A
Figure 1.
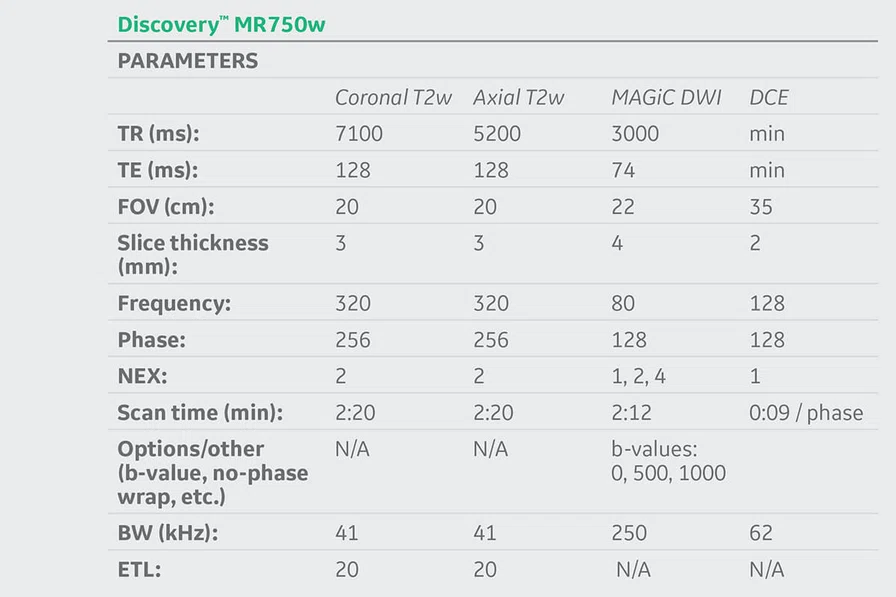
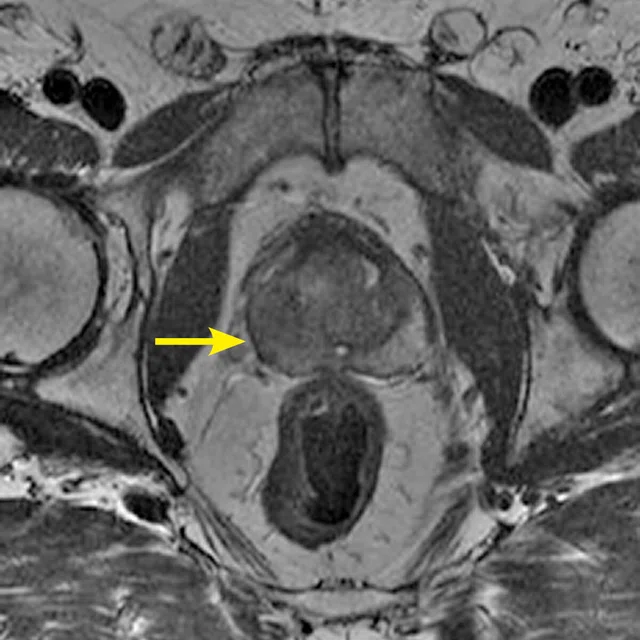
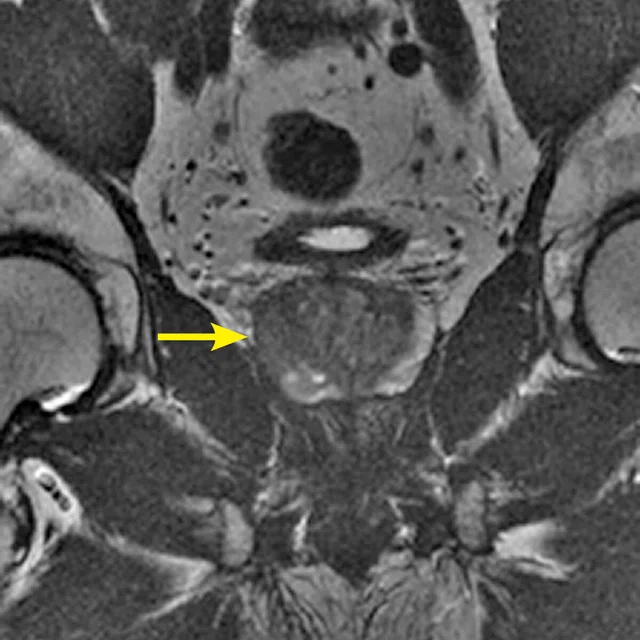
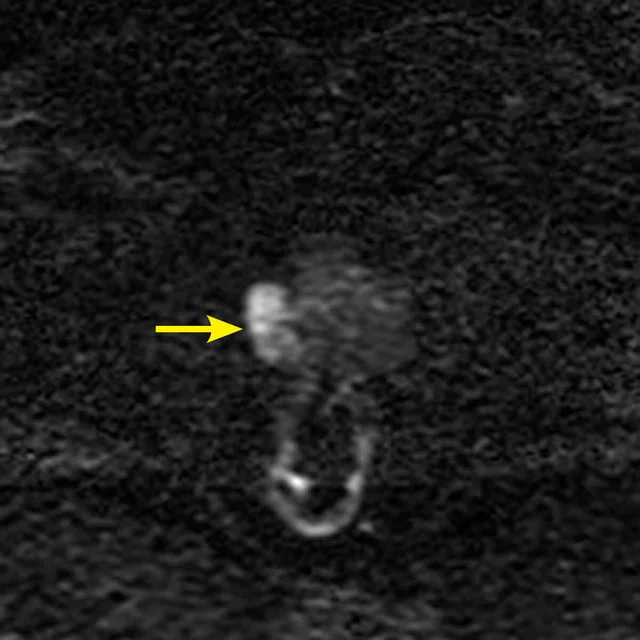
There is a 17 mm observation in the right middle peripheral zone which is hypointense on T2w and shows markedly high signal on synthetic high b-value DWI and markedly low signal on ADC map with early asymmetric and focal avid enhancement (arrows). (A) Axial, and (B) coronal T2w, (C) MAGiC DWI b1500 mm2/sec. DWI, (D) ADC map and (E) T1w 3D GRE from DCE-MR.
B
Figure 1.
There is a 17 mm observation in the right middle peripheral zone which is hypointense on T2w and shows markedly high signal on synthetic high b-value DWI and markedly low signal on ADC map with early asymmetric and focal avid enhancement (arrows). (A) Axial, and (B) coronal T2w, (C) MAGiC DWI b1500 mm2/sec. DWI, (D) ADC map and (E) T1w 3D GRE from DCE-MR.
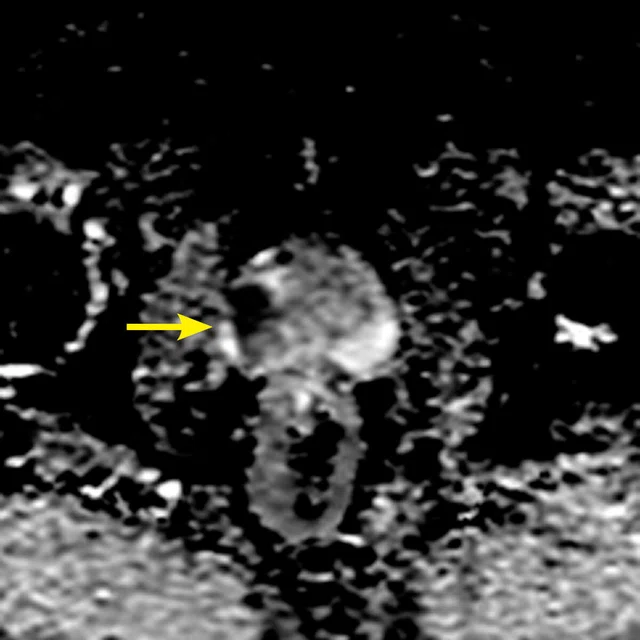
C
Figure 1.
There is a 17 mm observation in the right middle peripheral zone which is hypointense on T2w and shows markedly high signal on synthetic high b-value DWI and markedly low signal on ADC map with early asymmetric and focal avid enhancement (arrows). (A) Axial, and (B) coronal T2w, (C) MAGiC DWI b1500 mm2/sec. DWI, (D) ADC map and (E) T1w 3D GRE from DCE-MR.
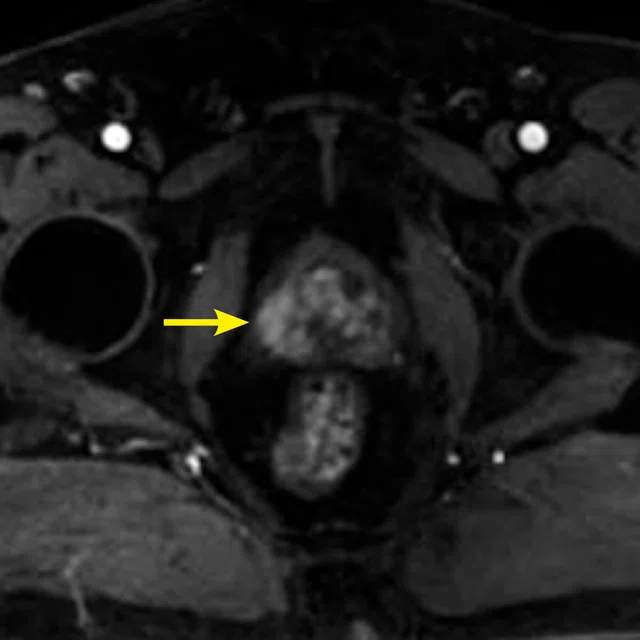
D
Figure 1.
There is a 17 mm observation in the right middle peripheral zone which is hypointense on T2w and shows markedly high signal on synthetic high b-value DWI and markedly low signal on ADC map with early asymmetric and focal avid enhancement (arrows). (A) Axial, and (B) coronal T2w, (C) MAGiC DWI b1500 mm2/sec. DWI, (D) ADC map and (E) T1w 3D GRE from DCE-MR.
E
Figure 1.
There is a 17 mm observation in the right middle peripheral zone which is hypointense on T2w and shows markedly high signal on synthetic high b-value DWI and markedly low signal on ADC map with early asymmetric and focal avid enhancement (arrows). (A) Axial, and (B) coronal T2w, (C) MAGiC DWI b1500 mm2/sec. DWI, (D) ADC map and (E) T1w 3D GRE from DCE-MR.
1 Purysko AS, Rosenkrantz AB, Barentsz JO, Weinreb JC, Macura KJ. PI-RADS Version 2: A Pictorial Update. Radiographics. 2016 Sep-Oct;36(5):1354-72.
2 Niu XK, Chen XH, Chen ZF, Chen L, Li J Peng T. Diagnostic Performance of Biparametric MRI for Detection of Prostate Cancer: A Systematic Review and Meta-Analysis. AJR Am J Roentgenol. 2018 Aug;211(2):369-378.
2 Niu XK, Chen XH, Chen ZF, Chen L, Li J Peng T. Diagnostic Performance of Biparametric MRI for Detection of Prostate Cancer: A Systematic Review and Meta-Analysis. AJR Am J Roentgenol. 2018 Aug;211(2):369-378.
3 van der Leest M, Israël B, Cornel EB, et al. High Diagnostic Performance of Short Magnetic Resonance Imaging Protocols for Prostate Cancer Detection in Biopsy-naïve Men: The Next Step in Magnetic Resonance Imaging Accessibility. Eur Urol. 2019 Jun 2. pii: S0302- 2838(19)30436-1.
3 van der Leest M, Israël B, Cornel EB, et al. High Diagnostic Performance of Short Magnetic Resonance Imaging Protocols for Prostate Cancer Detection in Biopsy-naïve Men: The Next Step in Magnetic Resonance Imaging Accessibility. Eur Urol. 2019 Jun 2. pii: S0302- 2838(19)30436-1.
4 Kasivisvanathan V, Rannikko AS, Borghi M, et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 2018;378:1767e77.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
CASE STUDIES
Fast MR prostate protocol in less than 15 minutes
Fast MR prostate protocol in less than 15 minutes
By Nicola Schieda, MD, FRCPC, Associate Professor of Radiology and Director of Abdominal and Pelvic MRI and Prostate Imaging, The Ottawa Hospital, Ottawa, Canada
The introduction of the Prostate Imaging Reporting and Data System (PI-RADS®) for prostate MR in 2012 has led to more standardized acquisition, interpretation and reporting of prostate MR. The revised PI-RADS® Version 2 and Version 2.1 have improved upon the original PI-RADS® and, based on multiparametric (mp) MR imaging findings, enable assessment of the level of suspicion that an MR abnormality represents a clinically significant cancer.1
After starting our MR prostate program in 2012 where we performed approximately 85 studies per year, our volume has grown exponentially to over 2,000 exams per year. Our initial protocol was approximately 40 minutes and was abbreviated to our main protocol which was approximately 30 minutes and included: localizers, coronal T2-weighted SSFSE, three planes of T2-weighted FRFSE, axial T1-weighted in-plane (IP) and out-of-plane (OP), conventional DWI including acquired high b-value (NEX 10), DCE (5 minutes) and large field-of-view (FOV) T1 weighted LAVA Flex post-contrast sequences.
In autumn of 2018, we switched to a pseudo-fast protocol using conventional DWI by eliminating sequences (namely multiplanar T2-weighted FRFSE and elimination of large FOV imaging). This reduced scan time to under 20 minutes.
To further improve scan times, in March 2019 we introduced MAGiC DWI, which included calculated (rather than acquired) high b-value DWI. For approximately one month, patients were evaluated with both conventional and synthetic DWI, and our observations were similar image quality and artifacts on ADC map images, but with improved contrast on the synthetic high b-value DWI compared to the conventional acquisition with tumor-to background contrast improvements.
In April 2019, we fully converted patients who were undergoing prostate MR for pre-biopsy assessment, active surveillance or with previous negative biopsy but persistent concern for possible cancer to a fast mpMR protocol using MAGiC DWI. We have performed over 250 fast mpMR exams so far.
The fast MR reduced scan time from the conventional sequence by more than half. We can scan patients door-to-door in under 15 minutes. We book four patients per hour. The doubling of efficiency enabled us to manage precious resource allocation, which is limited in Canada, and provide access for increased utilization of prostate MR (volume doubled from 2016 to 2019) without an increase in operational hours or blocking access to MR for other patients.
Patient history
A 64-year-old male with Prostate Serum Antigen (PSA) 12.3 ng/mL undergoing fast prostate MR for targeting pre-biopsy.
Results
A low T2-weighted lesion in the peripheral zone with marked restricted diffusion and avid early asymmetric enhancement was noted. The observation was characterized as a PI-RADS® v2.1 category 5 (clinically significant cancer is very likely to be present). Subsequent transrectal ultrasound-MR fusion biopsy confirmed Gleason 4+3=7 prostate cancer.
Technique
Our first attempt at fast MR included one plane of T2-weighted imaging (the axial plane). Our experience, which is in line with PI RADS® v2.1 recommendations, is that a proportion of transition zone nodules may appear partially or incompletely circumscribed, partially or incompletely encapsulated, or show blurred or indistinct margins due to volume averaging effects when using only axial T2-weighted images. PI-RADS® v2.1 suggests at least one additional plane of T2-weighted imaging in addition to the axial plane, and we have found that this strategy improves our characterization of transition zone nodules. The use of a T2 weighted 3D sequence (i.e., Cube) is another strategy and, when used with a novel time saving technique that combines parallel imaging and compressed sensing (i.e., HyperSense), could be a real alternative to a conventional T2-weighted 2D sequence with expected marked reduction in scan time and artifact.
Discussion
In our experience using the fast mpMR technique, we found no difference in the detection of cancers overall but subjectively improved contrast-to-noise on synthetic high b-value DWI, improving reader confidence for detection of prostate cancers. There was also no change in biopsy rates or accuracy; however, we did experience improved reader confidence when evaluating potential tumor to background on the synthetic high b-value images.
More importantly, we doubled our capacity to accommodate a significant increase in requests for prostate MR with no change in operational hours or funding, or an increase in wait times. Patients are very satisfied with the shorter exams.
The accuracy of the fast mpMR protocol is not better than the standard mpMR protocol; however, it is not inferior in terms of cancer detection rates, and that is important. Based on the results from the PRECISION trial4, we could infer that in the 30 percent of men who have a negative mpMR and are undergoing imaging for elevated PSA or abnormal DRE, biopsy could be avoided in the future if further validation of this practice becomes available, thus saving costs and potential morbidity for the patient.
At The Ottawa Hospital, we are evaluating switching to a bpMR protocol for most patients and recalling the subset of patients who require DCE-MR if we believe that may help to improve the exam quality (e.g., artifact compromising DWI, PI-RADS® 3 peripheral zone observation). More vigilant protocolling of cases, i.e., identifying patients with metallic implants in the pelvis and those with suspected local recurrence of tumor after therapy, would further delineate which patients would require GBCA at the time of their first exam.
Based on our experience in prostate MR, we are considering implementing MAGiC DWI into all of our pelvic MR protocols, especially those for rectal and cervical cancer assessment.
Other institutions that evaluate synthetic DWI sequences such as MAGiC DWI may also discover what I have found: more is not better. Patient tolerance for MR exams decreases over time and the shorter the exam, the better success in reducing patient-induced motion artifacts. The results from our adoption of the synthetic DWI, combined with our own reductions in sequences, incorporate engineering advances with practical experience to improve exam quality, shorten exam times, increase patient tolerance and enhance access/capacity while maintaining diagnostic accuracy.
Figure 1.
There is a 17 mm observation in the right middle peripheral zone which is hypointense on T2w and shows markedly high signal on synthetic high b-value DWI and markedly low signal on ADC map with early asymmetric and focal avid enhancement (arrows). (A) Axial, and (B) coronal T2w, (C) MAGiC DWI b1500 mm2/sec. DWI, (D) ADC map and (E) T1w 3D GRE from DCE-MR.
Further reductions in scan time could be achieved if using an abbreviated biparametric (bp) MR rather than an mpMR exam. The main difference between bpMR and mpMR is the use of gadolinium-based contrast agents (GBCA) and dynamic contrast enhanced (DCE) imaging in the later protocol.
The use of GBCA for DCE in prostate MR is a controversial topic due to concerns of gadolinium retention, higher associated costs and longer scan times. In general, there has been increased scrutiny regarding the liberal use of GBCA for many MR exams, leading to interest in bpMR.
A meta-analysis of 33 studies found that the pooled specificity between mpMR and bpMR were not significantly different.2 However, bpMR had a statistically significant lower sensitivity (80 percent compared to 85 percent) that the authors suggest may be attributed to the ability to detect subtle lesions with DCE-MR, even though DCE has a limited role in the diagnosis of prostate cancer.2
A recent study comparing mpMR, bpMR and a “fast” (monoplanar) bpMR in 626 biopsy-naïve men reported the same sensitivity (95 percent) for all protocols and a specificity of 65 percent for the “fast” bpMR and 69 percent for both the bpMR and mpMR.3 Inter reader agreement was 90 percent for the fast bpMR and 93 percent for the bpMR.3 The authors reported that both bpMR protocols had an equal detection rate of high-grade prostate cancer equivalent to mpMR, and the “fast” bpMR had a high negative predictive value of 97 percent. However, there are added benefits of the “fast” bpMR, such as the ability to increase prostate MR capacity at a lower cost and the avoidance of potential risks associated with GBCA administration.3
We presently do not perform bpMR at our institution and all patients undergo a comprehensive mpMR exam that is fully compliant with PI-RADS® v2.1 guidelines, including two planes of T2-weighted imaging, axial DWI and axial DCE. In our own experience, we estimate DCE is required in the following situations: approximately 10 percent of cases where DWI may be compromised by artifact (e.g., from rectal gas, hip prosthesis); in PI-RADS® v2.1 assessment category 3 lesions in the peripheral zone; and in patients who have undergone therapy (e.g., radical prostatectomy, radiotherapy) and there is concern for local recurrence. We are actively considering the use of bpMR with the strategy of calling patients back when DCE-MR is required; however, we continue to perform mpMR in all patients. For patients referred for local staging of a known significant prostate cancer, we perform a comprehensive staging mpMR, which is acquired in under 30 minutes but includes all three planes of T2 weighted imaging and large FOV sequences of the whole pelvis to assess for lymphadenopathy and the pelvic marrow.