A
Figure 1.
Comparison of (A) STIR FSE and (B) STIR PROPELLER using SCENIC and AIR™ Recon, demonstrating significant artifact A B reduction in (B).
B
Figure 1.
Comparison of (A) STIR FSE and (B) STIR PROPELLER using SCENIC and AIR™ Recon, demonstrating significant artifact A B reduction in (B).
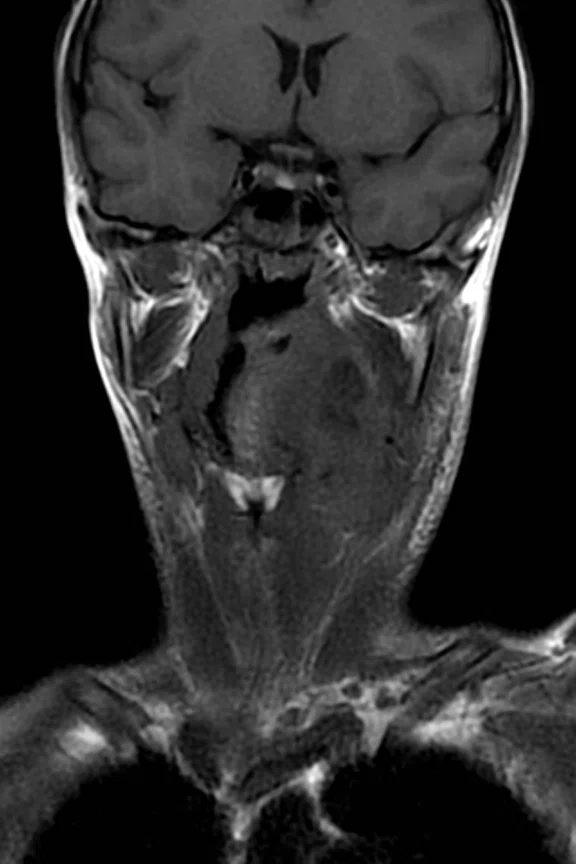
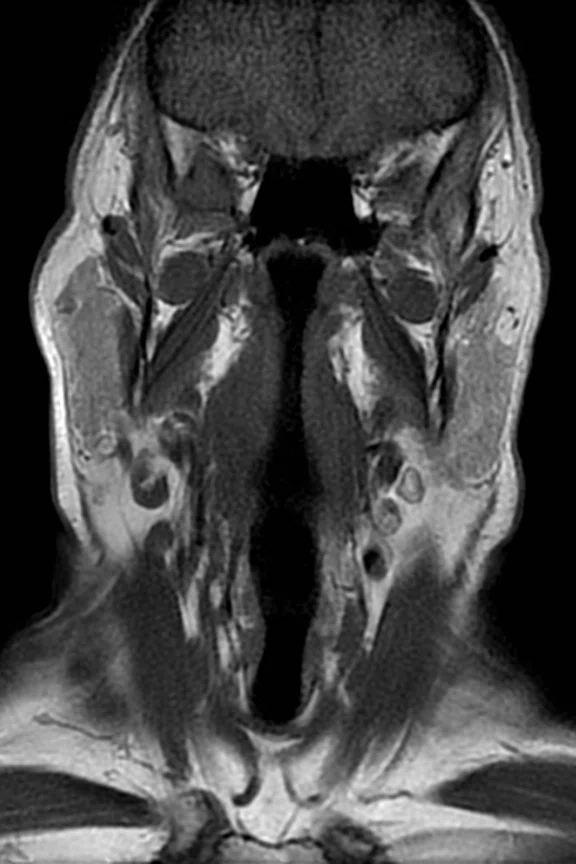
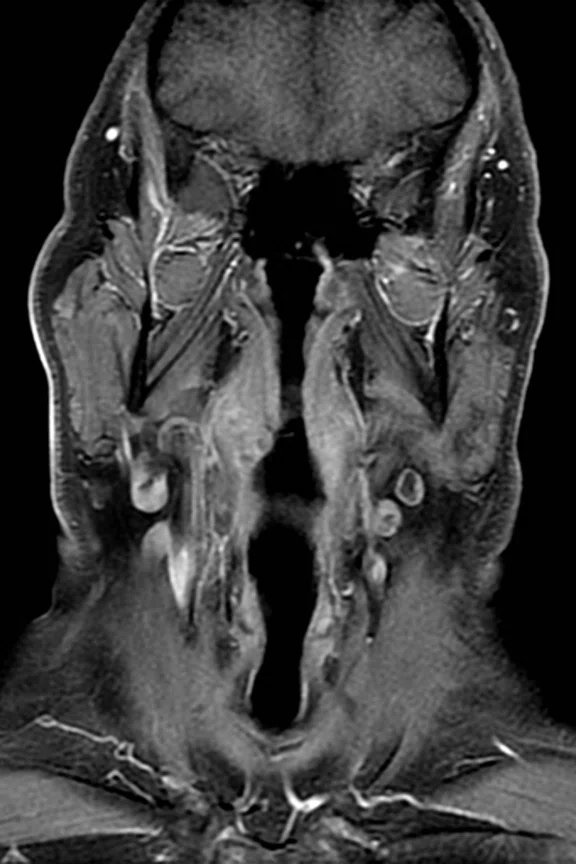
A
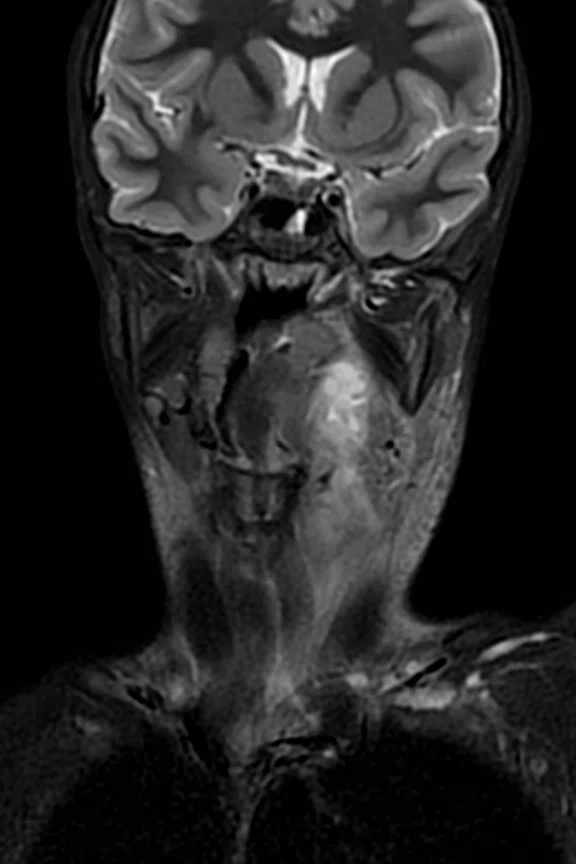
Figure 2.
(A) Coronal STIR PROPELLER, 3:21 min., (B) coronal T1 PROPELLER, 3:16 min and (C) coronal T1 FSE Flex with contrast, 3:36 min.
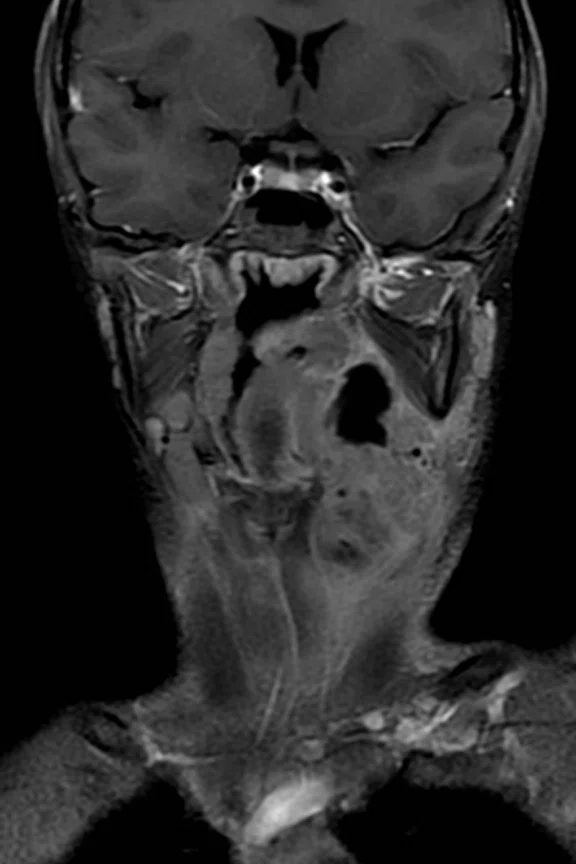
B
Figure 2.
(A) Coronal STIR PROPELLER, 3:21 min., (B) coronal T1 PROPELLER, 3:16 min and (C) coronal T1 FSE Flex with contrast, 3:36 min.
C
Figure 2.
(A) Coronal STIR PROPELLER, 3:21 min., (B) coronal T1 PROPELLER, 3:16 min and (C) coronal T1 FSE Flex with contrast, 3:36 min.
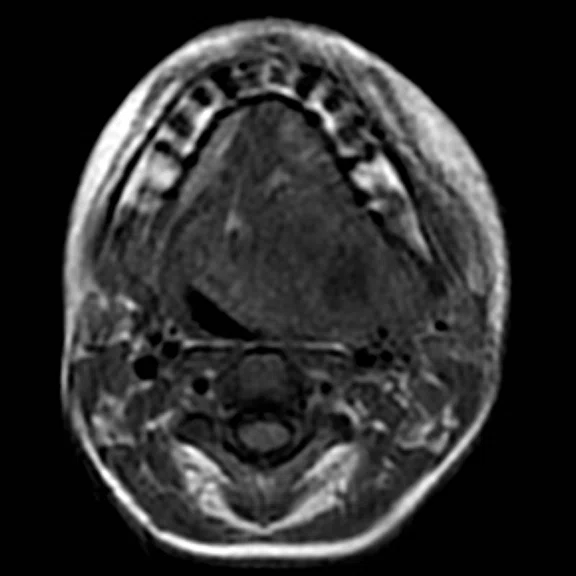
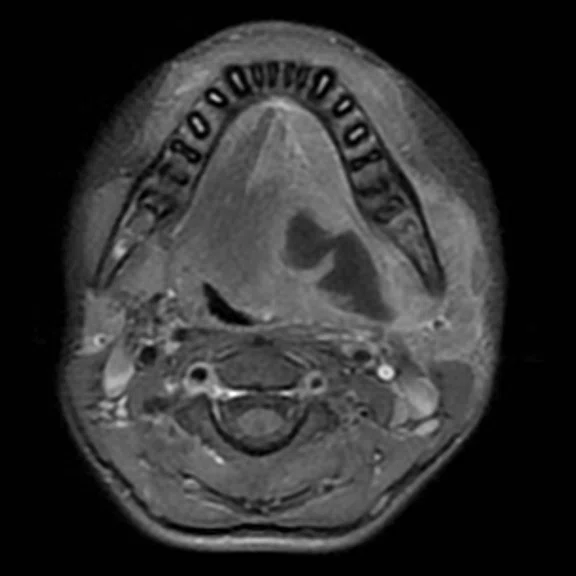
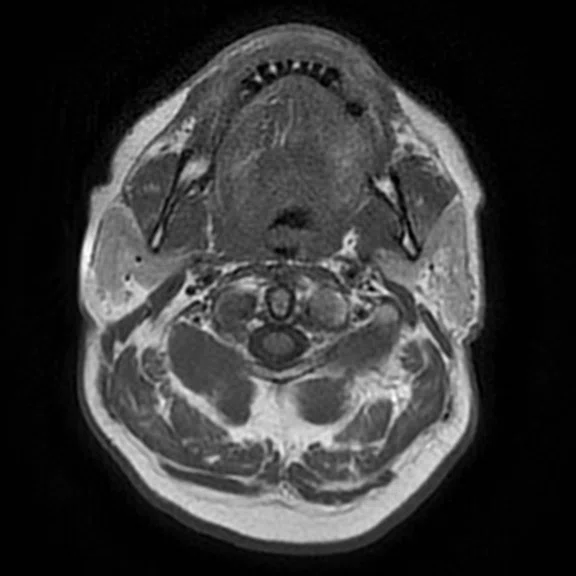
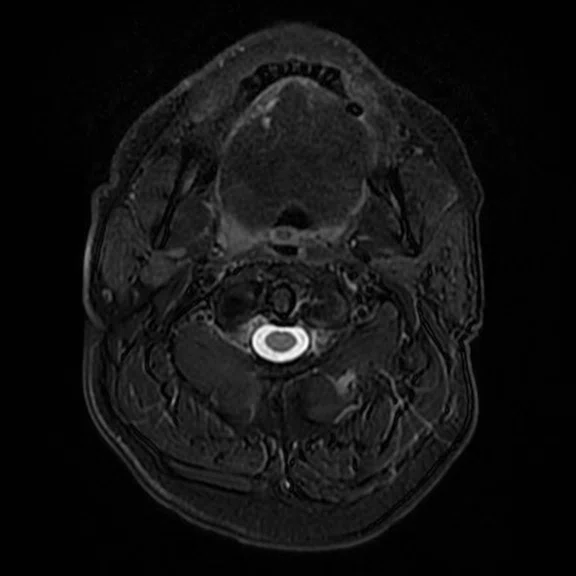
A
Figure 3.
(A) Axial T1 PROPELLER, 3:16 min., (B) axial T2 FSE Flex, 3:17 min., (C) axial T1 FSE Flex with contrast, 2:46 min. and (D) axial LAVA Flex with contrast, 2:00 min.
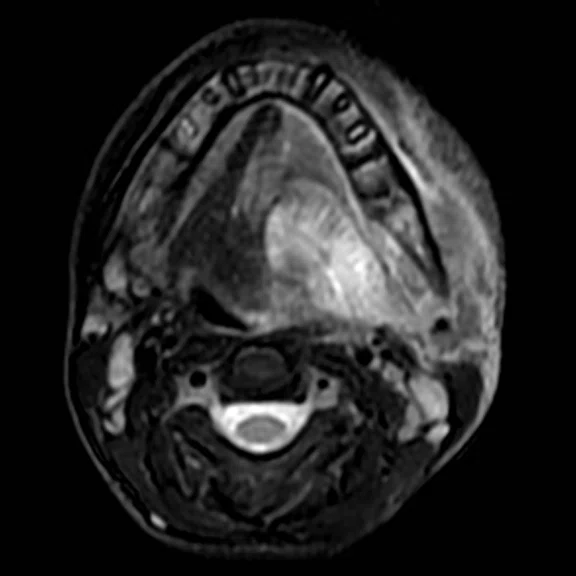
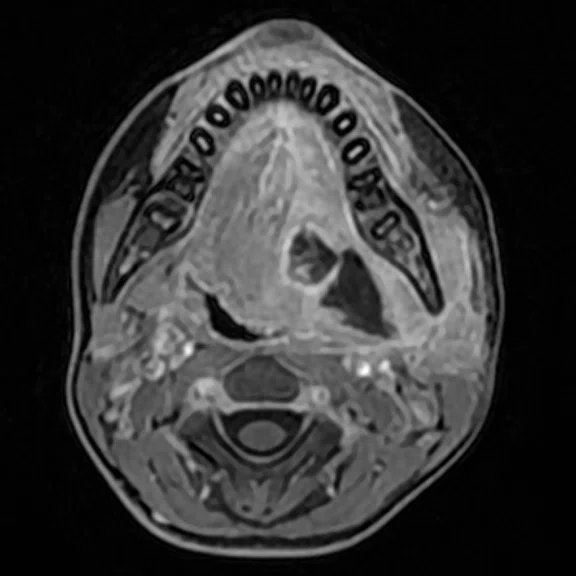
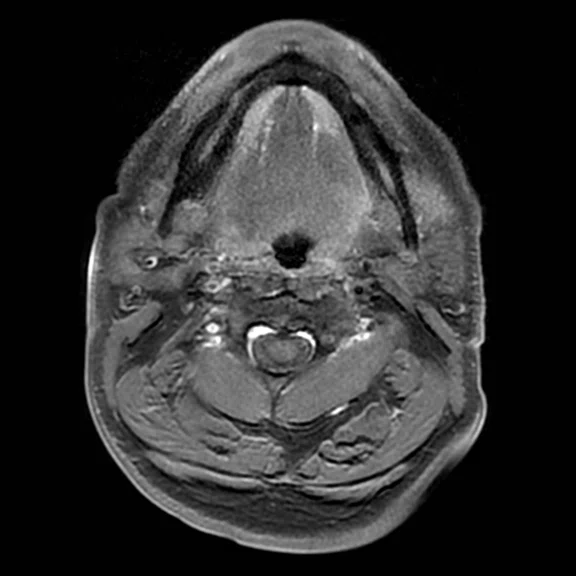
B
Figure 3.
(A) Axial T1 PROPELLER, 3:16 min., (B) axial T2 FSE Flex, 3:17 min., (C) axial T1 FSE Flex with contrast, 2:46 min. and (D) axial LAVA Flex with contrast, 2:00 min.
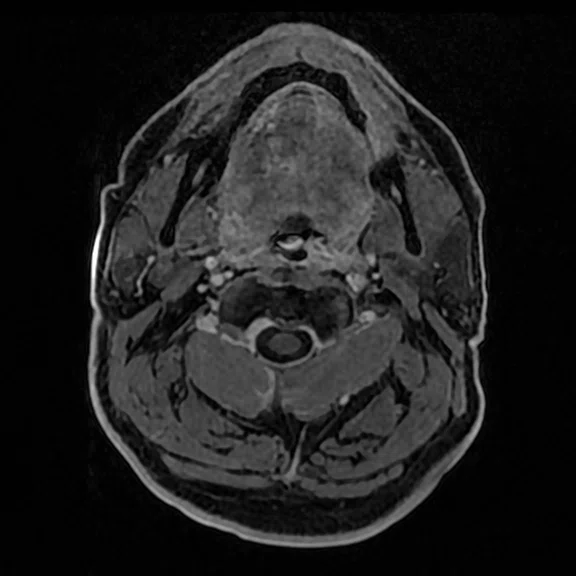
C
Figure 3.
(A) Axial T1 PROPELLER, 3:16 min., (B) axial T2 FSE Flex, 3:17 min., (C) axial T1 FSE Flex with contrast, 2:46 min. and (D) axial LAVA Flex with contrast, 2:00 min.
D
Figure 3.
(A) Axial T1 PROPELLER, 3:16 min., (B) axial T2 FSE Flex, 3:17 min., (C) axial T1 FSE Flex with contrast, 2:46 min. and (D) axial LAVA Flex with contrast, 2:00 min.
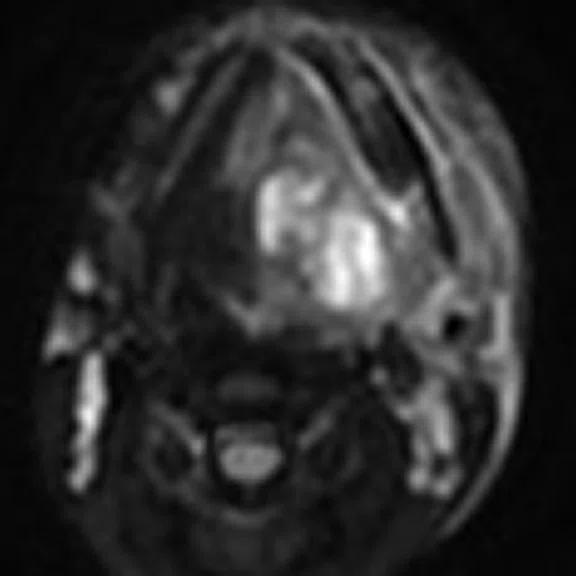
A
Figure 4.
(A) Axial STIR DWI, b800 mm-2s, 5:40 min. and (B) ADC map mm-2s-1.
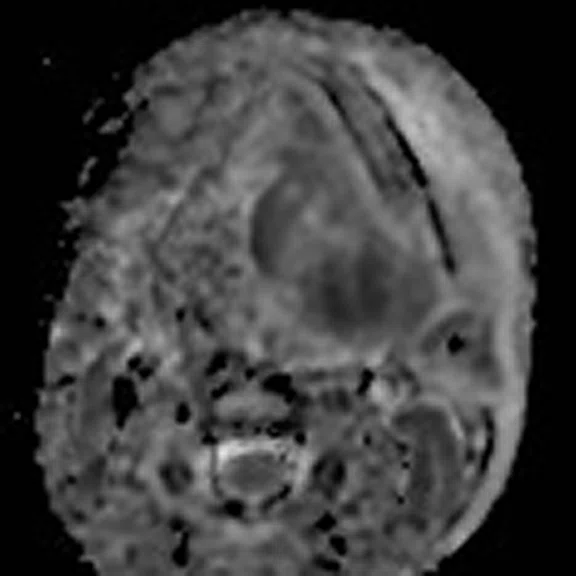
B
Figure 4.
(A) Axial STIR DWI, b800 mm-2s, 5:40 min. and (B) ADC map mm-2s-1.
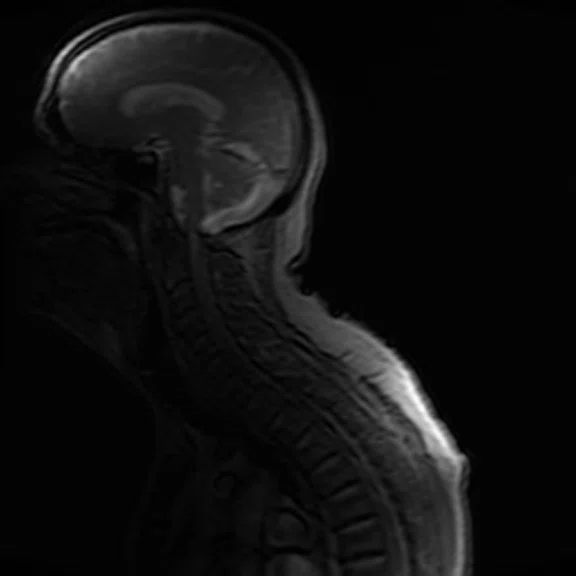
A
Figure 5.
Kyphotic patient necessitated use of AIR™ AA Coil.
A
Figure 6.
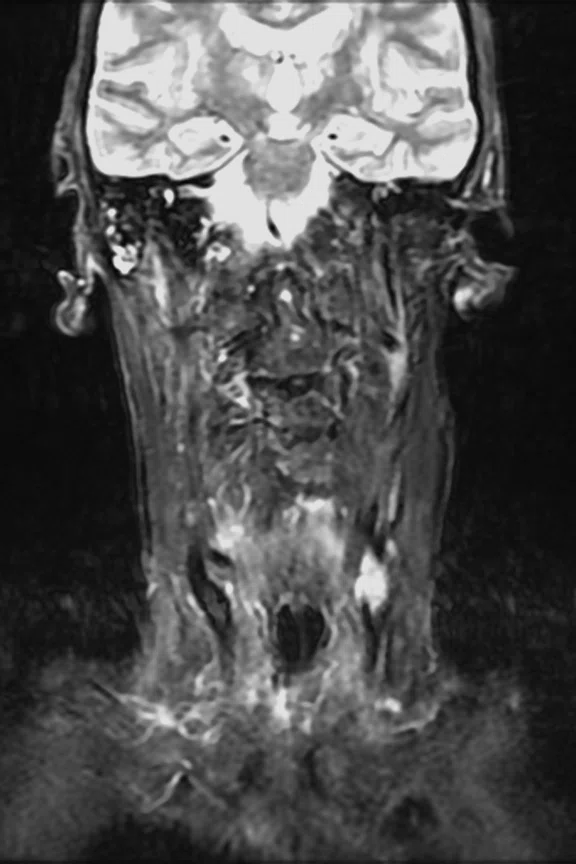
(A) Coronal STIR PROPELLER, 4:10 min., (B) coronal T1 PROPELLER, 3:25 min and (C) coronal T1 FSE Flex with contrast, 3:36 min.
B
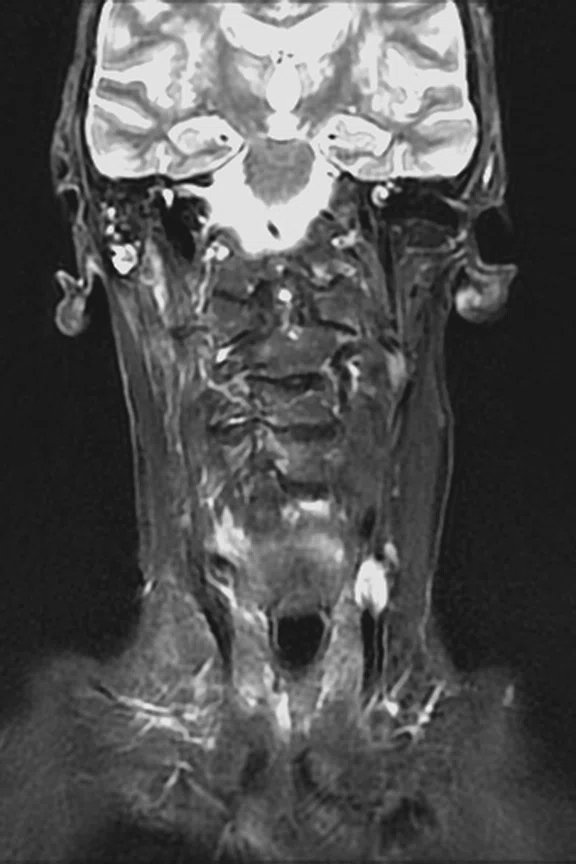
Figure 6.
(A) Coronal STIR PROPELLER, 4:10 min., (B) coronal T1 PROPELLER, 3:25 min and (C) coronal T1 FSE Flex with contrast, 3:36 min.
C
Figure 6.
(A) Coronal STIR PROPELLER, 4:10 min., (B) coronal T1 PROPELLER, 3:25 min and (C) coronal T1 FSE Flex with contrast, 3:36 min.
A
Figure 7.
(A) Axial T1 PROPELLER, 3:56 min., (B) axial T2 FSE Flex, 3:38 min., (C) axial T1 FSE Flex with contrast, 3:10 min. and (D) axial LAVA Flex with contrast, 2:01 min.
B
Figure 7.
(A) Axial T1 PROPELLER, 3:56 min., (B) axial T2 FSE Flex, 3:38 min., (C) axial T1 FSE Flex with contrast, 3:10 min. and (D) axial LAVA Flex with contrast, 2:01 min.
C
Figure 7.
(A) Axial T1 PROPELLER, 3:56 min., (B) axial T2 FSE Flex, 3:38 min., (C) axial T1 FSE Flex with contrast, 3:10 min. and (D) axial LAVA Flex with contrast, 2:01 min.
D
Figure 7.
(A) Axial T1 PROPELLER, 3:56 min., (B) axial T2 FSE Flex, 3:38 min., (C) axial T1 FSE Flex with contrast, 3:10 min. and (D) axial LAVA Flex with contrast, 2:01 min.
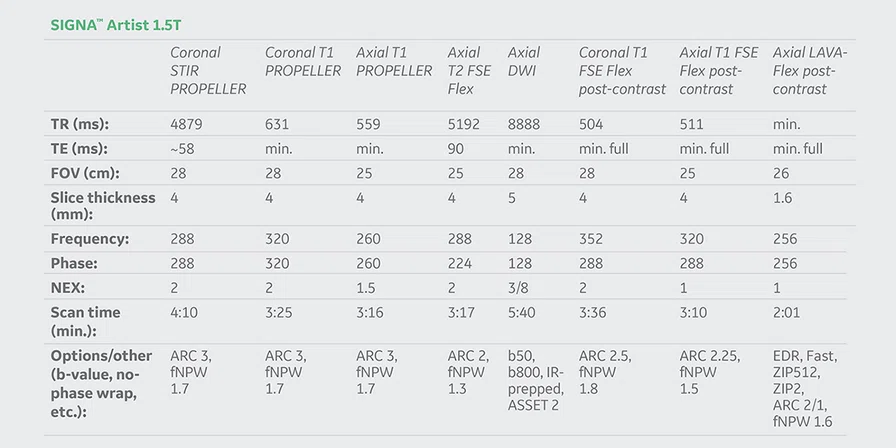
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
CASE STUDIES
Improving soft tissue neck imaging with shorter scan times, robust fat nulling and high SNR
Improving soft tissue neck imaging with shorter scan times, robust fat nulling and high SNR
by Lawrence Kenning, PhD, Medical Physicist, Susanna Valfre, BSc, PgC, Specialist MR Radiographer, and Richard List, FRCR, EDiNR, Consultant Radiologist in Head and Neck and Neuroradiology, Hull University Teaching Hospitals NHS Trust, Hull, UK
MR imaging of the head and neck is challenging for a number of reasons. Nulling the signal from fat is challenging since it is difficult to obtain a homogeneous magnetic field due to the anatomical shape of the head-neck-shoulder region. Additionally, robust fat nulling is required over a relatively large field-of-view (FOV). A number of blood vessels run through the neck region, contributing to pulsatile artifacts degrading the image quality. Often, these patients have malignancies and treatments that can affect their ability to comfortably lay on their back for extended periods of time. Also, because treatment may limit saliva production, some patients experience dry mouth and are prone to excessive swallowing.
Motion-related artifacts, including those from voluntary and involuntary motion, can obscure pathology. PROPELLER is a game-changer in terms of reducing motion/flow artifacts and provides a more signal-rich image due to the oversampling of the center of k-space. STIR PROPELLER and T1 PROPELLER are even less sensitive to flow and voluntary/involuntary motion than a traditional FSE sequence, resulting in a clearer depiction of the patient’s anatomy.
Robust and uniform fat nulling across the entire FOV, typically 28 cm, is important for characterizing neck pathology. Traditional chemical FatSat techniques often fail due to an inhomogeneous magnetic field. Flex, a 2-point Dixon technique, is more robust over a difficult anatomic area like the neck and results in uniform nulling of the fat signal even over a large FOV.
Reducing scan times for this patient cohort, who often have difficulty laying in the supine position, delivers both patient comfort and image quality benefits. With SIGNA™Works AIR™ Edition, we can reliably accelerate the PROPELLER sequence from ARC 2 to ARC 3. FSE Flex is another 2-point Dixon technique for robust fat modeling across the FOV that can produce sharper images in less time compared to IDEAL, a 3-point Dixon technique.
With FSE sequences, SCENIC provides a uniform signal intensity across the entire FOV combined with a noise reduction filter. AIR™ Recon selects only the coil elements contributing to signal, therefore reducing out of FOV artifacts such as ghosting that can impact interpretation.
Flexible No Phase Wrap (NPW) is an option that can be applied to FSE Flex and PROPELLER, enabling us to use a lower NPW factor (1.3-1.8), which when combined with partial NEX can further reduce scan times to limit the impact of patient movement Flexible NPW is user selectable based on the patient’s size. The combination of these scan time reductions has decreased total exam time by a third, from approximately 45 minutes to just under 30 minutes, compared to our other 1.5T MR system with an earlier software version.
Complementing the improvements in these sequences are the AIR™ Anterior Array (AA) Coil and AIR™ Recon. The AIR™ AA Coil has a higher channel count, delivering more signal-to-noise ratio (SNR). It provides added flexibility, with the ability to combine it with the integrated head and neck unit (HNU), a Flex coil and/or the posterior array (PA) if needed. AIR™ Recon is a reconstruction technology that reduces background noise and out-of-FOV artifacts for improved SNR and sharper images, enabling us to further reduce scan times.
Case 1
Patient history
A 10-year-old male presenting with anterior neck swelling from left submandibular mass with mild soreness for six days. The mass gradually increased in size and was crossing midline, restricting neck movement and causing trismus. Patient had neck surgery six years prior, however, limited information was available.
Results
There is a large inflammatory mass in the left sublingual, submandibular and parapharyngeal spaces, with pockets of restricted diffusion consistent with abscess formation. This extends through a congenital defect in the mylohyoid into the anterior neck.
Case 2
Patient history
A 65-year-old male with a three-month history of a right tonsil mass and associated sore throat on the right side. Kyphotic patient unable to fit in standard HNU; posterior elements of the HNU (no faceplate) and AIR™ AA Coil were used.
Results
The right palatine tonsil is larger than the left, however, there is no radiological evidence of a tumor in the tonsil or of invasion into adjacent structures. Normal striated appearance of tonsil. No cervical lymphadenopathy. Tonsillectomy was performed on clinical grounds: chronic tonsillitis with tonsillolith and actinomyces.
Discussion
These cases highlight how, with the dedicated support of our medical physicist and radiographers, we are able to optimize imaging on the SIGNA™ Artist system to produce high-quality, diagnostic images in difficult situations and with challenging patients. Unwell children often struggle to tolerate MR. The reduced scan time is better tolerated to completion without compromising on image quality and avoiding the need to irradiate the child using CT.
Implementing SIGNA™Works AIR™ Edition delivers a significant improvement in image quality and reduction in scan times. Every part of our protocol has been enhanced – it is not just one sequence or advancement, but rather the sum of all that enables us to accelerate as fast as we do and obtain high image quality. AIR™ Recon provides us with the confidence in SNR to accelerate sequences further. Flexible NPW allows us to decrease scan times. STIR PROPELLER reduces flow and patient motion artifacts, which when combined with SCENIC, provides uniformity correction and denoising. FSE Flex delivers complete and homogeneous fat nulling. The AIR™ AA Coil improves SNR with a higher channel count and increases patient comfort. It also provides the flexibility to image patients who cannot tolerate or fit inside the standard coil, such as the elderly kyphotic patient, and still produce diagnostic images. The synergy of SIGNA™ Artist with SIGNA™Works AIR™ Edition results in higher SNR and more reproducible exams, and improves workflow and clinical confidence.