1. Pasvol TJ, Horsfall L, Bloom S, Segal AW, Sabin C, Field N, Rait G. Incidence and prevalence of inflammatory bowel disease in UK primary care: a population-based cohort study. BMJ Open. 2020 Jul 19;10(7):e036584. doi: 10.1136/ bmjopen-2019-036584. Erratum in: BMJ Open. 2020 Aug 27;10(8):e036584corr1. PMID: 32690524; PMCID: PMC7371214.
A
Figure 1.
(A-C) Initial CT imaging on days seven and nine post-op, demonstrating rim-enhancing collections (white arrows) and peritoneal thickening consistent with peritonitis.
B
Figure 1.
(A-C) Initial CT imaging on days seven and nine post-op, demonstrating rim-enhancing collections (white arrows) and peritoneal thickening consistent with peritonitis.
C
Figure 1.
(A-C) Initial CT imaging on days seven and nine post-op, demonstrating rim-enhancing collections (white arrows) and peritoneal thickening consistent with peritonitis.
A
Figure 2.
(A-C) Initial CT imaging on days seven and nine post-op, demonstrating rim-enhancing collections (white arrows) and peritoneal thickening consistent with peritonitis.
B
Figure 2.
(A-C) MR imaging performed three days after second drain placement showed reassuring findings with smaller collections (white arrows). Blue arrow is the drain tip.
C
Figure 2.
(A-C) MR imaging performed three days after second drain placement showed reassuring findings with smaller collections (white arrows). Blue arrow is the drain tip.
A
Figure 3.
(A, C, E) Exam 1. (A) Fluid collection (white arrows) and drain (blue arrow). (C, E) mesenteric edema (white arrows), small residual collection (E, yellow arrow). (B, D, E) Exam 2, showing a reduction in the fluid collections (B, D, white arrows) and resolution of mesenteric edema (E, white arrow) near drain tip (E, blue arrow).
B
Figure 3.
(A, C, E) Exam 1. (A) Fluid collection (white arrows) and drain (blue arrow). (C, E) mesenteric edema (white arrows), small residual collection (E, yellow arrow). (B, D, E) Exam 2, showing a reduction in the fluid collections (B, D, white arrows) and resolution of mesenteric edema (E, white arrow) near drain tip (E, blue arrow).
C
Figure 3.
(A, C, E) Exam 1. (A) Fluid collection (white arrows) and drain (blue arrow). (C, E) mesenteric edema (white arrows), small residual collection (E, yellow arrow). (B, D, E) Exam 2, showing a reduction in the fluid collections (B, D, white arrows) and resolution of mesenteric edema (E, white arrow) near drain tip (E, blue arrow).
D
Figure 3.
(A, C, E) Exam 1. (A) Fluid collection (white arrows) and drain (blue arrow). (C, E) mesenteric edema (white arrows), small residual collection (E, yellow arrow). (B, D, E) Exam 2, showing a reduction in the fluid collections (B, D, white arrows) and resolution of mesenteric edema (E, white arrow) near drain tip (E, blue arrow).
E
Figure 3.
(A, C, E) Exam 1. (A) Fluid collection (white arrows) and drain (blue arrow). (C, E) mesenteric edema (white arrows), small residual collection (E, yellow arrow). (B, D, E) Exam 2, showing a reduction in the fluid collections (B, D, white arrows) and resolution of mesenteric edema (E, white arrow) near drain tip (E, blue arrow).
F
Figure 3.
(A, C, E) Exam 1. (A) Fluid collection (white arrows) and drain (blue arrow). (C, E) mesenteric edema (white arrows), small residual collection (E, yellow arrow). (B, D, E) Exam 2, showing a reduction in the fluid collections (B, D, white arrows) and resolution of mesenteric edema (E, white arrow) near drain tip (E, blue arrow).
A
Figure 4.
(A) Original CT study showing small bowel inflammation (white arrows) and fluid collection (blue arrow). (B) MR exam 2 showing resolution of bowel inflammation with only a trace residual collection. Stoma bag contents (yellow arrow).
B
Figure 4.
(A) Original CT study showing small bowel inflammation (white arrows) and fluid collection (blue arrow). (B) MR exam 2 showing resolution of bowel inflammation with only a trace residual collection. Stoma bag contents (yellow arrow).
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.

David Bowden, FRCR
Addenbrooke’s Hospital,
Cambridge, United Kingdom
CASE STUDIES
AIR Coil: a game-changer in pediatric Crohn’s disease and acute abdomen cases
AIR Coil: a game-changer in pediatric Crohn’s disease and acute abdomen cases
by David Bowden, FRCR, Consultant Hepatobiliary and Gastroenterology Radiologist, Addenbrooke’s Hospital, Cambridge University Hospitals NHS Foundation Trust, Cambridge, United Kingdom
Crohn’s disease is a chronic inflammatory bowel disease that affects the lining of the digestive tract, causing abdominal pain, diarrhea, weight loss, fatigue and malnutrition. Although rare, with an estimated incidence rate of 10.2 per 100,000 people in the UK1 , it can be painful and debilitating, and can sometimes lead to life-threatening complications. Most people are diagnosed between 20-30 years old, and there is currently no cure for Crohn’s disease.
Imaging tests such as X-ray (fluoroscopy), CT and MR are often used to examine the intestine and bowels in patients with Crohn’s disease. In pediatric patients, MR is preferred where possible due to the lack of ionizing radiation.
Patient history
A 16-year-old patient with a history of Crohn’s disease since age 12 developed severe Crohn’s colitis refractory to medical treatment with severe abdominal pain, and subsequently required an emergency subtotal colectomy (complete removal of almost the entire large bowel). Postoperatively the patient had worsening pain; two abdominal CT exams on days seven and nine following surgery demonstrated enhancing fluid collections with features consistent with peritonitis (Figure 1). An additional chest CT was also required due to concerns regarding a possible pulmonary embolus.
Figure 3.
(A, C, E) Exam 1. (A) Fluid collection (white arrows) and drain (blue arrow). (C, E) mesenteric edema (white arrows), small residual collection (E, yellow arrow). (B, D, E) Exam 2, showing a reduction in the fluid collections (B, D, white arrows) and resolution of mesenteric edema (E, white arrow) near drain tip (E, blue arrow).
The patient continued to suffer pain and fever with elevated inflammatory markers, indicative of either significant residual or further collections despite the placement of two ultrasound-guided drains on day 10 and 17 following surgery.
The clinical team was concerned about the pediatric patient undergoing a further CT exam, having already been exposed to the equivalent radiation dose of 700 chest X-rays during this admission alone. Since the patient could not tolerate deep pressure due to ongoing peritonitis, ultrasound was deemed very unlikely to provide the image quality required to evaluate the pelvic collections.
While MR appeared to be the best imaging option, the patient was reluctant to undergo a repeat MR exam due to an inability to lie flat for a significant length of time or to tolerate a conventional surface coil due to pain.
However, our institution had recently acquired the AIR™ Anterior Array (AA) Coil, a lightweight, flexible coil that provides a more comfortable patient experience. I therefore suggested an attempt to persuade the patient to try an MR exam with this coil and provided pictures of it to the surgeon for reassurance. The patient subsequently agreed to the MR exam.
Results
MR imaging was performed three days after the second drain placement. Both coronal Cine and axial FIESTA acquisitions showed a significant reduction in the size of the collections, with the drain clearly visible within the right flank (Figure 2A). Axial SSFSE images also demonstrated only a minimal residual collection above the bladder and a reduction in both flank collections (Figure 2B-C) compared to original CT images (Figure 1). Image quality was very good despite a total scan time of only 12 minutes.
Of equal importance, the patient tolerated the scan extremely well and patient-controlled analgesia was not required during the transport to/from the MR room or during the MR exam.
A second MR study was subsequently requested six days later due to the patient’s continued pain and fever, with the attending surgeon specifically requesting the use of the AIR™ AA Coil given it was well tolerated previously.
The patient subsequently successfully underwent a second MR exam, which showed only trace fluid remaining and an improvement in mesenteric and resolution of small bowel inflammation (Figures 3 and 4). The patient continued to improve, drains were removed and the patient was discharged without further complications.
Discussion
This case highlights the impact the AIR™ AA Coil has on increased patient comfort and cooperation during an MR exam. Pediatric patients are often very challenging to image, particularly when in pain, and are frequently nervous, which can lead to movement artifact. Although initially skeptical, the patient tolerated imaging with the AIR™ AA Coil very well and was prepared to have additional imaging even though previous experiences with conventional surface coils had originally made the patient reluctant to agree to further MR exams.
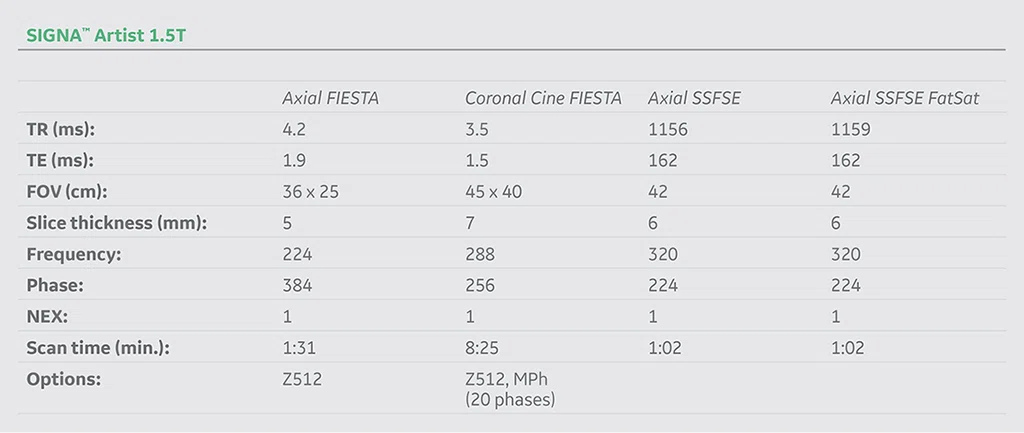
The use of rapid protocols on the SIGNA™ Artist 1.5T further increased patient comfort, an imaging option that was not previously available. Visually explaining the AIR™ AA Coil also helped reduce the patient’s anxiety and increased the likelihood that the patient would agree to the MR exam.
Without the AIR™ AA Coil and SIGNA™ Artist, the only imaging option available was additional CT imaging that would have led to significant further radiation exposure in a pediatric patient. Having these two solutions provided a new avenue for imaging a pediatric patient who was in pain, with a direct impact on patient care. These same benefits can also be realized in adult patients in pain who are frequently difficult to image.