 0.7 x 0.6 x 4.5 mm. The images show a large ulcer on the dorsal aspect of the forearm. There is edema of the dorsal compartment of the forearm muscles and of the deep anterior muscles proximal of the elbow. There is high water sensitive signal within the ulna and radius. The images suggested reactive osteitis.
Figure 7.
A 33-year-old male with a large ulceration on his left forearm. The AIR™ Coil was wrapped around his forearm and elbow. (A) Coronal IR-FSE; (B) axial T1w FSE with a voxel size of 0.6 x 0.6 x 4.5 mm; and (C) axial IR-FSE with a voxel size of 0.7 x 0.6 x 4.5 mm. The images show a large ulcer on the dorsal aspect of the forearm. There is edema of the dorsal compartment of the forearm muscles and of the deep anterior muscles proximal of the elbow. There is high water sensitive signal within the ulna and radius. The images suggested reactive osteitis.
The AIR™ AA Coil has now become our preferred coil for all thoracic and abdominal imaging, and we are just starting to explore its application in other areas, such as whole-body imaging (Figure 8).
Figure 8.
Claustrophobic 39-year-old male with Li-Fraumeni syndrome. The patient had previous treatment for Burkitt lymphoma. Whole-body MR was performed with the Head/Neck Unit, AIR™ Coil and peripheral vascular MRA coil. A tumor is seen in the retroperitoneum (arrows). (A) DWI (b800 s/mm2) in a total scan time of 30 min.; (B) coronal IR-FSE with a total scan time of 15 min.; and (C) fused DWI and IR-FSE.
Two significant advances have simplified workflow and enhanced the user experience. First, AIR Touch™ – a new workflow application that automates coil selection and landmarking – is simple, easy to use and allows a seamless workflow when using multiple coils. The coil icons allow for easy identification of the coil and, as soon as we start scanning, the most appropriate coil for the field-of-view is automatically selected. Secondly, the integration of the calibration scan within the individual sequence prescan (where necessary) also makes the workflow substantially less user intensive.
Overall, we are reaping the benefits of the trinity of SIGNA™ Artist, SIGNA™Works and AIR™ Coils. The combination of the new pulse sequences together with the unique flexibility of the AIR™ Coil, both in terms of applications as well as physical characteristics, makes this the most advanced platform within our installed base. We are now planning to upgrade all of our other Optima™ MR450w systems so that we can provide an equal operator and patient experience and ensure that all our radiologists are provided with the highest quality images.
Acknowledgements
We gratefully acknowledge the support of all the CUH radiographers and radiologists, as well as our GE Healthcare colleagues, Simon Dezonie, UK Clinical Zone Leader, and Dr. Gavin Houston, Clinical Scientist.