A
Figure 1.
Liver exam with AIR™ Recon DL demonstrates the image quality improvements that enable depiction of a small lesion in the left lobe. (A) Axial T2w, 0.9 x 1.2 x 3 mm, 5:50 min.; (B) high-resolution axial DWI, 2.2 x 1.4 x 5 mm, 3:24 min.; and (C) ADC map.
B
Figure 1.
Liver exam with AIR™ Recon DL demonstrates the image quality improvements that enable depiction of a small lesion in the left lobe. (A) Axial T2w, 0.9 x 1.2 x 3 mm, 5:50 min.; (B) high-resolution axial DWI, 2.2 x 1.4 x 5 mm, 3:24 min.; and (C) ADC map.
C
Figure 1.
Liver exam with AIR™ Recon DL demonstrates the image quality improvements that enable depiction of a small lesion in the left lobe. (A) Axial T2w, 0.9 x 1.2 x 3 mm, 5:50 min.; (B) high-resolution axial DWI, 2.2 x 1.4 x 5 mm, 3:24 min.; and (C) ADC map.
A
Figure 2.
In the case of a 79-year-old female, using FOCUS DWI with AIR™ Recon DL demonstrates high signal of the pancreas, enabling confirmation of a pancreatic tumor. Because of the high spatial resolution images, it was possible to visualize the spiculation of the tumor, as shown in the (D) MAGiC DWI and (E) ADC map. (A) Axial T2w SSFSE with AIR™ Recon DL, 0.9 x 1.1 x 5 mm, 37 sec.; (B) 3D MRCP with Auto Navigator; (C) axial FOCUS DWI with AIR™ Recon DL, b600, 1.8 x 3.4 x 3 mm, 4 min.; (D) MAGiC DWI, b1000; and (E) ADC map.
B
Figure 2.
In the case of a 79-year-old female, using FOCUS DWI with AIR™ Recon DL demonstrates high signal of the pancreas, enabling confirmation of a pancreatic tumor. Because of the high spatial resolution images, it was possible to visualize the spiculation of the tumor, as shown in the (D) MAGiC DWI and (E) ADC map. (A) Axial T2w SSFSE with AIR™ Recon DL, 0.9 x 1.1 x 5 mm, 37 sec.; (B) 3D MRCP with Auto Navigator; (C) axial FOCUS DWI with AIR™ Recon DL, b600, 1.8 x 3.4 x 3 mm, 4 min.; (D) MAGiC DWI, b1000; and (E) ADC map.
C
Figure 2.
In the case of a 79-year-old female, using FOCUS DWI with AIR™ Recon DL demonstrates high signal of the pancreas, enabling confirmation of a pancreatic tumor. Because of the high spatial resolution images, it was possible to visualize the spiculation of the tumor, as shown in the (D) MAGiC DWI and (E) ADC map. (A) Axial T2w SSFSE with AIR™ Recon DL, 0.9 x 1.1 x 5 mm, 37 sec.; (B) 3D MRCP with Auto Navigator; (C) axial FOCUS DWI with AIR™ Recon DL, b600, 1.8 x 3.4 x 3 mm, 4 min.; (D) MAGiC DWI, b1000; and (E) ADC map.
D
Figure 2.
In the case of a 79-year-old female, using FOCUS DWI with AIR™ Recon DL demonstrates high signal of the pancreas, enabling confirmation of a pancreatic tumor. Because of the high spatial resolution images, it was possible to visualize the spiculation of the tumor, as shown in the (D) MAGiC DWI and (E) ADC map. (A) Axial T2w SSFSE with AIR™ Recon DL, 0.9 x 1.1 x 5 mm, 37 sec.; (B) 3D MRCP with Auto Navigator; (C) axial FOCUS DWI with AIR™ Recon DL, b600, 1.8 x 3.4 x 3 mm, 4 min.; (D) MAGiC DWI, b1000; and (E) ADC map.
E
Figure 2.
In the case of a 79-year-old female, using FOCUS DWI with AIR™ Recon DL demonstrates high signal of the pancreas, enabling confirmation of a pancreatic tumor. Because of the high spatial resolution images, it was possible to visualize the spiculation of the tumor, as shown in the (D) MAGiC DWI and (E) ADC map. (A) Axial T2w SSFSE with AIR™ Recon DL, 0.9 x 1.1 x 5 mm, 37 sec.; (B) 3D MRCP with Auto Navigator; (C) axial FOCUS DWI with AIR™ Recon DL, b600, 1.8 x 3.4 x 3 mm, 4 min.; (D) MAGiC DWI, b1000; and (E) ADC map.
A
Figure 3.
(A) Auto Navigator DWI, b1000, 4 NEX, 1.8 x 1.4 x 9 mm, 2:33 min. with (B) corresponding ADC map. (C) Using AIR™ Recon DL, breath-hold DWI, b1000, 1 NEX, 2.7 x 2.2 x 9 mm, 14 sec. with (D) corresonding ADC map.
B-1
Figure 3.
(A) Auto Navigator DWI, b1000, 4 NEX, 1.8 x 1.4 x 9 mm, 2:33 min. with (B) corresponding ADC map. (C) Using AIR™ Recon DL, breath-hold DWI, b1000, 1 NEX, 2.7 x 2.2 x 9 mm, 14 sec. with (D) corresonding ADC map.
B-2
Figure 3.
(A) Auto Navigator DWI, b1000, 4 NEX, 1.8 x 1.4 x 9 mm, 2:33 min. with (B) corresponding ADC map. (C) Using AIR™ Recon DL, breath-hold DWI, b1000, 1 NEX, 2.7 x 2.2 x 9 mm, 14 sec. with (D) corresonding ADC map.
C
Figure 3.
(A) Auto Navigator DWI, b1000, 4 NEX, 1.8 x 1.4 x 9 mm, 2:33 min. with (B) corresponding ADC map. (C) Using AIR™ Recon DL, breath-hold DWI, b1000, 1 NEX, 2.7 x 2.2 x 9 mm, 14 sec. with (D) corresonding ADC map.
D-1
Figure 3.
(A) Auto Navigator DWI, b1000, 4 NEX, 1.8 x 1.4 x 9 mm, 2:33 min. with (B) corresponding ADC map. (C) Using AIR™ Recon DL, breath-hold DWI, b1000, 1 NEX, 2.7 x 2.2 x 9 mm, 14 sec. with (D) corresonding ADC map.
D-2
Figure 3.
(A) Auto Navigator DWI, b1000, 4 NEX, 1.8 x 1.4 x 9 mm, 2:33 min. with (B) corresponding ADC map. (C) Using AIR™ Recon DL, breath-hold DWI, b1000, 1 NEX, 2.7 x 2.2 x 9 mm, 14 sec. with (D) corresonding ADC map.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
SPOTLIGHT
A level above the rest in abdominal diffusion imaging
A level above the rest in abdominal diffusion imaging
Abdominal MR is a challenging exam due to multiple factors, including motion artifacts manifesting from respiration, heartbeat and peristalsis, susceptibility artifacts from bowel gas, B1 inhomogeneities resulting from the large size of the abdomen and the need to often acquire a large field-of-view (FOV). These issues may intensify at higher field strengths (e.g., 3.0T).
Abdominal MR is a challenging exam due to multiple factors, including motion artifacts manifesting from respiration, heartbeat and peristalsis, susceptibility artifacts from bowel gas, B1 inhomogeneities resulting from the large size of the abdomen and the need to often acquire a large field-of-view (FOV). These issues may intensify at higher field strengths (e.g., 3.0T).
Addressing these issues often involves modifying parameters to optimize the acquisition; however, there are trade- offs in MR between scan time and signal-to-noise ratio (SNR) that may limit changes to sequences. Artifacts can lead to blurring and ghosting, reducing image quality and rendering the study difficult to read for diagnosis.
At Fukuoka University Hospital (Fukuoka, Japan), Kengo Yoshimitsu, MD, PhD, Chairman of the Radiology Department and Professor of Radiology, specializes in abdominal radiology and in particular liver and pancreatic diseases. He has published extensively on MR imaging of the liver, pancreas and kidney. Recently, he oversaw the upgrade of the department’s Discovery™ MR750w to SIGNA™Works AIRTM IQ Edition software, which includes AIR™ Recon DL.
Initially, Professor Yoshimitsu was not very familiar with deep learning (DL) technologies. He thought DL may be difficult to apply and make it more complex to acquire high-quality images.
However, he soon discovered this was not the case with AIR™ Recon DL.
“The first impression of AIR™ Recon DL is that it is very good image quality, which is very uniform and has little noise, and scanning can be shortened,” Professor Yoshimitsu says. “It was not difficult to use AIR™ Recon DL and we apply it to all compatible abdominal pulse sequences.”
The first step was to consider the appropriate level of optimization to use with AIR™ Recon DL. Professor Yoshimitsu and his colleagues compared each DL strength (high, medium, low) using the same data. After evaluating the benefits of each level, they chose “high” for most pulse sequences.
“I feel that it is very easy to use in static anatomy such as MSK,” he adds. “The T2-weighted or DWI of the liver had a factor that could not be solved by a simple image quality improvement technique. However, it was solved by the enhancement of the DWI function in the new version of AIR™ Recon DL. I feel that there is no better MR technology.”
An enormous impact on image quality
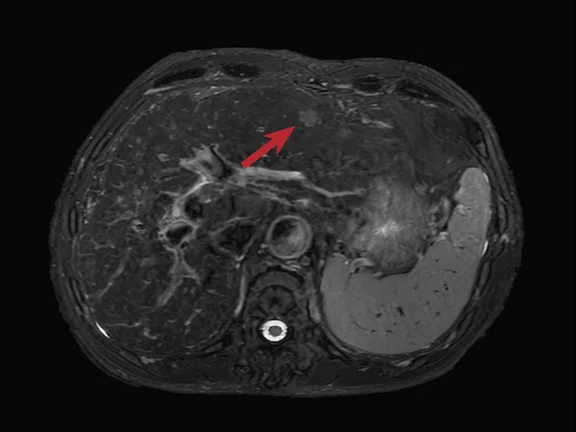
In the liver and pancreas, the impact of AIR™ Recon DL on SNR and the overall quality of the study is impressive for Professor Yoshimitsu. He has had many MR exams where the left lobe of the liver couldn’t be visualized using DWI due to the patient’s beating heart. In patients with iron deposits in their liver, the liver is “buried” in white noise. Both of these situations often make it very difficult to render a confident diagnosis.
“The benefits of AIR™ Recon DL are enormous, especially the image quality improvement in DWI and SSFSE T2w, making diagnosis easier than before,” Professor Yoshimitsu explains (Figure 1). “As a result, it is possible to obtain signals from the left lobe of the liver even with DWI and to detect very small lesions.”
Professor Yoshimitsu has also seen improved image quality as a result of using FOCUS DWI with AIR™ Recon DL. At Fukuoka University Hospital, FOCUS DWI is utilized for most pancreatic MR exams.
“With FOCUS DWI, it is possible to not only capture high signals in pancreatic head tumors, but also to depict the tumor spiculation,” Professor Yoshimitsu explains (Figure 2).
Figure 2.
In the case of a 79-year-old female, using FOCUS DWI with AIR™ Recon DL demonstrates high signal of the pancreas, enabling confirmation of a pancreatic tumor. Because of the high spatial resolution images, it was possible to visualize the spiculation of the tumor, as shown in the (D) MAGiC DWI and (E) ADC map. (A) Axial T2w SSFSE with AIR™ Recon DL, 0.9 x 1.1 x 5 mm, 37 sec.; (B) 3D MRCP with Auto Navigator; (C) axial FOCUS DWI with AIR™ Recon DL, b600, 1.8 x 3.4 x 3 mm, 4 min.; (D) MAGiC DWI, b1000; and (E) ADC map.
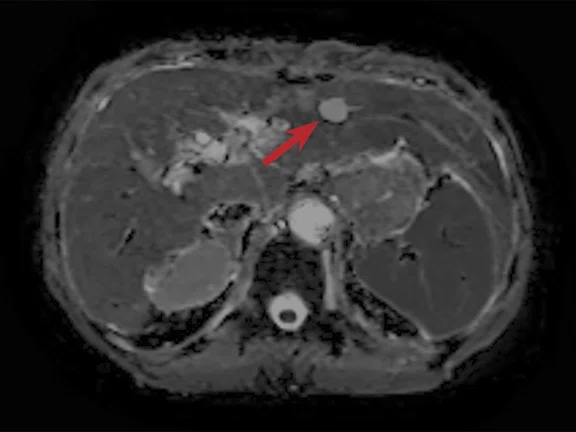
Considering that the most significant issue in MR abdominal imaging is the impact of breathing motion and heartbeat on image quality, the radiology department at Fukuoka University Hospital considered breath- hold scanning and diaphragm navigation.
At first, the SNR improvement with AIR™ Recon DL enabled the use of 1 NEX in a liver DWI scan. Breath-hold DWI in the upper abdomen further reduced misregistration of the ADC map, resulting in more reliable ADC values in the liver (Figure 3).
By using Auto Navigator, the technologists could obtain a stable breathing waveform by fixing the thorax with the abdominal belt. As a result, the department has shortened the scan time while achieving high image quality. With the shorter scan times, Professor Yoshimitsu says they can now add SSFSE and breath-holding DWI sequences.
Shorter scan times benefit patients and radiologists
Professor Yoshimitsu believes there is no doubt that shorter exam times will reduce patient stress. In many exams, reducing NEX reduces imaging time; however, there is an accompanying reduction in SNR.
The priority of choosing scan time reductions or SNR improvements changes for each exam, he further explains. “For example, in a follow-up brain or MSK exam, we will use AIR™ Recon DL to save time. On the other hand, in abdominal MR imaging we use AIR™ Recon DL for image quality improvements or, if we reduce scan times, it is for an additional scan, such as MR elastography or IDEAL IQ.”
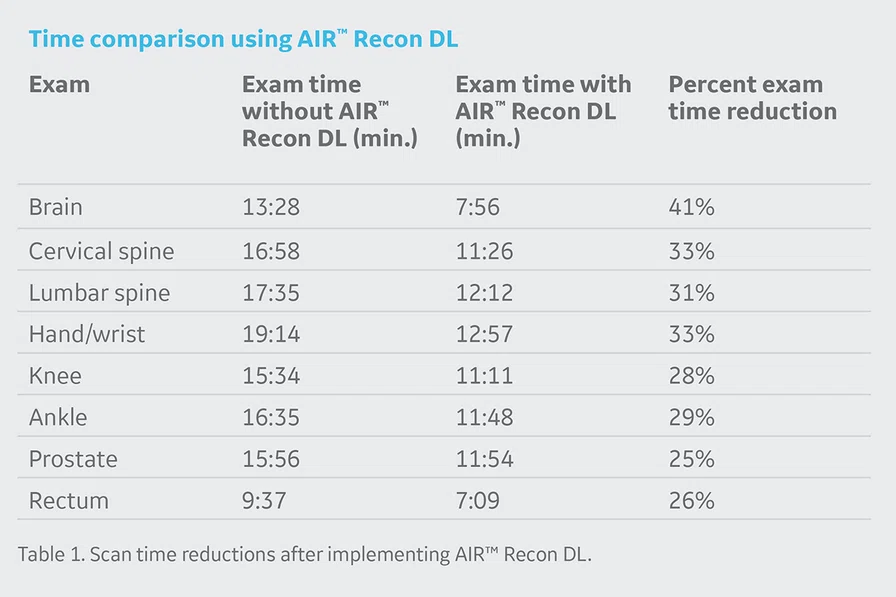
After implementing AIR™ Recon DL at Fukuoka University Hospital, the overall exam time has been shortened, on average, by nearly 31%, and the number of exams has increased by about 15%. He notes that the hospital’s pituitary protocol scan time was shortened by about 40% and that exams with a lot of 2D imaging, such as MSK, have consistently realized shorter scan times (Table 1).
“The ability to make an accurate diagnosis with AIR™ Recon DL is a direct benefit to patient care,” Professor Yoshimitsu says.
Shortening the scan time will reduce the burden to the patient during the exam. In addition, he says that radiologists can choose to improve the image quality according to the patient’s condition, such as increasing the spatial resolution with the same exam time. “I think that has the benefit of increasing the clinical information in the MR image and making it easier to diagnose,” he adds.
“I was most impressed that we were able to get very high quality images with the upgrade without having to buy new equipment. This was very exciting and a nice added benefit. So, I have no reason not to recommend AIR™ Recon DL,” Professor Yoshimitsu says.
Radiologists are also very pleased with the image quality improvements with AIR™ Recon DL, he continues.
“It’s not a complex or noisy image, so it’s faster and easier to read and diagnose. Quality of life is also improved for the radiologists by reducing the stress of diagnosis. AIR™ Recon DL makes patients and healthcare workers happy together. We would not revert to the pre-AIR™ Recon DL images, and we hope that the compatibility of AIR™ Recon DL will be further expanded in the future.”
Dr. Kengo Yoshimitsu