A
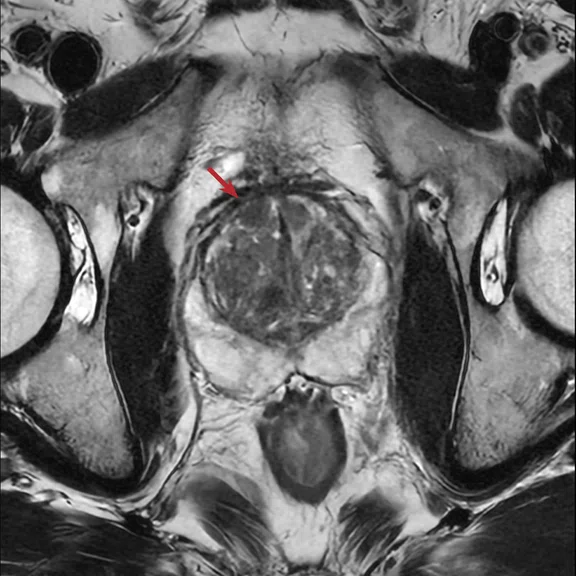
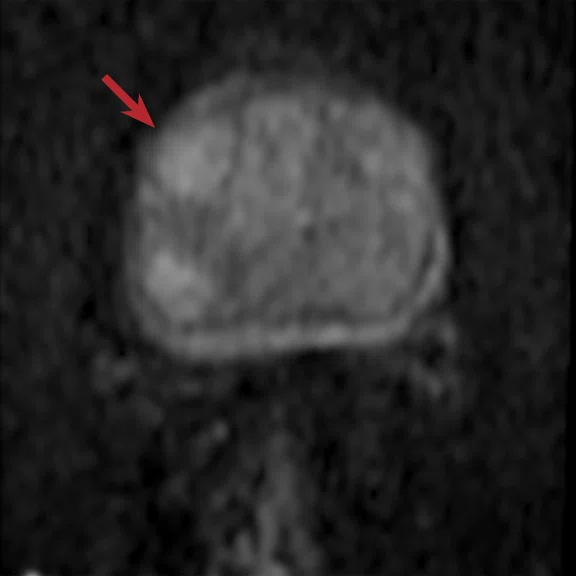
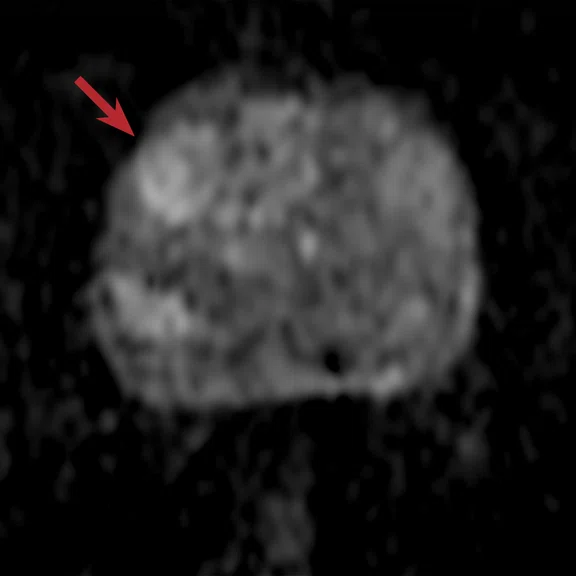
Figure 1.
(A) Axial T2 with AIR™ Recon DL, 0.5 x 0.6 x 3 mm, 2:04 min and (B) coronal T2 with AIR™ Recon DL, 0.4 x 0.6 x 3 mm, 2:42 min. Axial DWI FOCUS with AIR™ Recon DL, 1.8 x 1.3 x 3 mm, 5:11 min. (C) b50, (D) b150, (E) b990, (F) b1500 and (G) ADC. Note how the signal intensity changes as the b-value increases (arrows) and corresponds with the hypointense signal on the ADC.
B
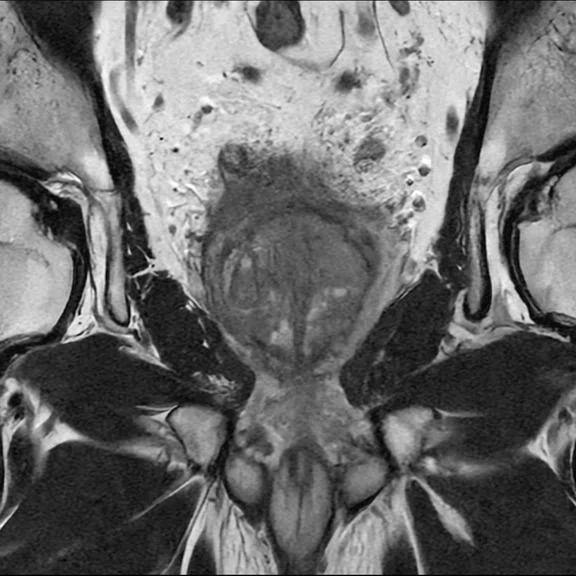
Figure 1.
(A) Axial T2 with AIR™ Recon DL, 0.5 x 0.6 x 3 mm, 2:04 min and (B) coronal T2 with AIR™ Recon DL, 0.4 x 0.6 x 3 mm, 2:42 min. Axial DWI FOCUS with AIR™ Recon DL, 1.8 x 1.3 x 3 mm, 5:11 min. (C) b50, (D) b150, (E) b990, (F) b1500 and (G) ADC. Note how the signal intensity changes as the b-value increases (arrows) and corresponds with the hypointense signal on the ADC.
1. Chatterjee A, Gallan AJ, He D, et al. Revisiting quantitative multi-parametric MRI of benign prostatic hyperplasia and its differentiation from transition zone cancer. Abdom Radiol (NY). 2019 Jun;44(6):2233-2243.
2. Chatterjee A, Tokdemir S, Gallan AJ, et al. Multiparametric MRI Features and Pathologic Outcome of Wedge-Shaped Lesions in the Peripheral Zone on T2-Weighted Images of the Prostate. AJR Am J Roentgenol. 2019 Jan;212(1):124-129.
A
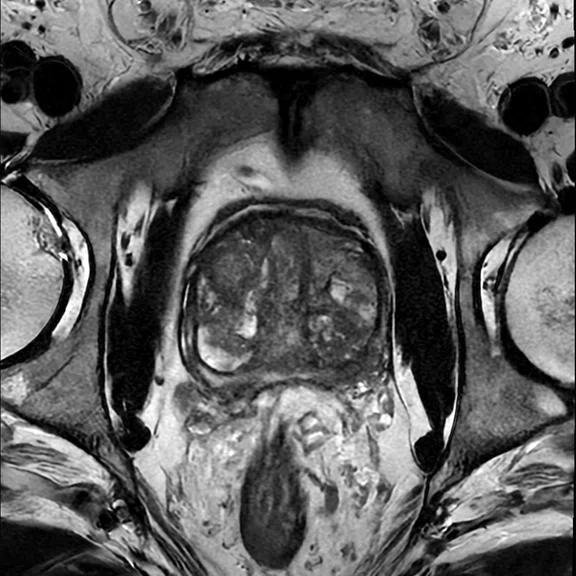
Figure 2.
(A) Axial T2 FSE, 0.5 x 0.6 x 3 mm, 2:19 min.; (B-D) axial FOCUS DWI, 1.8 x 1.3 x 3 mm, 6:42 min., (B) b150, (C) b990 and (D) b1500. Note how the signal intensity changes as the b-value increases (arrows).
B
Figure 2.
(A) Axial T2 FSE, 0.5 x 0.6 x 3 mm, 2:19 min.; (B-D) axial FOCUS DWI, 1.8 x 1.3 x 3 mm, 6:42 min., (B) b150, (C) b990 and (D) b1500. Note how the signal intensity changes as the b-value increases (arrows).
C
Figure 2.
(A) Axial T2 FSE, 0.5 x 0.6 x 3 mm, 2:19 min.; (B-D) axial FOCUS DWI, 1.8 x 1.3 x 3 mm, 6:42 min., (B) b150, (C) b990 and (D) b1500. Note how the signal intensity changes as the b-value increases (arrows).
D
Figure 2.
(A) Axial T2 FSE, 0.5 x 0.6 x 3 mm, 2:19 min.; (B-D) axial FOCUS DWI, 1.8 x 1.3 x 3 mm, 6:42 min., (B) b150, (C) b990 and (D) b1500. Note how the signal intensity changes as the b-value increases (arrows).
C
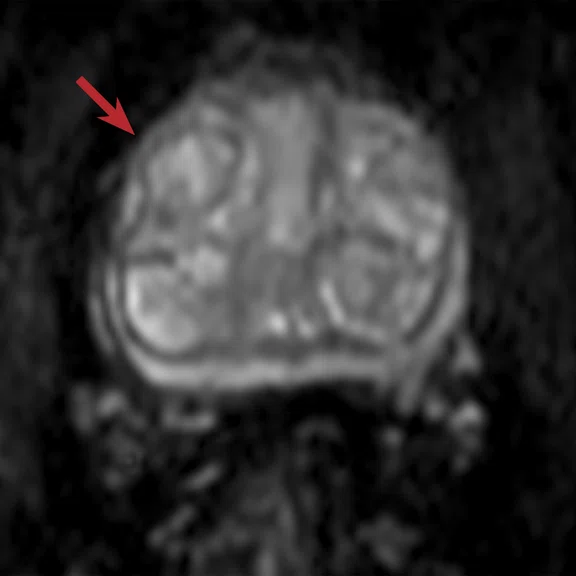
Figure 3.
(A) Axial T2 with AIR™ Recon DL, 0.5 x 0.6 x 3 mm, 2:04 min and (B) coronal T2 with AIR™ Recon DL, 0.4 x 0.6 x 3 mm, 2:42 min. Axial DWI FOCUS with AIR™ Recon DL, 1.8 x 1.3 x 3 mm, 5:11 min. (C) b50, (D) b150, (E) b990, (F) b1500 and (G) ADC. Note how the signal intensity changes as the b-value increases (arrows) and corresponds with the hypointense signal on the ADC.
D
Figure 1.
(A) Axial T2 with AIR™ Recon DL, 0.5 x 0.6 x 3 mm, 2:04 min and (B) coronal T2 with AIR™ Recon DL, 0.4 x 0.6 x 3 mm, 2:42 min. Axial DWI FOCUS with AIR™ Recon DL, 1.8 x 1.3 x 3 mm, 5:11 min. (C) b50, (D) b150, (E) b990, (F) b1500 and (G) ADC. Note how the signal intensity changes as the b-value increases (arrows) and corresponds with the hypointense signal on the ADC.
E
Figure 1.
(A) Axial T2 with AIR™ Recon DL, 0.5 x 0.6 x 3 mm, 2:04 min and (B) coronal T2 with AIR™ Recon DL, 0.4 x 0.6 x 3 mm, 2:42 min. Axial DWI FOCUS with AIR™ Recon DL, 1.8 x 1.3 x 3 mm, 5:11 min. (C) b50, (D) b150, (E) b990, (F) b1500 and (G) ADC. Note how the signal intensity changes as the b-value increases (arrows) and corresponds with the hypointense signal on the ADC.
F
Figure 1.
(A) Axial T2 with AIR™ Recon DL, 0.5 x 0.6 x 3 mm, 2:04 min and (B) coronal T2 with AIR™ Recon DL, 0.4 x 0.6 x 3 mm, 2:42 min. Axial DWI FOCUS with AIR™ Recon DL, 1.8 x 1.3 x 3 mm, 5:11 min. (C) b50, (D) b150, (E) b990, (F) b1500 and (G) ADC. Note how the signal intensity changes as the b-value increases (arrows) and corresponds with the hypointense signal on the ADC.
G
Figure 1.
(A) Axial T2 with AIR™ Recon DL, 0.5 x 0.6 x 3 mm, 2:04 min and (B) coronal T2 with AIR™ Recon DL, 0.4 x 0.6 x 3 mm, 2:42 min. Axial DWI FOCUS with AIR™ Recon DL, 1.8 x 1.3 x 3 mm, 5:11 min. (C) b50, (D) b150, (E) b990, (F) b1500 and (G) ADC. Note how the signal intensity changes as the b-value increases (arrows) and corresponds with the hypointense signal on the ADC.
4. Klotz L, Loblaw A, Sugar L, et al. Active Surveillance Magnetic Resonance Imaging Study (ASIST): Results of a Randomized Multicenter Prospective Trial. Eur Urol. 2019 Feb;75(2):300-309.
5. Klotz L, Pond G, Loblaw A, Sugar L, et al. Randomized Study of Systematic Biopsy Versus Magnetic Resonance Imaging and Targeted and Systematic Biopsy in Men on Active Surveillance (ASIST): 2-year Postbiopsy Follow-up. Eur Urol. 2020 Mar;77(3):311-317.
3. Turkbey B, Rosenkrantz AB, Haider MA, et al. Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur Urol. 2019;76(3):340-351.
‡ Technology in development that represents ongoing research and development efforts. These technologies are not products and may never become products. Not for sale. Not cleared or approved by the US FDA or any other global regulator for commercial availability.


result
PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
IN PRACTICE
AIR technology delivers a bright future for prostate MR imaging
AIR technology delivers a bright future for prostate MR imaging
Prostate MR is growing exponentially, due to the incredibly useful information it provides to help characterize the type of cancer a man has – whether it is slow-growing and indolent or very aggressive. When coupled with regular PSA screening, the sensitivity of MR may also help men avoid unnecessary biopsies or worse, undergo treatment of an indolent cancer.
Prostate MR is growing exponentially, due to the incredibly useful information it provides to help characterize the type of cancer a man has – whether it is slow-growing and indolent or very aggressive. When coupled with regular PSA screening, the sensitivity of MR may also help men avoid unnecessary biopsies or worse, undergo treatment of an indolent cancer.
In 2007, Professor Aytekin Oto, MD, MBA, Chair, Department of Radiology and Chief Physician, Head of the Faculty Practice Plan and Dean for Clinical Affairs, The University of Chicago (UChicago) Medicine, started the institution’s prostate MR program. Even though prostate MR was not available when he underwent training as a resident or fellow, Dr. Oto was instrumental in developing UChicago Medicine’s prostate imaging service, initially on a 1.5T MR system using an endorectal coil. Since that time, prostate MR has significantly evolved and today the center uses 3.0T for the majority of prostate MR exams.
“There have been a lot of technological improvements in MR imaging and our understanding about prostate MR and how it correlates with pathology has also evolved.”
Dr. Aytekin Oto
UChicago Medicine is a world-renowned health system advancing medical science through groundbreaking research. It’s that access to research, funded over the years through grants from the American Cancer Society, the National Institutes of Health (NIH) and the Department of Defense, that has helped Dr. Oto address many of the questions he had during the early days of prostate MR imaging.
Today, UChicago Medicine’s Sanford J. Grossman Center of Excellence in Prostate Imaging and Image Guided Therapy is conducting numerous clinical trials on MR-guided diagnosis, biopsy and treatment. Currently, two key studies Dr. Oto is helping to lead are the development of an imaging-based tool to identify areas for prostate cancer biology (NCT03585660) and MR-guided laser ablation (NCT02766543). The research and clinical trial team consists of physicists, data scientists/informatics specialists, statisticians, pathologists, urologists, radiation oncologists and, of course, radiologists.
Closing the gaps
Correlating MR signals with pathology is one area where Dr. Oto’s research contribution reverberates across the industry.
“If you look at the liver or kidneys across different patients over their life span, they look more or less the same,” Dr. Oto says. “The prostate is such an interesting organ because it looks different in everyone and changes its shape and composition substantially with age.”
Even in the same person, the prostate will change in appearance from age 30 to age 55, he explains. This is especially true in the transition zone, where it is not uncommon for a radiologist to struggle during interpretation.
“A common understanding was that only stromal benign prostatic hyperplasia (BPH) nodules look dark on T2 and ADC images,” Dr. Oto says. “After careful, meticulous radiology-pathology correlation, we could show that completely glandular BPH nodules also look dark on T2 and ADC and can mimic cancer.”1
Another challenge is wedge-shaped T2 hypointense areas in the peripheral zone. The key question is whether these hypointense areas are cancer. UChicago Medicine research led by Dr. Oto demonstrated that 30% of these wedge-shaped T2 hypointense areas can be malignant, while the other 70% could be hemorrhage, inflammation or increased vessels.2
C
D
E
F
G
Figure 1.
(A) Axial T2 with AIR™ Recon DL, 0.5 x 0.6 x 3 mm, 2:04 min and (B) coronal T2 with AIR™ Recon DL, 0.4 x 0.6 x 3 mm, 2:42 min. Axial DWI FOCUS with AIR™ Recon DL, 1.8 x 1.3 x 3 mm, 5:11 min. (C) b50, (D) b150, (E) b990, (F) b1500 and (G) ADC. Note how the signal intensity changes as the b-value increases (arrows) and corresponds with the hypointense signal on the ADC.
Importance of SNR and quality
In MR imaging, SNR is critical. With higher SNR, one can choose to increase resolution or shorten scan time. Historically, however, gaining SNR required longer scan times.
GE Healthcare’s AIR™ Recon DL addresses the compromise between SNR, scan times and image resolution. AIR™ Recon DL is a revolutionary, deep-learning-based image reconstruction technology that provides sharper, clearer and accurate images.
Generating a high-quality prostate MR exam is not necessarily an easy task. The prostate is close to other organs that may move due to respiration and there is often the presence of air (e.g., rectum), both of which can lead to artifacts. In addition to having a different appearance, the prostate also has a variable depth that can change the quality of MR imaging across patients.
The American College of Radiology has worked to improve quality through PI-RADS® v2.13 by addressing both qualitative and quantitative imaging metrics. Dr. Oto is a member of the PI-RADS Committee. His group has worked on a quantitative quality metric for DWI.
“If you look at DWI images with a higher b-value, the signal should never go up with the exception of malignancies. We can show that in about 15-20% of the prostate, the signal goes up with higher b-values, which tells us there is something wrong with that part of the image.”
Dr. Aytekin Oto
Just as he did earlier in his career, Dr. Oto believes many radiologists still continue to learn how to interpret prostate MR as they read more studies. “We are getting better. However, I do feel that I can teach one of our residents or fellows how to read a liver MR exam in a more clear-cut way than a prostate MR exam,” Dr. Oto adds.
This is an area where Dr. Oto believes incorporating artificial intelligence (AI) and deep learning into the daily imaging and reading routine can make a difference in prostate MR.
“We should be able to demonstrate in prospective studies, either using AI or in other quantitative ways, how to look at and read prostate MR,” Dr. Oto says. “An important goal will be using technology to reduce the variability in image acquisition and image interpretation. That is one area I think radiology as a group will need to focus on strategically.”
The use of endorectal coils has long been a key component for acquiring a quality prostate MR exam. Although Dr. Oto believes he can get a better image with the endorectal coil, he also realizes that its use has to be balanced with the additional hardware and personnel cost and, more importantly, patient acceptance and experience. This also includes duration of the prostate MR study.
With overlapping ultra-light, flexible coil elements, AIR™ Coils deliver an MR experience that gets closer to the patient. The technology represents a new standard in coil innovation, enabling a simplified, faster workflow while maintaining excellent image quality.
“I didn’t believe we could scan patients without an endorectal coil until I saw the images from AIR™ Recon DL and the AIR™ Coil,” Dr. Oto says.
UChicago Medicine has conducted an internal quality control study to compare the difference in image quality with and without the endorectal coil. “We felt that the image quality is really good with AIR™ Recon DL and AIR™ Coil, almost comparable to the endorectal coil. The issue we see with other technologies and coils is the variation from patient to patient. With AIR™ Recon DL and AIR™ Coil, that variation based on body habitus or anatomy is not as high,” Dr. Oto adds.
He was convinced based on the T2-weighted images with AIR™ Recon DL because it helped address the key issue of low baseline signal of a normal peripheral zone. Previously, the signal was not sufficiently high, which affected contrast-to-noise ratio (CNR), especially in the presence of cancerous lesions in the peripheral zone. Because the T2-weighted images help the radiologist identify and understand the prostate anatomy, he believes it is the “backbone of prostate MR.”
Even in PI-RADS® v2.1 reporting, Dr. Oto believes AIR™ Recon DL helps make a difference. A good quality MR is reliant on high signal; a better MR exam enables the radiologist to more confidently assign PI-RADS® v2.1 scores.
“A better interpreted study leads to better detection of cancer, and that is what is important,” Dr. Oto adds.
As a result of AIR™ Recon DL, UChicago Medicine introduced non-endorectal coil protocols for prostate MR for the first time in 2020. The endorectal coil is still used for some patients, particularly difficult cases; however, the department is using the non-endorectal coil sequences with greater frequency – which tells Dr. Oto that the combination of the AIR™ Coil and AIR™ Recon DL are generating image quality comparable to the endorectal coil.
Next, he is anticipating the addition of AIR™ Recon DL DWI to see the difference that it can make in diffusion, and believes it will be a very important step forward that “solidifies the role of AIR™ Recon DL in prostate MR.”
Another area that can be problematic is the presence of hip implants in prostate MR. The average age for prostate cancer is similar to the age that men may have implanted hip prostheses.
“That’s another gap that we need to figure out,” Dr. Oto says. “Hip implants can cause a lot of problems, but we don’t have a mechanism to know which patients will be non-diagnostic prior to the MR exam, at this time.”
One possible answer is a new research coil‡ from GE that Dr. Oto and his team will soon study in terms of image quality and signal. This prototype is based off the AIR™ Coil technology and is worn/placed on the patient in a “3D fashion” so that the coil is as close to the region of interest as possible for the best possible signal. Dr. Oto also sees potential for this coil in rectum cancer patients and female pelvis imaging, although studies are still needed to evaluate the efficacy and image quality of the coil.
Similarly, addressing inter-reader variability of prostate MR by introducing a more quantitative approach with standardized image acquisition and interpretation is another area of research interest at UChicago Medicine. Dr. Oto is planning to collaborate with GE to develop a novel technique termed Hybrid Multidimensional MR‡ that will combine T2 and DWI, and correlate the MR signals with tissue percentages that are used in pathology. It is intended as a “virtual pathology” tool that may provide the radiologist with percentages of epithelium and lumen throughout the prostate. If the epithelium increases, as is expected in the pathology of cancer, the radiologist may be able to identify cancers in the prostate using this tool. Through an NIH/NCI grant, UChicago Medicine has conducted a single center study and will next expand the study to several other sites.
Looking forward, Dr. Oto says data on the value of MR as a triage study are being accumulated in other studies, such as the ASIST trial (NCT01354171), as well as whether MR can be used in place of biopsy in patients under surveillance for prostate cancer to identify clinically significant cancers.4,5
“If we want to apply something to a larger population, cost and reimbursement are always an issue. We will need to clearly demonstrate the value of MR to replace biopsies and provide reproducible results. These data are now being collected.”
Dr. Aytekin Oto
For now, however, the future is bright for prostate MR and the value it provides.
“There has been a lot of work through the ACR and at academic centers to demonstrate the appropriateness of prostate MR and giving it the credit it deserves in diagnosing and monitoring prostate cancer so that radiologists can help give men with this diagnosis the best possible quality of life and care,” Dr. Oto concludes.