A
Figure 1.
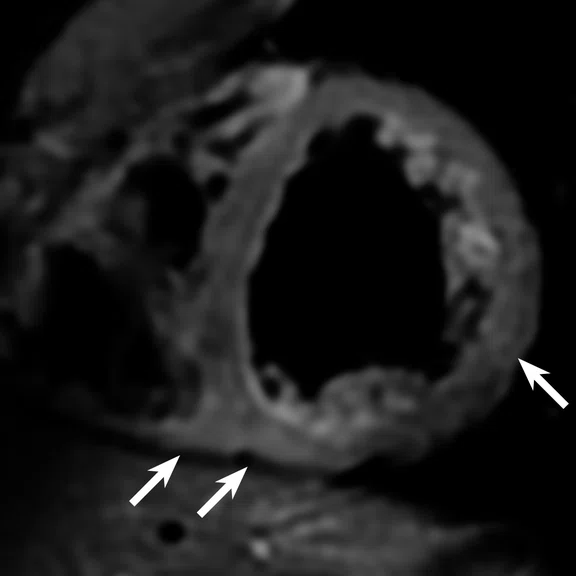
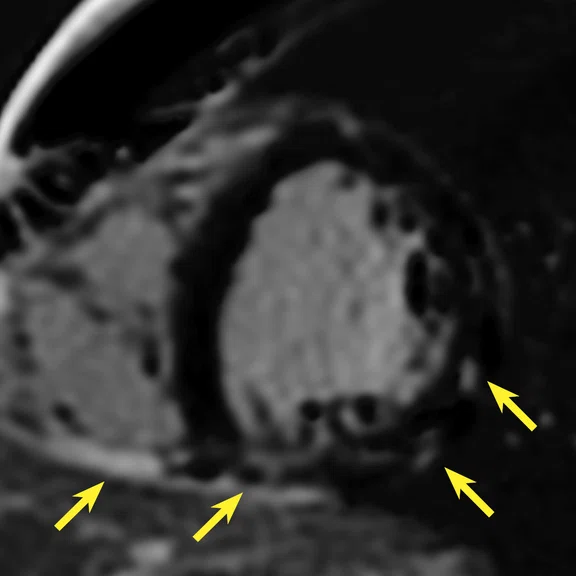
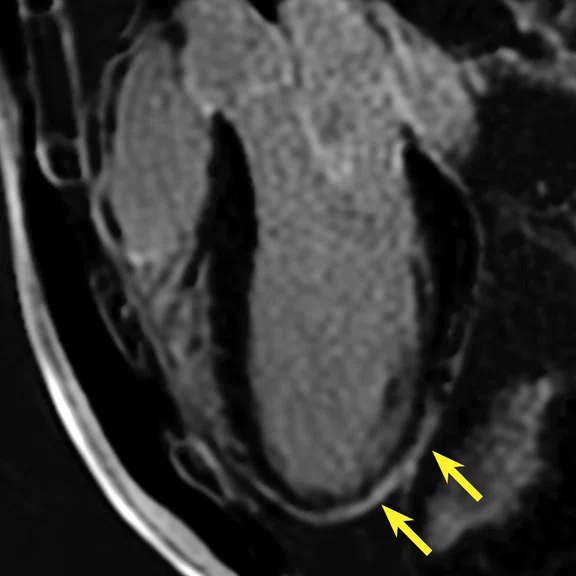
Acute myopericarditis in an asymptomatic athlete recovering from COVID-19. Cardiac MR revealed patchy mid- and epicardial late gadolinium enhancement (LGE) as well as pericardial enhancement (yellow arrows) and corresponding elevated T2w signal on the (A) fat-saturated double inversion recovery fast spin echo (SS BBFSE) image (white arrows). Also shown are (B) T1w phase-sensitive inversion recovery late gadolinium enhanced (PS MDE) and (C) 3-chamber view T1w PSIR LGE (3-chamber PS MDE) image.
B
Figure 1.
Acute myopericarditis in an asymptomatic athlete recovering from COVID-19. Cardiac MR revealed patchy mid- and epicardial late gadolinium enhancement (LGE) as well as pericardial enhancement (yellow arrows) and corresponding elevated T2w signal on the (A) fat-saturated double inversion recovery fast spin echo (SS BBFSE) image (white arrows). Also shown are (B) T1w phase-sensitive inversion recovery late gadolinium enhanced (PS MDE) and (C) 3-chamber view T1w PSIR LGE (3-chamber PS MDE) image.
C
Figure 1.
Acute myopericarditis in an asymptomatic athlete recovering from COVID-19. Cardiac MR revealed patchy mid- and epicardial late gadolinium enhancement (LGE) as well as pericardial enhancement (yellow arrows) and corresponding elevated T2w signal on the (A) fat-saturated double inversion recovery fast spin echo (SS BBFSE) image (white arrows). Also shown are (B) T1w phase-sensitive inversion recovery late gadolinium enhanced (PS MDE) and (C) 3-chamber view T1w PSIR LGE (3-chamber PS MDE) image.
1. Kim JH, Levine BD, Phelan D, et al. Coronavirus Disease 2019 and the Athletic Heart: Emerging Perspectives on Pathology, Risks, and Return to Play. JAMA Cardiol. 2021 Feb 1;6(2):219-227. doi: 10.1001/jamacardio.2020.5890.
2. Siripanthong B, Nazarian S, Muser D, et al. Recognizing COVID-19-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020;17(9):1463-1471. doi:10.1016/j.hrthm.2020.05.001.
3. Rathore SS, Rojas GA, Sondhi M, et al. Myocarditis associated with Covid-19 disease: A systematic review of published case reports and case series. Int J Clin Pract. 2021 Jul 7:e14470. doi: 10.1111/ijcp.14470.
2. Siripanthong B, Nazarian S, Muser D, et al. Recognizing COVID-19-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020;17(9):1463-1471. doi:10.1016/j.hrthm.2020.05.001.
4. Wilson M, O'Hanlon R, Prasad S, et al. Diverse patterns of myocardial fibrosis in lifelong, veteran endurance athletes. J Appl Physiol (1985). 2011 Jun;110(6):1622-6. doi: 10.1152/japplphysiol.01280.2010.
5. Małek, ŁA, Bucciarelli-Ducci, C. Myocardial fibrosis in athletes—Current perspective. Clin Cardiol. 2020; 43: 43: 882– 888. https://doi.org/10.1002/clc.23360.
6. Starekova J, Bluemke DA, Bradham WS, et al. Evaluation for Myocarditis in Competitive Student Athletes Recovering From Coronavirus Disease 2019 With Cardiac Magnetic Resonance Imaging. JAMA Cardiol.2021;6(8):945–950. doi:10.1001/jamacardio.2020.7444.
6. Starekova J, Bluemke DA, Bradham WS, et al. Evaluation for Myocarditis in Competitive Student Athletes Recovering From Coronavirus Disease 2019 With Cardiac Magnetic Resonance Imaging. JAMA Cardiol.2021;6(8):945–950. doi:10.1001/jamacardio.2020.7444.
7. Udelson JE, Curtis MA, Rowin EJ. Return to Play for Athletes After Coronavirus Disease 2019 Infection—Making High- Stakes Recommendations as Data Evolve. JAMA Cardiol. 2021;6(2):136–138. doi:10.1001/jamacardio.2020.5896.
8. Petersen SE, Friedrich MG, Leiner T, et al. Cardiovascular Magnetic Resonance for Patients With COVID-19. J Am Coll Cardiol Img. Oct 13, 2021. Article in press. DOI: 10.1016/j.jcmg.2021.08.021.
9. Daniels CJ, Rajpal S, Greenshields, et al. Big Ten COVID-19 Cardiac Registry Investigators. Prevalence of Clinical and Subclinical Myocarditis in Competitive Athletes With Recent SARS-CoV-2 Infection: Results From the Big Ten COVID-19 Cardiac Registry. JAMA Cardiol. 2021 Sep 1;6(9):1078-1087. doi: 10.1001/jamacardio.2021.2065.
10. Starekova J, Thottakara T, Lund GK, et al. Increased myocardial mass and attenuation of myocardial strain in professional male soccer players and competitive male triathletes. Int J Cardiovasc Imaging. 2020;36(11):2187-2197. doi:10.1007/s10554-020-01918-1.
11. Kim JH, Levine BD, Phelan D, et al. Coronavirus Disease 2019 and the Athletic Heart: Emerging Perspectives on Pathology, Risks, and Return to Play. JAMA Cardiol. 2021;6(2):219–227. doi:10.1001/jamacardio.2020.5890.
8. Petersen SE, Friedrich MG, Leiner T, et al. Cardiovascular Magnetic Resonance for Patients With COVID-19. J Am Coll Cardiol Img. Oct 13, 2021. Article in press. DOI: 10.1016/j.jcmg.2021.08.021.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
SPOTLIGHT
Myocarditis in COVID-19-positive student athletes
Myocarditis in COVID-19-positive student athletes
COVID-19-related myocarditis has been reported in the literature1,2,3 with clinical findings including changes in electrocardiogram and cardiac biomarkers, and impaired cardiac function2. At the start of the pandemic, positive cases of COVID-19 were reported at the University of Wisconsin (UW)-Madison, prompting a group of professors, including Jitka Starekova, MD, a Bracco-sponsored Visiting Assistant Professor in the Department of Radiology, to investigate whether cardiac MRI could be used as a screening tool for myocarditis in competitive student athletes after recovering from COVID-19.
"Myocarditis and inflammation of the heart muscle may lead to fibrosis (scar tissue in the heart), a potential substrate for cardiac arrhythmias, and may result in sudden cardiac death in athletes," Dr. Starekova says.
Small areas of myocardial fibrosis have been previously detected in athletes, including middle-aged or veteran athletes, where there was a higher prevalence of fibrosis compared to age-matched controls4,5.
"We know that focal fibrosis can occur also at a younger age, however, longitudinal studies are needed to evaluate its clinical relevance in otherwise asymptomatic athletes. We need to prove the potential link between fibrosis and fatal events," she adds.
In collaboration with the Big Ten conference, Dr. Starekova and colleagues initiated a screening program to evaluate all student athletes who tested positive for COVID-19. After completing a 10-day quarantine, each student athlete underwent cardiac MRI on either a 1.5T or 3.0T MR system using a standardized myocarditis protocol that included T2 BBFSE, T1 and T2 mapping, 2D FIESTA and PS MDE6.
Of the 145 student athletes, nearly half had mild symptoms, slightly more than one-quarter had moderate symptoms and the remainder were either asymptomatic or did not specify symptoms6. Based on the cardiac MRI exam, only a small portion, 1.4% (two athletes), had myocarditis-like findings6.
Figure 1.
Acute myopericarditis in an asymptomatic athlete recovering from COVID-19. Cardiac MR revealed patchy mid- and epicardial late gadolinium enhancement (LGE) as well as pericardial enhancement (yellow arrows) and corresponding elevated T2w signal on the (A) fat-saturated double inversion recovery fast spin echo (SS BBFSE) image (white arrows). Also shown are (B) T1w phase-sensitive inversion recovery late gadolinium enhanced (PS MDE) and (C) 3-chamber view T1w PSIR LGE (3-chamber PS MDE) image.
Although prevalence of myocarditislike MR findings in athletes recovering from COVID-19 varied from 0 up to 15% in single center studies7, recently performed multicenter studies confirmed prevalence at the lower end of this range8. For example, the results from the Big Ten COVID-19 Cardiac Registry, of which UW-Madison participated, showed that 2.3% of 1,597 athletes diagnosed with COVID-19 had clinical or sub-clinical myocarditis9.
However, "the clinical significance of these myocarditis-like findings could be only determined after prospective longitudinal studies of these young athletes," Dr. Starekova points out.
Limitations of the UW-Madison study, and of many other studies on athletes, were retrospective design, lack of case-controls and lack of appropriate normative values (e.g., by age, gender, type of sport), an issue that Dr. Starekova believes could be resolved with further studies on younger athletes. A strength of the UW study was the inclusion of all athletes who tested positive for COVID-19, a factor that would reduce potential bias.
"The MR findings of athletes recovering from COVID-19 need to be interpreted carefully," Starekova said. For example, focal septal fibrosis, at inferior insertion point of the right ventricle, has been previously reported in connection with athletic training and is unlikely to have been caused by COVID-19. Further, COVID-19 may alter cardiac function, however, attenuation of myocardial strain was seen also in athletes without COVID-19, and was shown to be associated with the level of myocardial hypertrophy10.
“It is very important to understand that different sports lead to different cardiac adaptations or remodeling, and avoid possible misinterpretations.”
Dr. Jitka Starekova
To ensure the safety of all COVID-19 positive student athletes, a returnto-play protocol was developed. First, students had to be asymptomatic and then they could gradually resume the sport activity11. In the event that student athletes experienced new onset of cardiac symptoms, it was advised they undergo ECG and echocardiography, and cardiac MRI should be considered8.