A
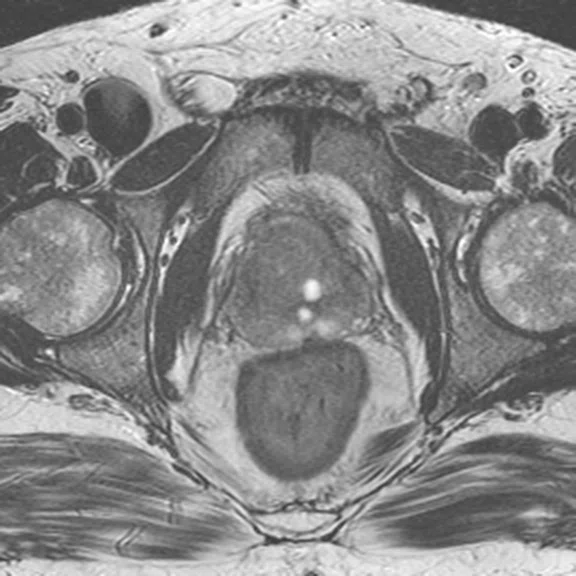
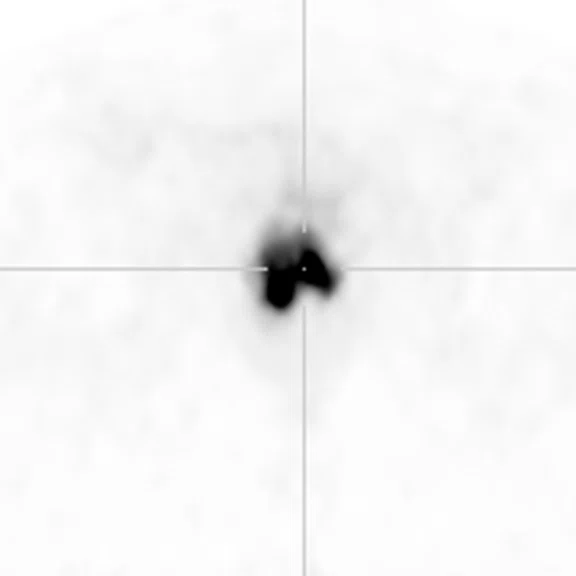
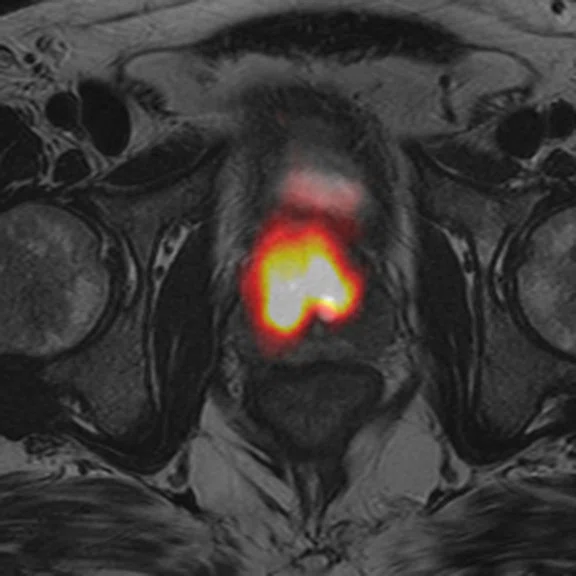
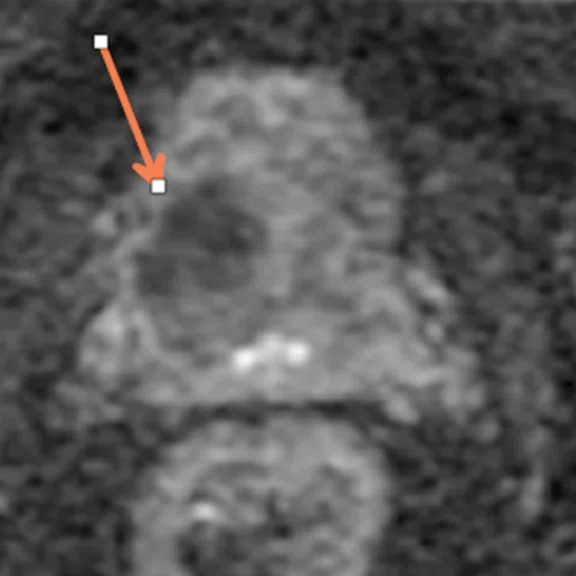
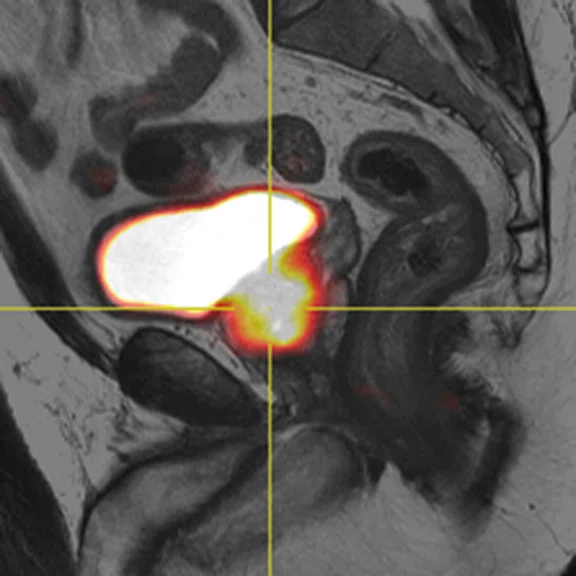
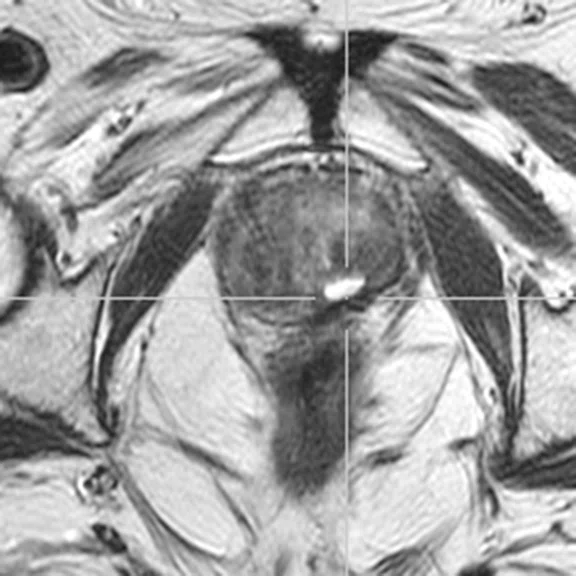
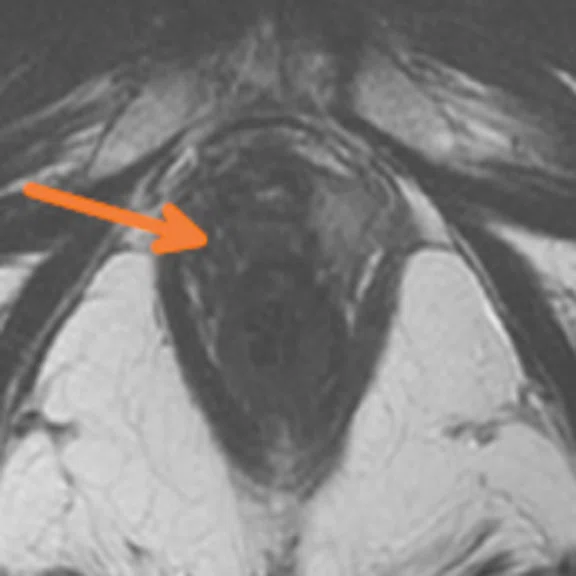
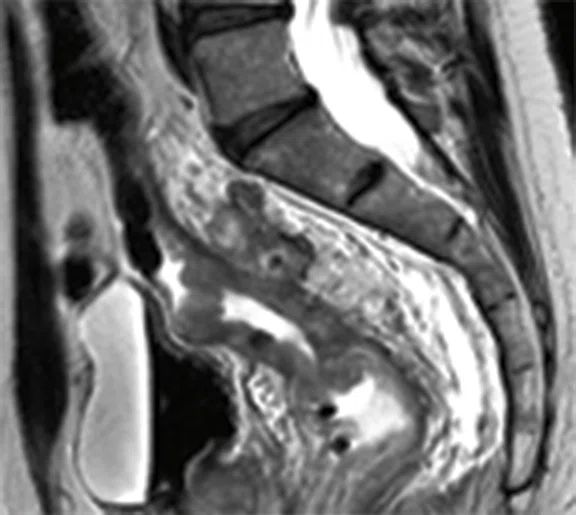
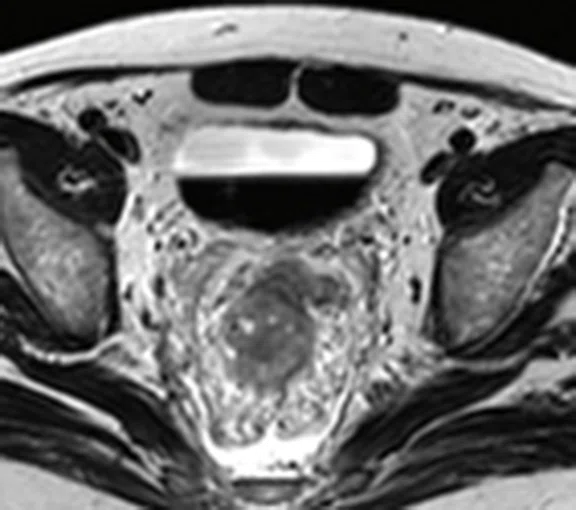
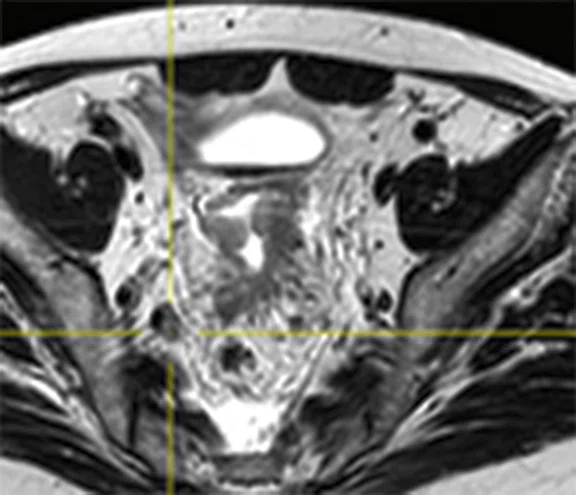
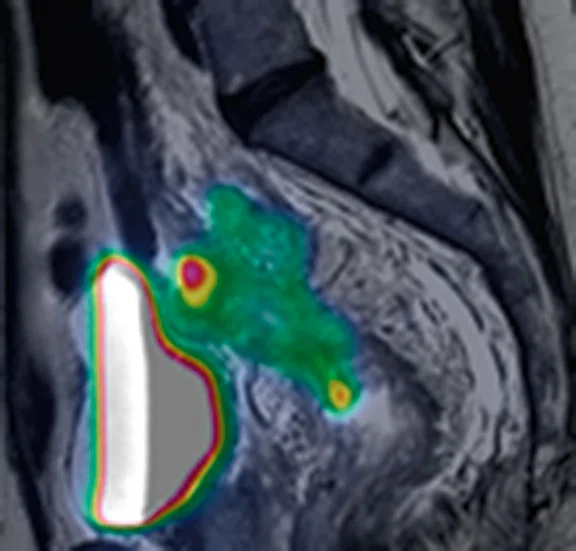
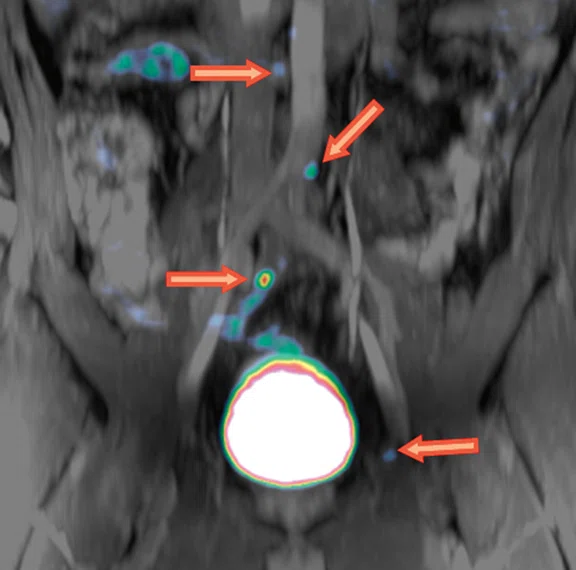
Figure 1.
A 57-year-old male with recently diagnosed prostatic adenocarcinoma was referred for evaluation of suspicious lymph nodes detected in an MR exam. (A, E) T2w with (B, F) corresponding PET and (C, G) fused PET/MR; (D) ADC; (H) perfusion; and (I) T2w (J) fused with PET. Exam confirmed lymph node involvement. MR exam confirmed the lymph nodes were not metastatic.
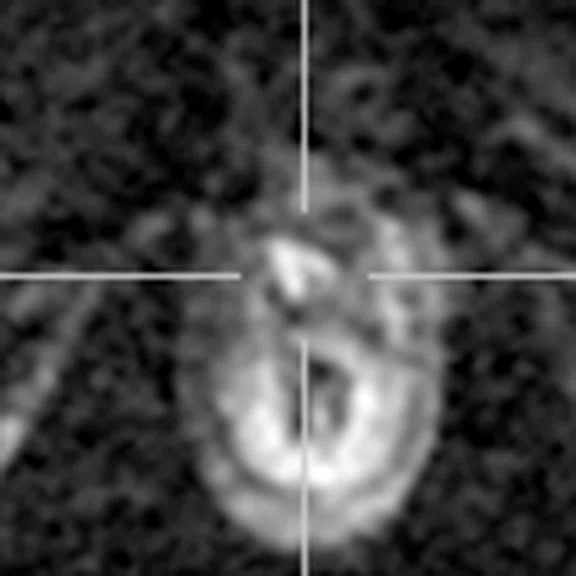
B
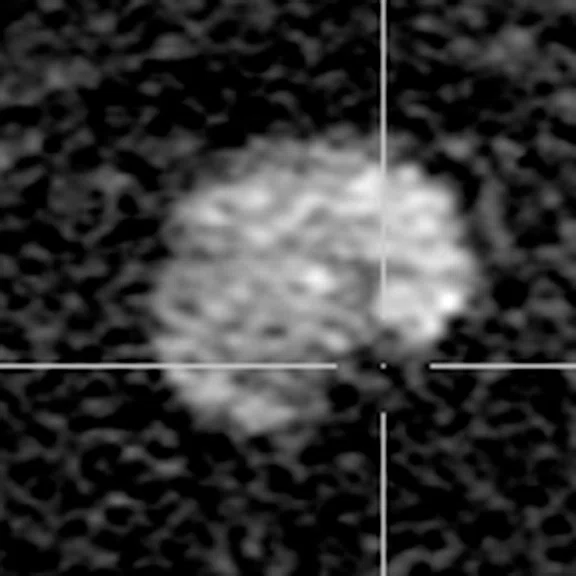
Figure 1.
A 57-year-old male with recently diagnosed prostatic adenocarcinoma was referred for evaluation of suspicious lymph nodes detected in an MR exam. (A, E) T2w with (B, F) corresponding PET and (C, G) fused PET/MR; (D) ADC; (H) perfusion; and (I) T2w (J) fused with PET. Exam confirmed lymph node involvement. MR exam confirmed the lymph nodes were not metastatic.
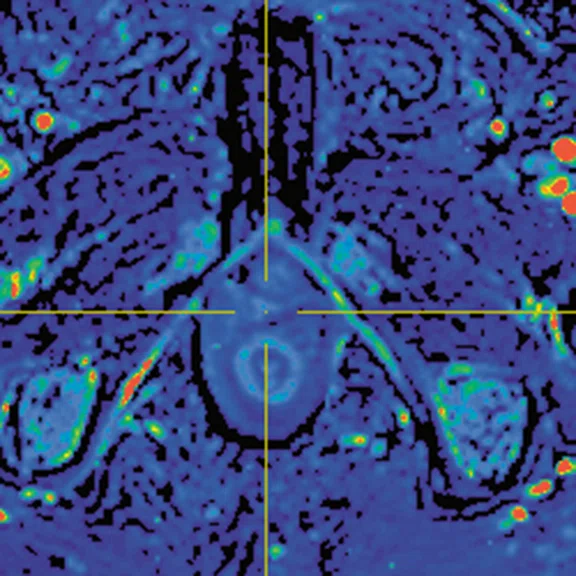
C
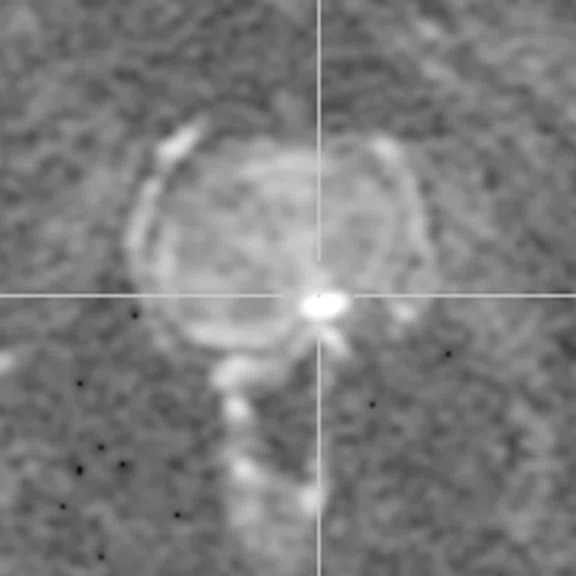
Figure 1.
A 57-year-old male with recently diagnosed prostatic adenocarcinoma was referred for evaluation of suspicious lymph nodes detected in an MR exam. (A, E) T2w with (B, F) corresponding PET and (C, G) fused PET/MR; (D) ADC; (H) perfusion; and (I) T2w (J) fused with PET. Exam confirmed lymph node involvement. MR exam confirmed the lymph nodes were not metastatic.
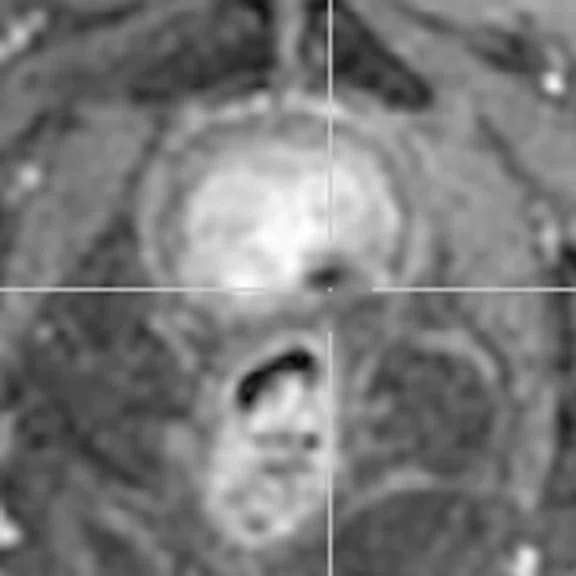
D
Figure 1.
A 57-year-old male with recently diagnosed prostatic adenocarcinoma was referred for evaluation of suspicious lymph nodes detected in an MR exam. (A, E) T2w with (B, F) corresponding PET and (C, G) fused PET/MR; (D) ADC; (H) perfusion; and (I) T2w (J) fused with PET. Exam confirmed lymph node involvement. MR exam confirmed the lymph nodes were not metastatic.
E
Figure 1.
A 57-year-old male with recently diagnosed prostatic adenocarcinoma was referred for evaluation of suspicious lymph nodes detected in an MR exam. (A, E) T2w with (B, F) corresponding PET and (C, G) fused PET/MR; (D) ADC; (H) perfusion; and (I) T2w (J) fused with PET. Exam confirmed lymph node involvement. MR exam confirmed the lymph nodes were not metastatic.
F
Figure 1.
A 57-year-old male with recently diagnosed prostatic adenocarcinoma was referred for evaluation of suspicious lymph nodes detected in an MR exam. (A, E) T2w with (B, F) corresponding PET and (C, G) fused PET/MR; (D) ADC; (H) perfusion; and (I) T2w (J) fused with PET. Exam confirmed lymph node involvement. MR exam confirmed the lymph nodes were not metastatic.
G
Figure 1.
A 57-year-old male with recently diagnosed prostatic adenocarcinoma was referred for evaluation of suspicious lymph nodes detected in an MR exam. (A, E) T2w with (B, F) corresponding PET and (C, G) fused PET/MR; (D) ADC; (H) perfusion; and (I) T2w (J) fused with PET. Exam confirmed lymph node involvement. MR exam confirmed the lymph nodes were not metastatic.
H
Figure 1.
A 57-year-old male with recently diagnosed prostatic adenocarcinoma was referred for evaluation of suspicious lymph nodes detected in an MR exam. (A, E) T2w with (B, F) corresponding PET and (C, G) fused PET/MR; (D) ADC; (H) perfusion; and (I) T2w (J) fused with PET. Exam confirmed lymph node involvement. MR exam confirmed the lymph nodes were not metastatic.
I
Figure 1.
A 57-year-old male with recently diagnosed prostatic adenocarcinoma was referred for evaluation of suspicious lymph nodes detected in an MR exam. (A, E) T2w with (B, F) corresponding PET and (C, G) fused PET/MR; (D) ADC; (H) perfusion; and (I) T2w (J) fused with PET. Exam confirmed lymph node involvement. MR exam confirmed the lymph nodes were not metastatic.
J
Figure 1.
A 57-year-old male with recently diagnosed prostatic adenocarcinoma was referred for evaluation of suspicious lymph nodes detected in an MR exam. (A, E) T2w with (B, F) corresponding PET and (C, G) fused PET/MR; (D) ADC; (H) perfusion; and (I) T2w (J) fused with PET. Exam confirmed lymph node involvement. MR exam confirmed the lymph nodes were not metastatic.
A
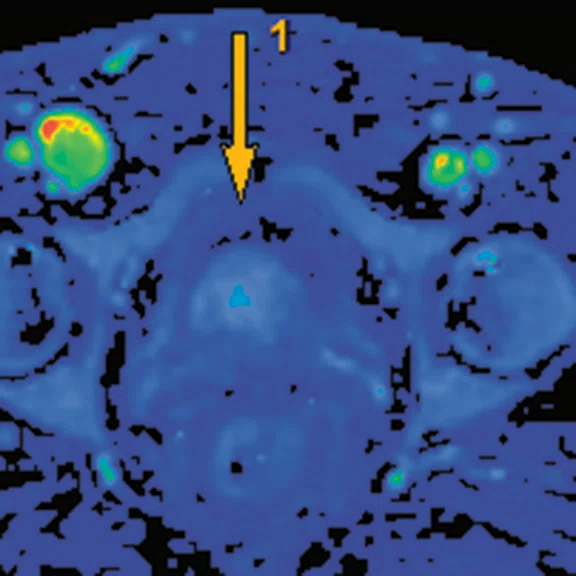
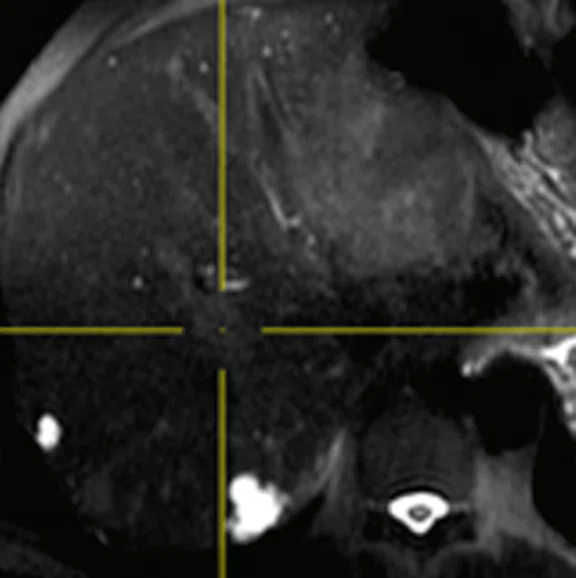
Figure 2.
A 76-year-old male previously treated with high intensity focused ultrasound for prostatic cancer and presenting with recently elevated PSA levels was referred to PET/MR to evaluate treatment response. The MR exam demonstrated good treatment of the local prostatic tumor, however, pelvic node metastases were detected, indicating site of biochemical recurrence. (A) T2w, (B) DWI, (C) ADC, (D) post-contrast ADC, (E) perfusion, (F-I) fused PET/MR and (J) whole-body PET .
B
Figure 2.
A 76-year-old male previously treated with high intensity focused ultrasound for prostatic cancer and presenting with recently elevated PSA levels was referred to PET/MR to evaluate treatment response. The MR exam demonstrated good treatment of the local prostatic tumor, however, pelvic node metastases were detected, indicating site of biochemical recurrence. (A) T2w, (B) DWI, (C) ADC, (D) post-contrast ADC, (E) perfusion, (F-I) fused PET/MR and (J) whole-body PET .
C
Figure 2.
A 76-year-old male previously treated with high intensity focused ultrasound for prostatic cancer and presenting with recently elevated PSA levels was referred to PET/MR to evaluate treatment response. The MR exam demonstrated good treatment of the local prostatic tumor, however, pelvic node metastases were detected, indicating site of biochemical recurrence. (A) T2w, (B) DWI, (C) ADC, (D) post-contrast ADC, (E) perfusion, (F-I) fused PET/MR and (J) whole-body PET .
D
Figure 3.
A 76-year-old male previously treated with high intensity focused ultrasound for prostatic cancer and presenting with recently elevated PSA levels was referred to PET/MR to evaluate treatment response. The MR exam demonstrated good treatment of the local prostatic tumor, however, pelvic node metastases were detected, indicating site of biochemical recurrence. (A) T2w, (B) DWI, (C) ADC, (D) post-contrast ADC, (E) perfusion, (F-I) fused PET/MR and (J) whole-body PET .
E
Figure 2.
A 76-year-old male previously treated with high intensity focused ultrasound for prostatic cancer and presenting with recently elevated PSA levels was referred to PET/MR to evaluate treatment response. The MR exam demonstrated good treatment of the local prostatic tumor, however, pelvic node metastases were detected, indicating site of biochemical recurrence. (A) T2w, (B) DWI, (C) ADC, (D) post-contrast ADC, (E) perfusion, (F-I) fused PET/MR and (J) whole-body PET .
F
Figure 2.
A 76-year-old male previously treated with high intensity focused ultrasound for prostatic cancer and presenting with recently elevated PSA levels was referred to PET/MR to evaluate treatment response. The MR exam demonstrated good treatment of the local prostatic tumor, however, pelvic node metastases were detected, indicating site of biochemical recurrence. (A) T2w, (B) DWI, (C) ADC, (D) post-contrast ADC, (E) perfusion, (F-I) fused PET/MR and (J) whole-body PET .
G
Figure 2.
A 76-year-old male previously treated with high intensity focused ultrasound for prostatic cancer and presenting with recently elevated PSA levels was referred to PET/MR to evaluate treatment response. The MR exam demonstrated good treatment of the local prostatic tumor, however, pelvic node metastases were detected, indicating site of biochemical recurrence. (A) T2w, (B) DWI, (C) ADC, (D) post-contrast ADC, (E) perfusion, (F-I) fused PET/MR and (J) whole-body PET .
H
Figure 2.
A 76-year-old male previously treated with high intensity focused ultrasound for prostatic cancer and presenting with recently elevated PSA levels was referred to PET/MR to evaluate treatment response. The MR exam demonstrated good treatment of the local prostatic tumor, however, pelvic node metastases were detected, indicating site of biochemical recurrence. (A) T2w, (B) DWI, (C) ADC, (D) post-contrast ADC, (E) perfusion, (F-I) fused PET/MR and (J) whole-body PET .
I
Figure 2.
A 76-year-old male previously treated with high intensity focused ultrasound for prostatic cancer and presenting with recently elevated PSA levels was referred to PET/MR to evaluate treatment response. The MR exam demonstrated good treatment of the local prostatic tumor, however, pelvic node metastases were detected, indicating site of biochemical recurrence. (A) T2w, (B) DWI, (C) ADC, (D) post-contrast ADC, (E) perfusion, (F-I) fused PET/MR and (J) whole-body PET .
J
Figure 2.
A 76-year-old male previously treated with high intensity focused ultrasound for prostatic cancer and presenting with recently elevated PSA levels was referred to PET/MR to evaluate treatment response. The MR exam demonstrated good treatment of the local prostatic tumor, however, pelvic node metastases were detected, indicating site of biochemical recurrence. (A) T2w, (B) DWI, (C) ADC, (D) post-contrast ADC, (E) perfusion, (F-I) fused PET/MR and (J) whole-body PET .
A
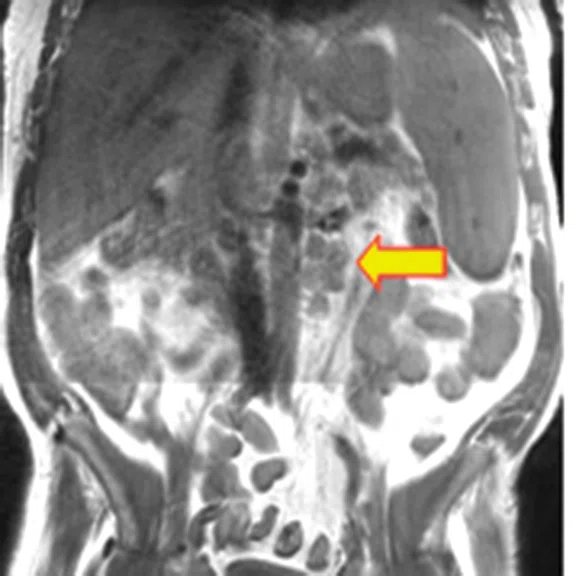
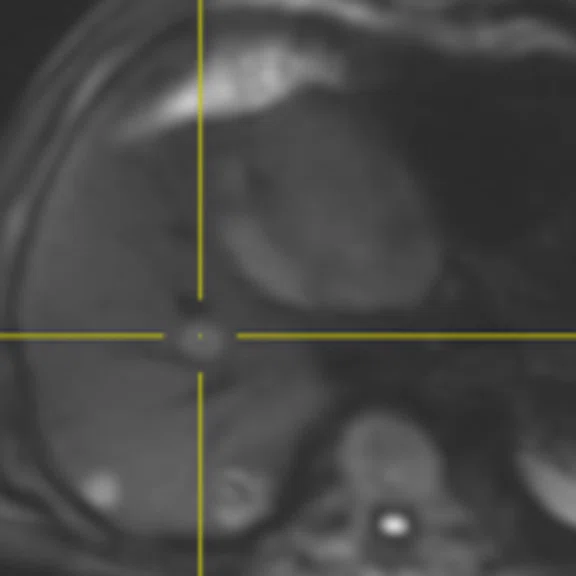
Figure 3.
A 70-year-old male with history of radical prostatectomy presenting with high PSA reaching 1.99 ng/ml referred for PET/MR with suspected biochemical recurrence. (A) T2w, (B) ADC, (C) perfusion, (D-F) fused PET (G) FLAIR and (H, I) whole-body PET. Biochemical recurrence at the bladder neck was depicted by mpMRI and was concordant with PSMA-PET. (F, G) Distant brain metastasis was noted.
B
Figure 3.
A 70-year-old male with history of radical prostatectomy presenting with high PSA reaching 1.99 ng/ml referred for PET/MR with suspected biochemical recurrence. (A) T2w, (B) ADC, (C) perfusion, (D-F) fused PET (G) FLAIR and (H, I) whole-body PET. Biochemical recurrence at the bladder neck was depicted by mpMRI and was concordant with PSMA-PET. (F, G) Distant brain metastasis was noted.
C
Figure 3.
A 70-year-old male with history of radical prostatectomy presenting with high PSA reaching 1.99 ng/ml referred for PET/MR with suspected biochemical recurrence. (A) T2w, (B) ADC, (C) perfusion, (D-F) fused PET (G) FLAIR and (H, I) whole-body PET. Biochemical recurrence at the bladder neck was depicted by mpMRI and was concordant with PSMA-PET. (F, G) Distant brain metastasis was noted.
D
Figure 3.
A 70-year-old male with history of radical prostatectomy presenting with high PSA reaching 1.99 ng/ml referred for PET/MR with suspected biochemical recurrence. (A) T2w, (B) ADC, (C) perfusion, (D-F) fused PET (G) FLAIR and (H, I) whole-body PET. Biochemical recurrence at the bladder neck was depicted by mpMRI and was concordant with PSMA-PET. (F, G) Distant brain metastasis was noted.
E
Figure 3.
A 70-year-old male with history of radical prostatectomy presenting with high PSA reaching 1.99 ng/ml referred for PET/MR with suspected biochemical recurrence. (A) T2w, (B) ADC, (C) perfusion, (D-F) fused PET (G) FLAIR and (H, I) whole-body PET. Biochemical recurrence at the bladder neck was depicted by mpMRI and was concordant with PSMA-PET. (F, G) Distant brain metastasis was noted.
F
Figure 3.
A 70-year-old male with history of radical prostatectomy presenting with high PSA reaching 1.99 ng/ml referred for PET/MR with suspected biochemical recurrence. (A) T2w, (B) ADC, (C) perfusion, (D-F) fused PET (G) FLAIR and (H, I) whole-body PET. Biochemical recurrence at the bladder neck was depicted by mpMRI and was concordant with PSMA-PET. (F, G) Distant brain metastasis was noted.
G
Figure 3.
A 70-year-old male with history of radical prostatectomy presenting with high PSA reaching 1.99 ng/ml referred for PET/MR with suspected biochemical recurrence. (A) T2w, (B) ADC, (C) perfusion, (D-F) fused PET (G) FLAIR and (H, I) whole-body PET. Biochemical recurrence at the bladder neck was depicted by mpMRI and was concordant with PSMA-PET. (F, G) Distant brain metastasis was noted.
H
Figure 3.
A 70-year-old male with history of radical prostatectomy presenting with high PSA reaching 1.99 ng/ml referred for PET/MR with suspected biochemical recurrence. (A) T2w, (B) ADC, (C) perfusion, (D-F) fused PET (G) FLAIR and (H, I) whole-body PET. Biochemical recurrence at the bladder neck was depicted by mpMRI and was concordant with PSMA-PET. (F, G) Distant brain metastasis was noted.
I
Figure 3.
A 70-year-old male with history of radical prostatectomy presenting with high PSA reaching 1.99 ng/ml referred for PET/MR with suspected biochemical recurrence. (A) T2w, (B) ADC, (C) perfusion, (D-F) fused PET (G) FLAIR and (H, I) whole-body PET. Biochemical recurrence at the bladder neck was depicted by mpMRI and was concordant with PSMA-PET. (F, G) Distant brain metastasis was noted.
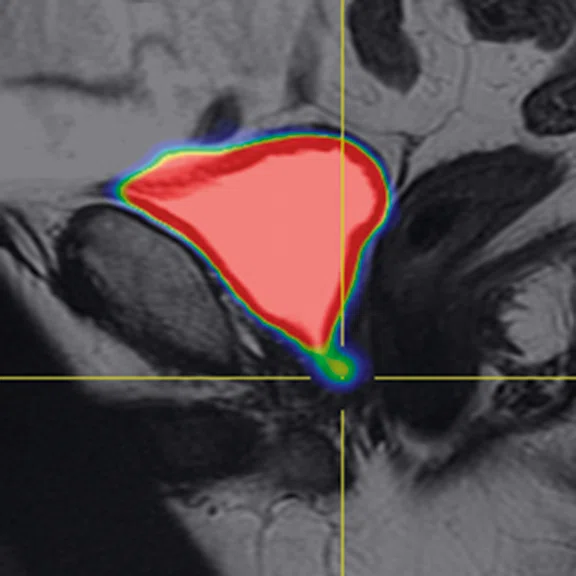
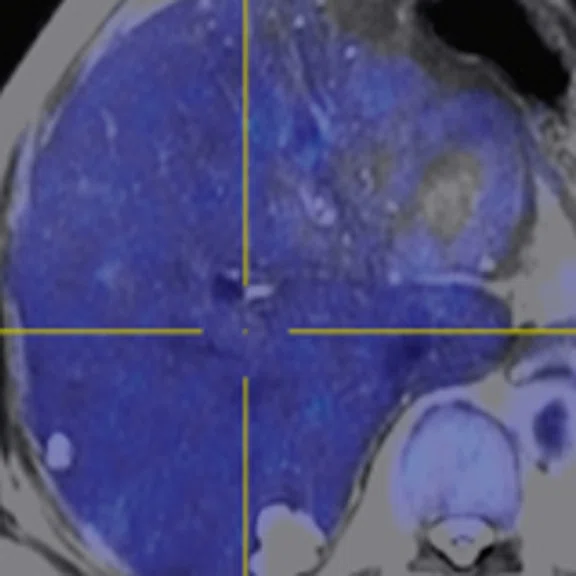
A
Figure 4.
PET/MR provides structural, functional and metabolic data simultaneously in pelvic malignancy cases. (A-C) T2w, (D-F) fused with PET, (G, H) DWI and (I) sagittal T2w. MR facilitates accurate staging because it can depict infiltration of the muscularis propria, mesorectal facial involvement and (I) peritoneal reflection involvement.
B
Figure 4.
PET/MR provides structural, functional and metabolic data simultaneously in pelvic malignancy cases. (A-C) T2w, (D-F) fused with PET, (G, H) DWI and (I) sagittal T2w. MR facilitates accurate staging because it can depict infiltration of the muscularis propria, mesorectal facial involvement and (I) peritoneal reflection involvement.
C
Figure 4.
PET/MR provides structural, functional and metabolic data simultaneously in pelvic malignancy cases. (A-C) T2w, (D-F) fused with PET, (G, H) DWI and (I) sagittal T2w. MR facilitates accurate staging because it can depict infiltration of the muscularis propria, mesorectal facial involvement and (I) peritoneal reflection involvement.
D
Figure 4.
PET/MR provides structural, functional and metabolic data simultaneously in pelvic malignancy cases. (A-C) T2w, (D-F) fused with PET, (G, H) DWI and (I) sagittal T2w. MR facilitates accurate staging because it can depict infiltration of the muscularis propria, mesorectal facial involvement and (I) peritoneal reflection involvement.
E
Figure 4.
PET/MR provides structural, functional and metabolic data simultaneously in pelvic malignancy cases. (A-C) T2w, (D-F) fused with PET, (G, H) DWI and (I) sagittal T2w. MR facilitates accurate staging because it can depict infiltration of the muscularis propria, mesorectal facial involvement and (I) peritoneal reflection involvement.
F
Figure 4.
PET/MR provides structural, functional and metabolic data simultaneously in pelvic malignancy cases. (A-C) T2w, (D-F) fused with PET, (G, H) DWI and (I) sagittal T2w. MR facilitates accurate staging because it can depict infiltration of the muscularis propria, mesorectal facial involvement and (I) peritoneal reflection involvement.
G
Figure 4.
PET/MR provides structural, functional and metabolic data simultaneously in pelvic malignancy cases. (A-C) T2w, (D-F) fused with PET, (G, H) DWI and (I) sagittal T2w. MR facilitates accurate staging because it can depict infiltration of the muscularis propria, mesorectal facial involvement and (I) peritoneal reflection involvement.
H
Figure 4.
PET/MR provides structural, functional and metabolic data simultaneously in pelvic malignancy cases. (A-C) T2w, (D-F) fused with PET, (G, H) DWI and (I) sagittal T2w. MR facilitates accurate staging because it can depict infiltration of the muscularis propria, mesorectal facial involvement and (I) peritoneal reflection involvement.
I
Figure 4.
PET/MR provides structural, functional and metabolic data simultaneously in pelvic malignancy cases. (A-C) T2w, (D-F) fused with PET, (G, H) DWI and (I) sagittal T2w. MR facilitates accurate staging because it can depict infiltration of the muscularis propria, mesorectal facial involvement and (I) peritoneal reflection involvement.
A
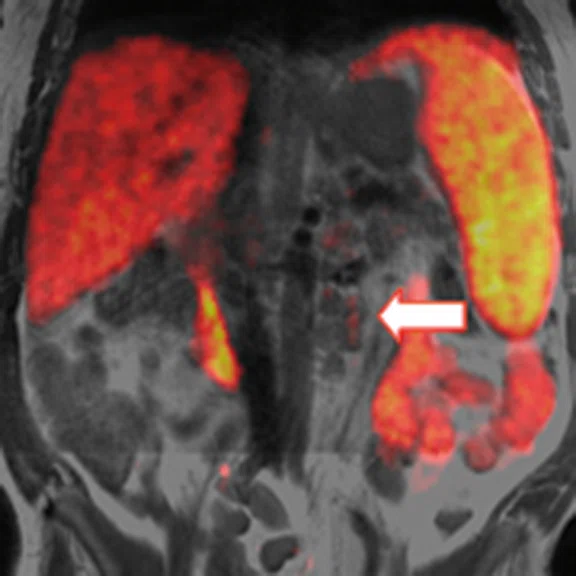
Figure 5.
PET/MR assists with (A) nodal staging in rectal cancer and, because both PET and MR provide whole-body imaging, the evaluation of distant metastases (B-D) in the liver, (E, F) peritoneal and (G-I) lung.
B
Figure 5.
PET/MR assists with (A) nodal staging in rectal cancer and, because both PET and MR provide whole-body imaging, the evaluation of distant metastases (B-D) in the liver, (E, F) peritoneal and (G-I) lung.
C
Figure 5.
PET/MR assists with (A) nodal staging in rectal cancer and, because both PET and MR provide whole-body imaging, the evaluation of distant metastases (B-D) in the liver, (E, F) peritoneal and (G-I) lung.
D
Figure 5.
PET/MR assists with (A) nodal staging in rectal cancer and, because both PET and MR provide whole-body imaging, the evaluation of distant metastases (B-D) in the liver, (E, F) peritoneal and (G-I) lung.
E
Figure 5.
PET/MR assists with (A) nodal staging in rectal cancer and, because both PET and MR provide whole-body imaging, the evaluation of distant metastases (B-D) in the liver, (E, F) peritoneal and (G-I) lung.
F
Figure 5.
PET/MR assists with (A) nodal staging in rectal cancer and, because both PET and MR provide whole-body imaging, the evaluation of distant metastases (B-D) in the liver, (E, F) peritoneal and (G-I) lung.
G
Figure 5.
PET/MR assists with (A) nodal staging in rectal cancer and, because both PET and MR provide whole-body imaging, the evaluation of distant metastases (B-D) in the liver, (E, F) peritoneal and (G-I) lung.
H
Figure 5.
PET/MR assists with (A) nodal staging in rectal cancer and, because both PET and MR provide whole-body imaging, the evaluation of distant metastases (B-D) in the liver, (E, F) peritoneal and (G-I) lung.
I
Figure 5.
PET/MR assists with (A) nodal staging in rectal cancer and, because both PET and MR provide whole-body imaging, the evaluation of distant metastases (B-D) in the liver, (E, F) peritoneal and (G-I) lung.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
In Practice
PET/MR revolutionizes the assessment of prostate cancer and pelvic malignancies
PET/MR revolutionizes the assessment of prostate cancer and pelvic malignancies
In December 2019, the Misr Radiology Center (MRC) in Cairo, Egypt, became the first institute in Africa to install a PET/MR scanner. As a pioneer in providing both PET and MR imaging, the facility added the SIGNA™ PET/MR system to give its referring urologists and oncologists the most advanced technology for cancer patients.
State-of-the-art applications in prostate cancer
PET/MR has shown growing value in Gallium 68 (68Ga) prostate-specific membrane antigen (PSMA) imaging in recent years for diagnosing/staging, monitoring (e.g., active surveillance) and assessing treatment in prostate cancer patients, one the most common cancers in men. PET/MR can help determine the TNM (tumor, node, metastasis) stage and/or PI-RADS® classification by evaluating the mass, local pelvic and distant lymph nodes, and associated bone marrow metastasis. This is particularly useful in patients with moderate or high risk of metastasis or high grades of prostate cancer.
“In our experience, the SIGNA™ PET/MR system is very helpful for many patients in initial staging for prostate cancer, which are usually the intermediate or high-risk patients with high PSA levels over 20 ng/ml. The PET/MR really helps us with proper evaluation of local staging, especially if extracapsular extensions or seminal vesicle involvement is suspected,” says Rasha Salaheldein, MD, Assistant Professor of Radiology at Ain Shams University and a radiologist at MRC.
Dr. Salaheldein notes that occasionally the seminal vesicles would show a signal alteration in the conventional MR image, which makes it difficult to discriminate between retained secretions and true infiltration in the seminal vesicles. “PET/MR can help to confirm or exclude the involvement of the seminal vesicles, which is crucial in planning the patient’s treatment strategy,” she says.
After treatment, if the patient experiences a biochemical recurrence, the PET/MR is MRC’s modality of choice to assess disease progression. This helps clinicians assess if it is a local occurrence or if there is metastatic spread to distant lymph nodes and organs.
Dr. Salaheldein believes PET/MR is valuable in prostate cancer imaging, due to the combination of 68Ga-PSMA PET with multiparametric MRI (mpMRI), which includes T1 K-trans for permeability, diffusion-weighted and T2-weighted imaging. It is also a critical tool in precisely assessing and characterizing any bone marrow metastases versus other bone marrow lesions.
In four MRC patients previously treated for prostate cancer, 68Ga-PSMA PET/CT found no recurrence of cancer, despite the patients’ rising PSA levels. But when the men were referred for an exam on the SIGNA™ PET/MR system, Dr. Salaheldein found recurrence in the bladder neck and brain that had been masked in the PET/CT images. Pathology confirmed the brain metastases were from the prostate, which is very rare/uncommon.
The PET/MR images also helped evaluate the extra prostatic extension and involvement of the neurovascular bundle to determine if the patient could undergo nerve-sparing surgery.
Figure 1.
A 57-year-old male with recently diagnosed prostatic adenocarcinoma was referred for evaluation of suspicious lymph nodes detected in an MR exam. (A, E) T2w with (B, F) corresponding PET and (C, G) fused PET/MR; (D) ADC; (H) perfusion; and (I) T2w (J) fused with PET. Exam confirmed lymph node involvement. MR exam confirmed the lymph nodes were not metastatic.
Yasser Abd El-Azim Abbas, MD, PhD, Professor of Radiology at Ain Sham University and co-founder of the MRC, calls rising PSA levels in patients with a history of prostate cancer a “red light” that requires investigation. “PSMA PET/MR is excellent at highlighting these tumors and metastases,” he says.
He notes that 68Ga-PSMA PET exams in Egypt are expensive, which can deter doctors from performing them and patients from getting them. The option to use PET/MR in patients with high grades of malignancy for local staging of the prostate, seminal vesicles, lymph nodes near the prostate, distant lymph nodes outside the pelvis, and potential metastases in the bones is a huge benefit.
“When you combine PET and MR in a one-stop shop, you are saving time, effort and money for the patient. This is crucial because otherwise, the patient will do more than one exam that is not read by the same people and there will be ambiguity,” says Dr. Abbas.
PET/MR can also clearly indicate the absence of disease in certain patients. “The SIGNA™ PET/MR can help us see if the patient is non-metastatic, which is very helpful to downstage the patient and is necessary to evaluate these patients,” says Dr. Salaheldein.
In one patient case, conventional CT, which is routinely performed at MRC for staging, showed distant metastatic abdominal and mediastinal lymph nodes. However, the 68Ga-PSMA PET was negative and with the PET/MR exam, Dr. Salaheldein was able to determine that the patient had sarcoidosis, not metastatic prostate cancer, that caused the lymphadenopathies depicted on the CT.
The MRC performs dedicated mpMRI for the prostate, including using FOCUS for diffusion with high b-values for proper evaluation of the primary tumor and evaluation of local staging of the prostate. The center routinely uses PET/MR for whole-body imaging, including the head, neck, chest, abdomen, pelvis and thigh (above the knees), as it helps identify and stage distance metastatic lesions. They also use diffusion-weighted imaging and a T1 perfusion k-trans. “The SIGNA™ PET/MR is excellent in doing this. It has been proven very helpful, especially in the post-treatment cases,” says Dr. Abbas.
Figure 2.
A 76-year-old male previously treated with high intensity focused ultrasound for prostatic cancer and presenting with recently elevated PSA levels was referred to PET/MR to evaluate treatment response. The MR exam demonstrated good treatment of the local prostatic tumor, however, pelvic node metastases were detected, indicating site of biochemical recurrence. (A) T2w, (B) DWI, (C) ADC, (D) post-contrast ADC, (E) perfusion, (F-I) fused PET/MR and (J) whole-body PET .
In the initial MR evaluation protocol, Dr. Salaheldein starts with the mpMRI images, which includes T2, DWI with integrated ADC maps and DCE, to analyze the peripheral and transitional zones of the prostate and determine each zone’s PI-RADS® score. Next, she fuses the PET images to confirm, exclude or modify that initial interpretation. Then, she stages the prostatic capsule and determines seminal vesical involvement. “I evaluate it first with the MR images and then combine it with the PET images later on,” she says.
Next, she moves to nodal evaluation in the pelvis, as well as abdominal, mediastinal and supraclavicular lymph nodes. She also evaluates bone metastases with the whole-body T1-weighted MR images combined with the PET images. Lastly, she evaluates the viscera, including the brain, lungs and liver, and then fuses the T1- and T2-weighted images with the diffusion and PET images on the AW Server.
“Every part of the exam has a particular sequence that is helpful in proper image interpretation. The T1-weighted images help to properly assess any osseous and marrow infiltrative lesions. And in the rest of the abdominal organs, I rely on the T2 images along with the diffusion-weighted imaging,” Dr. Salaheldein says.
GE HealthCare has a comprehensive PI-RADS® acquisition and reporting tool that is supported by PET images. PROView, available on the AW Workstation, provides a deep-learning-based, automated contouring and measurement of the prostate gland for volume calculation and extraction and automated calculation of PSA Density. PROView includes dedicated tools for lesion localization and for reporting on a PI-RADS® sector map. Specifically, PROView enables lesion mapping to sectors and measurement for peripheral and transitional zones and the scoring of T2-weighted, DWI with integrated ADC maps and DCE acquisitions.
Figure 3.
A 70-year-old male with history of radical prostatectomy presenting with high PSA reaching 1.99 ng/ml referred for PET/MR with suspected biochemical recurrence. (A) T2w, (B) ADC, (C) perfusion, (D-F) fused PET (G) FLAIR and (H, I) whole-body PET. Biochemical recurrence at the bladder neck was depicted by mpMRI and was concordant with PSMA-PET. (F, G) Distant brain metastasis was noted.
The value of FDG-PET/MR in pelvic malignancies
There is a growing role for FDG-PET/MR for the proper staging of pelvic cancers, particularly the most common ones that include rectal cancer and gynecological malignancies, such as ovarian and uterine cancers.
MRC utilizes FDG-PET/MR to fully assess tumors in the pelvis, as well as the regional and distant lymph nodes and any metastatic deposits in bones or soft tissue. This is performed in a “one-stop shop” PET/MR exam that delivers structural, functional and metabolic data simultaneously. This hybrid method assesses the structural MR data and metabolic PET data, then adds it to the various novel MR techniques, including diffusion, perfusion, and more.
E
F
G
H
I
Figure 4.
PET/MR provides structural, functional and metabolic data simultaneously in pelvic malignancy cases. (A-C) T2w, (D-F) fused with PET, (G, H) DWI and (I) sagittal T2w. MR facilitates accurate staging because it can depict infiltration of the muscularis propria, mesorectal facial involvement and (I) peritoneal reflection involvement.
In rectal cancer cases, patients come for initial staging, evaluation of chemotherapy and radiotherapy treatment prior to surgery, and evaluation of recurrence after completion of the treatment and surgical intervention.
“PET/MR gives us the edge over PET/CT because of the power of MR in evaluating local tumor staging, which is very crucial in a treatment plan, especially in the mesorectal fascia and circumferential resection margin, which is of concern for both the surgeon and the radiation oncologist,” says Dr. Salaheldein. She adds that MR facilitates accurate staging because it can depict infiltration of the muscularis propria, mesorectal facial involvement and the distance for anorectal junction involvement of anal sphincters, for example, due to its excellent soft tissue imaging capabilities.
Evaluating pelvic lymph nodes can be challenging with conventional imaging, but the SIGNA™ PET/MR helps properly stage the visualized lymph nodes to determine if they are metastatic. “In rectal cancer, it’s important to evaluate metastasis to the liver, because that can change a patient’s treatment plan,” she says. Although National Comprehensive Cancer Network® (NCCN) guidelines recommend performing a CT to evaluate metastases such as these, Dr. Salaheldein says, “we know that MR is more powerful than CT in detecting hepatic metastasis, especially if they are very early or small.”
PET/MR is also critical in evaluating peritoneal involvement in the rectal tumor, which can be challenging to image with only PET due to the high mucous content of the rectal tumor. “Here comes the power of MR and DWI to confirm the presence of peritoneal involvement,” she explains.
Dr. Salaheldein also uses ZTE to evaluate the lungs, a primary site of metastases from rectal cancer. “It’s nice to evaluate the lung without exposing the patient to additional radiation or the need for additional CT imaging to evaluate the lung parenchyma for small pulmonary metastatic lesions – some that may be as small as 6 mm,” she says.
Dr. Abbas notes that PET/MR can have great impact on patient outcomes. “It saves a lot of time for the patient because by the time they do all the other exams, and doctors realize that PET/MR would have been better, their condition might be aggravated,” he says.
Since the installation of the SIGNA™ PET/MR, the facility has seen an increase in demand for scans on it. “Our imaging volume increased a lot because referring clinicians became aware of this marvelous technology that we now have available to patients in Egypt and northern Africa,” says Dr. Salaheldein.
Both doctors expect PET/MR usage to increase with growing global demand, as American and European imaging societies continue to add PET/MR to their guidelines for proper evaluation and staging in certain types of tumors, including brain, neck, prostate and anal tumors.
DOWNLOAD ARTICLE HERE