A
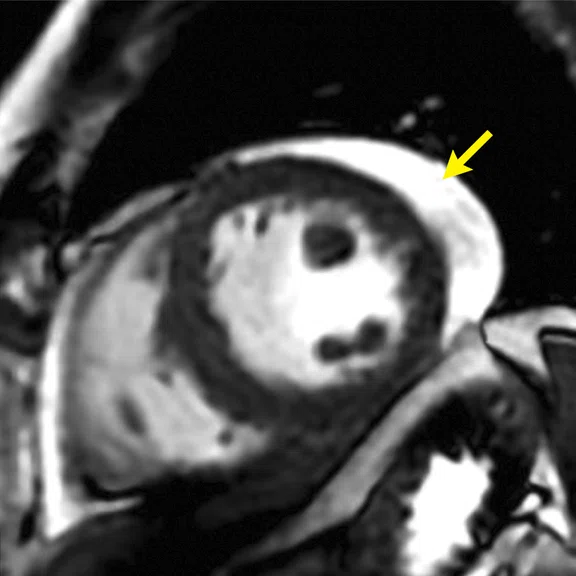
Figure 1.
CMR findings in short axis views of a patient with COVID-19-related acute myocarditis. (A) Cine image with pericardial effusion (arrow); (B) late enhancement (MDE) image with mild patchy inflammatory necrosis (arrows); (C) T2 map showing increased T2 values (in red) for the entire LV myocardium, consistent with widespread myocardial edema. The LV volume was small and the resulting cardiac output reduced, despite tachycardia.
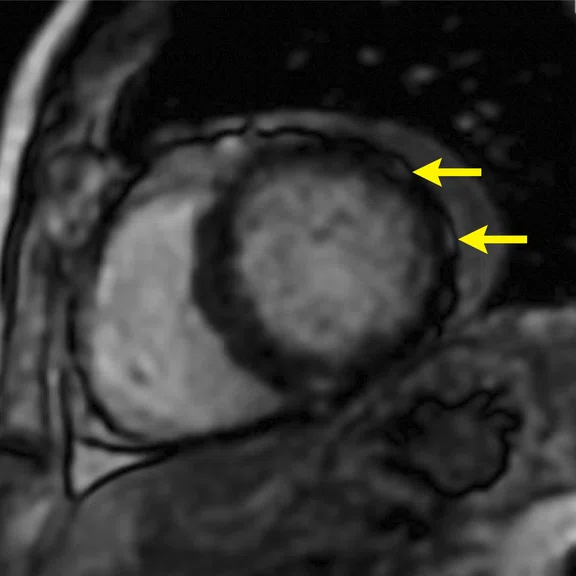
B
Figure 1.
CMR findings in short axis views of a patient with COVID-19-related acute myocarditis. (A) Cine image with pericardial effusion (arrow); (B) late enhancement (MDE) image with mild patchy inflammatory necrosis (arrows); (C) T2 map showing increased T2 values (in red) for the entire LV myocardium, consistent with widespread myocardial edema. The LV volume was small and the resulting cardiac output reduced, despite tachycardia.
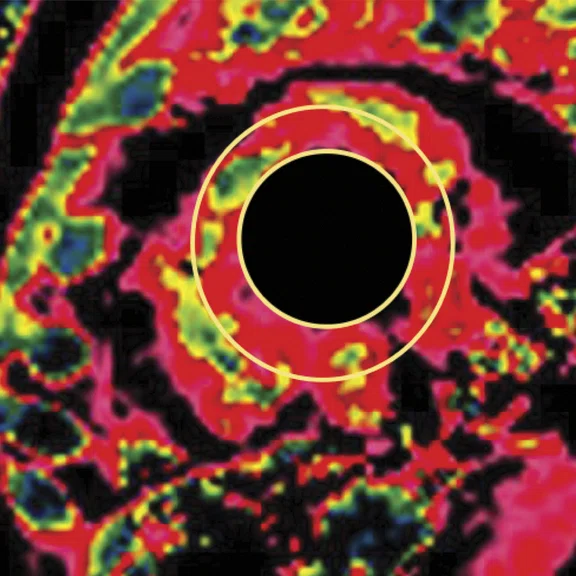
C
Figure 1.
CMR findings in short axis views of a patient with COVID-19-related acute myocarditis. (A) Cine image with pericardial effusion (arrow); (B) late enhancement (MDE) image with mild patchy inflammatory necrosis (arrows); (C) T2 map showing increased T2 values (in red) for the entire LV myocardium, consistent with widespread myocardial edema. The LV volume was small and the resulting cardiac output reduced, despite tachycardia.
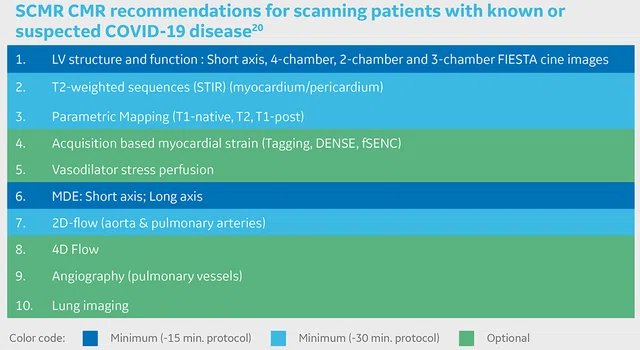
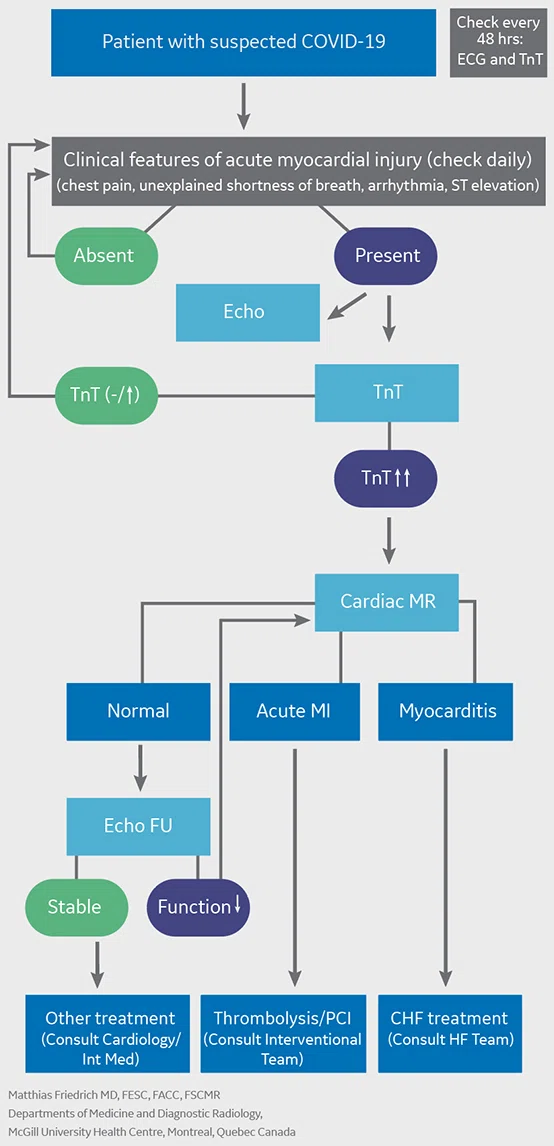
Figure 2.
SCMR has published recommendations for the clinical application of CMR during the COVID pandemic. In patients with suspected cardiac complications due to COVID-19, the recommendations are to perform a core CMR protocol focused on function and tissue characteristics.
Figure 3.
Suggested role of CMR during the COVID-19 pandemic.
1. European mortality monitoring activity (EuroMOMO). Available at: www.euromomo.eu.
2. Coronavirus tracked: the latest figures as countries fight to contain the pandemic. Financial Times. Available at: www.ft.com/coronavirus-latest.
3. Katz J, Sanger-Katz M. Deaths in New York City Are More Than Double the Usual Total. The New York Times. April 10, 2020. Available at: https://www.nytimes.com/interactive/2020/04/10/upshot/coronavirus-deaths-new-york-city.html.
4. Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417-1418. doi:10.1016/S0140-6736(20)30937-5.
5. Akhmerov A, Marbán E. COVID-19 and the Heart. Circ Res. 2020;126(10):1443-1455. doi:10.1161/CIRCRESAHA.120.317055.
5. Akhmerov A, Marbán E. COVID-19 and the Heart. Circ Res. 2020;126(10):1443-1455. doi:10.1161/CIRCRESAHA.120.317055.
6. Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) [published online March 27, 2020]. JAMA Cardiol. 2020. doi: 10.1001/jamacardio.2020.1017.
6. Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) [published online March 27, 2020]. JAMA Cardiol. 2020. doi: 10.1001/jamacardio.2020.1017.
7. Mahmud E, Dauerman HL Frederick GP, et al. Management of Acute Myocardial Infarction During the COVID-19 Pandemic. J Am Coll Cardiol. 2020 Apr 30. Epublished DOI:10.1016/j.jacc.2020.04.039.
8. Fried JA, Ramasubbu K, Bhatt R, et al. The Variety of Cardiovascular Presentations of COVID-19 [published online ahead of print, 2020 Apr 3]. Circulation. 2020;10.1161/CIRCULATIONAHA.120.047164. doi:10.1161/CIRCULATIONAHA.120.047164
9. Inciardi RM, Lupi L, Zaccone G, et al. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19) [published online ahead of print, 2020 Mar 27]. JAMA Cardiol. 2020;10.1001/jamacardio.2020.1096. doi:10.1001/jamacardio.2020.1096
10. Luetkens JA, Isaak A, Zimmer S, Nattermann J, Sprinkart AM, Boesecke C, Rieke GJ, Zachoval C, Heine A, Velten M, Duerr GD. Diffuse Myocardial Inflammation in COVID-19 Associated Myocarditis Detected by Multiparametric Cardiac Magnetic Resonance Imaging. Circ Cardiovasc Imaging 2020;13:e010897.
11. Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. Published online July 27, 2020. doi:10.1001/jamacardio.2020.3557
12. Sanz J. Evolving diagnostic and prognostic imaging of the various cardiomyopathies. Ann N Y Acad Sci. 2012;1254:123-130. doi:10.1111/j.1749-6632.2012.06490.x
13. Cummings KW, Bhalla S, Javidan-Nejad C, Bierhals AJ, Gutierrez FR, Woodard PK. A pattern-based approach to assessment of delayed enhancement in nonischemic cardiomyopathy at MR imaging. Radiographics. 2009;29(1):89-103. doi:10.1148/rg.291085052
14. Friedrich MG, Sechtem U, Schulz-Menger J, et al. Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J Am Coll Cardiol. 2009;53(17):1475-1487. doi:10.1016/j.jacc.2009.02.007.
15. Ferreira VM, Schulz-Menger J, Holmvang G, et al. Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation: Expert Recommendations. J Am Coll Cardiol. 2018;72(24):3158-3176. doi:10.1016/j.jacc.2018.09.072.
16. World Health Organization. Coronavirus disease (COVID-19) advice for the public. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
17. Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Social Distancing. Available at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html.
18. Moschetti K, Favre D, Pinget C, Pilz G, Petersen SE, Wagner A, Wasserfallen JB, Schwitter JJ. Comparative cost-effectiveness analyses of cardiovascular magnetic resonance and coronary angiography combined with fractional flow reserve for the diagnosis of coronary artery disease. J Cardiovasc Magn Reson 2014;16:13.
19. Han Y, Chen T, Bryant J, et al. Society for Cardiovascular Magnetic Resonance (SCMR) guidance for the practice of cardiovascular magnetic resonance during the COVID-19 pandemic. J Cardiovasc Magn Reson. 2020;22(1):26. Published 2020 Apr 27. doi:10.1186/s12968-020-00628-w.
20. Kelle S, Bucciarelli-Ducci C, Judd RM, et al. Society for Cardiovascular Magnetic Resonance (SCMR) recommended CMR protocols for scanning patients with active or convalescent phase COVID-19 infection. J Cardiovasc Magn Reson 22, 61 (2020). https://doi.org/10.1186/s12968-020-00656-6.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
SPOTLIGHT
Cardiac MR in times of COVID-19
Cardiac MR in times of COVID-19
by Matthias G. Friedrich, MD, FESC, FACC, MSCMR, Professor of Medicine and Diagnostic Radiology McGill University Health Centre, Montreal, Quebec, Canada
Coronavirus (COVID-19) is a disease caused by a novel virus, SARS-CoV-2, where SARS stands for severe acute respiratory syndrome. Although this is not the first variant of a coronavirus – both SARS and MERS were prior coronaviruses that underwent animal-to-human transition – COVID-19 does appear to be more contagious than its predecessors or the typical influenza virus.
Coronavirus (COVID-19) is a disease caused by a novel virus, SARS-CoV-2, where SARS stands for severe acute respiratory syndrome. Although this is not the first variant of a coronavirus – both SARS and MERS were prior coronaviruses that underwent animal-to-human transition – COVID-19 does appear to be more contagious than its predecessors or the typical influenza virus.
Many people infected with COVID-19 are asymptomatic. However, certain populations are at a substantially higher risk, including the elderly (over 65 years old) and those with immunosuppression and pre-existing lung and cardiovascular disease1. Obesity also appears to be a particularly strong risk factor.
Historically, in terms of deaths, there have been larger pandemics, including the 40-50 million people who died from the Spanish flu of 1918-1919 and the ongoing AIDS/HIV epidemic that has killed up to 35 million people since 1981. We don’t yet know the full impact COVID-19 will have on our society, economy and healthcare. The brutality of how the pandemic flooded certain countries led to partial collapses of regional healthcare systems. This is why it is important to think about how to address this pandemic. Countries such as Australia, Austria, South Korea and Norway that responded very quickly with lockdowns to reduce the spread of the virus did better in terms of overall death rates2. It appears, for the time being, that earlier restrictions had a positive impact on community spread and mortality, while a final evaluation of different strategies will not be possible for at least another year.
During the ongoing pandemic, people are also dying from other causes because they either are afraid of going to emergency rooms or because some hospitals are overwhelmed with COVID-19 patients. In New York City, a severely affected region, there are excess deaths not attributed to COVID-19, including patients who are waiting for urgent interventions they cannot receive3. Furthermore, the pandemic is already having a significant impact on the US economy, leading to an unprecedented spike in unemployment and downstream effects that will affect society for several years.
COVID-19 impact on the cardiovascular system
The SARS-CoV-2 virus enters the body’s cells through the angiotensin converting enzyme 2 (ACE2) receptor that is involved in regulating blood pressure and the vascular permeability, and that is especially prevalent in the lungs and heart. After an incubation period of four to six days, typical symptoms such as sore throat, dry cough, fever, myalgia and loss of smell and/or taste occur. Not all COVID-19-positive patients will experience each of these symptoms, whereas fever, cough and a sore throat are frequent.
The first symptom of severe disease, often four to six days after the first clinical signs, is dyspnea (shortness of breath). COVID-19 can lead to extensive necrotic inflammation in the lungs, associated with a poor prognosis. Recent findings suggest that SARSCoV-2 infection causes endotheliitis in several organs that may cause a massive inflammatory response leading to local formation of blood clots4. Resulting pulmonary embolism may explain why people with COVID-19 experience a sudden deterioration of their respiratory function. Another aspect of this virus is the potential for increased permeability of the blood vessels through the ACE2 receptor, leading to an escalation in edema.
This very strong response by the immune system has also been called the cytokine storm and it may initiate more damage than the virus itself, causing some of the young COVID-19 patients to be severely affected.
The disease progresses in three pathological stages: infection, pulmonary phase and severe disease caused by hyperinflammation5. In the first phase, viral infiltration and replication occurs with lymphocytopenia, a key laboratory finding. As the disease advances to the pulmonary phase, patients experience respiratory compromise and abnormal chest imaging. In the third and most severe phase, massive inflammation typically leads to extensive pulmonary damage with a subsequent lack of oxygen and finally multiorgan failure5.
A high incidence of acute myocardial injury, likely around 20 percent, is associated with poor prognosis and therefore a potential target for aggressive treatment6. According to early reports, up to 50 percent of COVID-19 patients with acute myocardial injury may die6.
Elevated biomarkers such as troponin and clinical symptoms including arrhythmia, palpitations, heart failure and sudden death indicate acute myocardial injury. Acute coronary syndrome involving the coronary arteries can lead to ischemic injury or an ischemic event, such as myocardial infarction.
A consensus paper from the Society for Cardiovascular Angiography and Interventions (SCAI), American College of Cardiology (ACC) and the American College of Emergency Physicians (ACEP) recommends additional non-invasive evaluation in patients with an unclear or unequivocal diagnosis. Potential causes for myocardial injury can be ST-elevation myocardial infarction (STEMI), viral invasion itself, the inflammatory response of an overly active immune system or a mismatch systemic of oxygen supply and demand7. Therefore, if there is evidence of myocardial injury without a known etiology, more information is needed for informed clinical decision-making. Among various non-invasive diagnostic procedures, cardiac MR (CMR) has a unique potential.
Using CMR in COVID-19
CMR imaging enables the visualization of anatomy, function and tissue pathology. Reports on myocardial injury in patients with COVID-19 are still scarce, with one case of ischemic injury with involvement of a coronary artery8, and another with acute myocardial injury that was apparently caused by a direct inflammatory response and not an underlying coronary artery issue. In the latter case, T2 maps (from CMR) depicted evidence of pericardial effusion in the pericardial sac. In the short axis view of the left ventricle, there was evidence of myocardial edema, as indicated by increased T2 times of the more apical myocardium as well as the bright area indicative of increased water content consistent with myocardial edema as depicted in a PS MDE sequence in a four-chamber view9. A recent case report confirmed this pattern10. Additionally, a recent study indicated a substantial incidence of persisting myocardial edema in patients having recovered from COVID-1911. If confirmed, these results may suggest a significant role of CMR in the care of patients with persisting symptoms after a COVID infection.
Because of its versatility, CMR is the technique of choice for a comprehensive assessment of the heart, specifically with respect to visualizing tissue pathology and thus specifically verifying or refuting the underlaying cause of cardiac disease. It can help identify ischemic versus non-ischemic injury, where ischemic injury always involves the subendocardial layer while non-ischemic rarely does12. Regional distribution of the injury also indicates ischemic or non-ischemic injury; there are certain patterns that most often provide specific additional information on the origin of the injury13, such as cardiomyopathies or certain infiltrative diseases.
Figure 1 shows a case of acute myocardial inflammation in a patient with COVID-19.
Except for very few diseases – sarcoid and myocarditis – the underlying cause of myocardial injury can generally be identified by the regional distribution.
Figure 1.
CMR findings in short axis views of a patient with COVID-19-related acute myocarditis. (A) Cine image with pericardial effusion (arrow); (B) late enhancement (MDE) image with mild patchy inflammatory necrosis (arrows); (C) T2 map showing increased T2 values (in red) for the entire LV myocardium, consistent with widespread myocardial edema. The LV volume was small and the resulting cardiac output reduced, despite tachycardia.
Among them, myocarditis (inflammation of the heart muscle) can be identified quite specifically with CMR using a combination of CMR "sequences" (protocol components), including mapping, cine imaging and late enhancement (MDE).
MDE imaging requires the administration of a contrast agent and can detect irreversible myocardial injury such as necrosis, infiltration or fibrosis/scars. The Lake Louise Criteria for the assessment of patients with suspected myocardial inflammation provides CMR protocol standards and diagnostic criteria for identifying myocarditis14. There are main criteria for edema/acute inflammation (based on T2 as a water-sensitive marker that can be measured in CMR images) and irreversible myocardial injury in a nonischemic regional distribution pattern. Supportive criteria include pericardial effusion and systolic left ventricular dysfunction15.
Safety of CMR in COVID-19 patients
CMR is considered the non-invasive gold standard for verifying or refuting a diagnosis of acute myocarditis. In COVID-19 patients, it’s not just the accuracy of the technique, it’s also keeping the healthcare staff safe. The virus is transmitted through the endothelium, particularly the mouth, nose and eyes. Transmission occurs through droplets and contaminated surfaces. Longer distance aerosol transmission of 1 to 2 meters is possible if enough of the virus droplets are in the air and 6 to 8 meters around infected persons who are sneezing and coughing. The World Health Organization recommends at least 3 feet and the Centers for Disease Control and Prevention suggests 6 feet for safe social distancing16, 17.
It seems apparent that many of the countries with severe sudden outbreaks of COVID-19 are the result of mass gatherings that served as a catalyst for rapid spreading: a mass religious gathering in South Korea, carnival in Germany, and beach parties in Italy and Florida. Therefore, if the healthcare staff has to work in a confined space without sufficient air filtering, the high risk is quite obvious.
While an MR exam does not generate the same risk for patient aerosols that intubation or resuscitation do, there is the risk that all patients can be carriers, even those who are asymptomatic or have a negative test.
Therefore, during a pandemic, all patients should be considered as potential virus carriers. Accordingly, all staff members associated with the scan should have proper training in donning and doffing, as well as sufficient personal protective equipment (PPE).
Given the increased risk, surgical masks are not sufficient to efficiently protect the healthcare worker. Therefore, N95/FFP2 masks, face shields or protective glasses, gloves and an impermeable gown should be used in the presence of COVID-19 positive patients.
There are a few additional important considerations. A focused CMR protocol that reduces the time a patient is in the scanner should be utilized to reduce the risk of droplets in the scanner bore. Non-contrast scans that don’t require an IV should be used when possible to avoid close contact with the patient and the risk of droplets. After the scan, it is important to carefully clean all surfaces that have been potentially contaminated, similar to the extended cleaning protocols that exist in many facilities with critically ill or intubated patients. Leaving the scanner room empty for 30 minutes after an exam allows for proper ventilation.
Clinical MR workflow
COVID-19 patients with a clinical suspicion of acute myocardial injury should be frequently (every 24 to 48 hours) checked for ST elevation in ECG, shortness of breath not otherwise explained, arrhythmia or atypical chest pain. Troponin, a sensitive serologic marker, should be measured in all patients with suspected acute myocardial injury. If troponin is elevated, a cardiac MR scan can differentiate normal from acute nonischemic injury. Furthermore, it can also differentiate between numerous nonischemic myocardial diseases.
CMR has been shown to have a strong impact on clinical decision making, such as whether the patient goes to cardiac catheterization or receives aggressive heart failure treatment, and, therefore, also on patient outcomes18.
If the heart appears relatively normal on CMR, then further diagnostic testing for other underlying causes, e.g., lung injury, is warranted. In late April, the Society for Cardiac Magnetic Resonance (SCMR) published recommendations for the use of CMR during the COVID-19 pandemic19. The authors recommended standard or rapid CMR protocols for these patients based on clinical indication. The SCMR continued to lead on this important topic by releasing guidance on CMR protocols for scanning active or convalescent COVID-19 infected patients in early September20. Today, there is a greater understanding that, even in patients who have recovered from the symptoms of this novel coronavirus, there may be lasting impact on the heart and lungs. This is an area of further study.
One additional important aspect regarding the use of MR in COVID-19 patients is that it can be used to examine other organs. In an unpublished case report of a patient in Iran undergoing an MR for breast disease, pulmonary findings consistent with COVID-19 were detected. Peripheral inflammation in the right lung was depicted in the T2-weighted images. The patient subsequently tested positive and developed moderate symptoms. This case indicates that in one scan, MR could double rule-out both pulmonary and cardiac involvement without the use of contrast. Although CT angiography has a higher spatial resolution, this case illustrates that with a cardiac MR scan the clinician can examine both the lungs and the heart and avoid a separate CT scan, avoid another transport through the hospital and possibly save precious therapeutic decision-making time.
To summarize, CMR can play a critically important role in the workup of COVID-19 patients with signs of acute myocardial injury. Further, it can be combined with T2-weighted lung sequences as a double rule-out of myocardial and pulmonary injury and thus render CMR the role of a fast, highly efficient exam in all patients with suspected COVID-19. The safety of technologists should be ensured by proper training and availability of adequate PPE.