A
Figure 1.
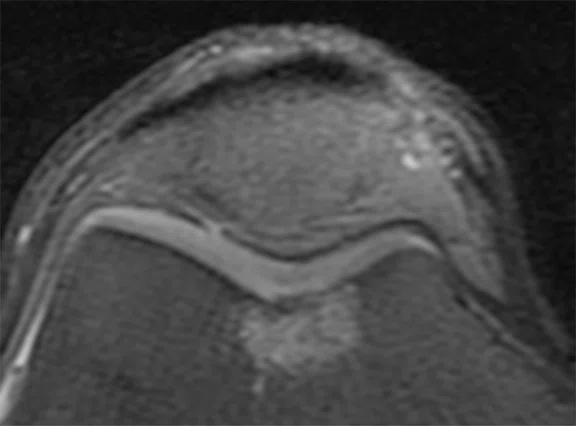
A professional baseball position player was unable to play for seven months due to anterior knee pain. Initial interpretation was chronic, grade 1-2 trochlear chondrosis, based on standard 3.0T exam, (A) axial PD FatSat and (B) sagittal PD FatSat.
B
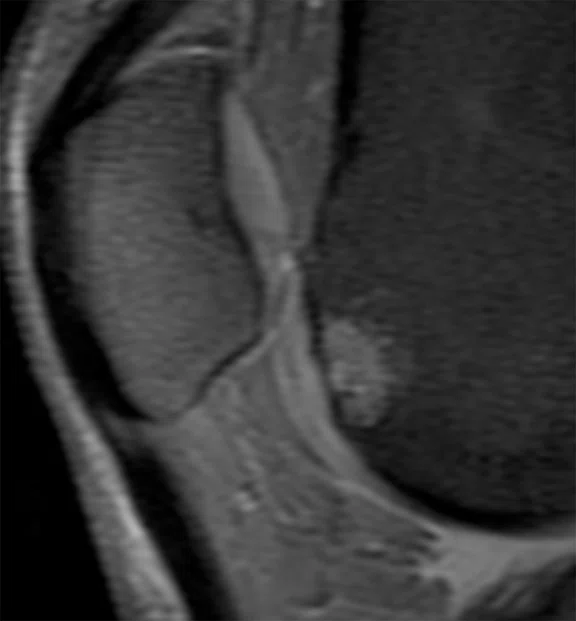
Figure 1.
A professional baseball position player was unable to play for seven months due to anterior knee pain. Initial interpretation was chronic, grade 1-2 trochlear chondrosis, based on standard 3.0T exam, (A) axial PD FatSat and (B) sagittal PD FatSat.
A
Figure 2.
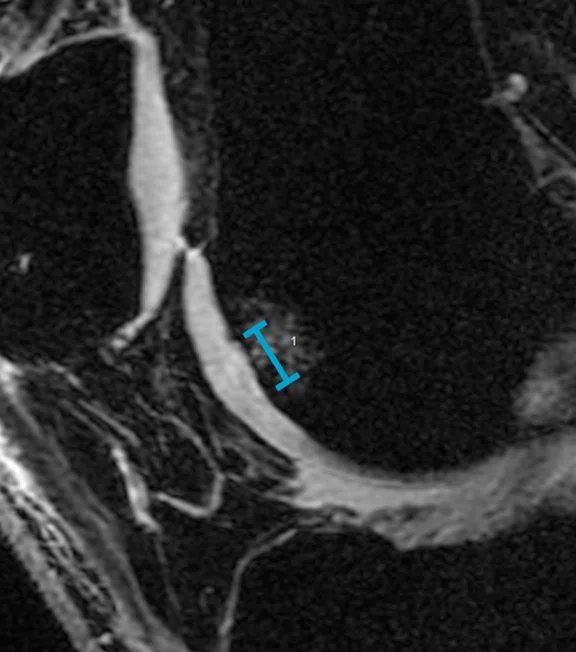
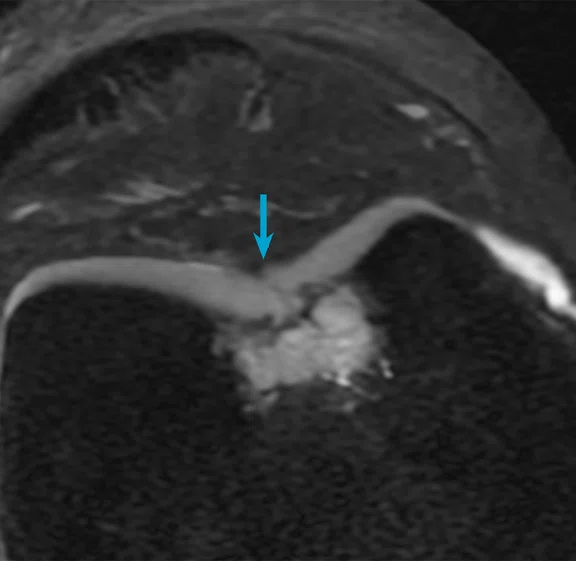
Same patient as Figure 1, underwent follow-up MR. (A) Sagittal and (B) axial 3D FIESTA with AIR™ Recon DL was used for high-resolution, 0.6 mm thin section images demonstrating a grade 3-4 chondrosis with fissure and prominent, active subchondral edema/cysts (likely pain generator). Patient was referred for intervention.
B
Figure 2.
Same patient as Figure 1, underwent follow-up MR. (A) Sagittal and (B) axial 3D FIESTA with AIR™ Recon DL was used for high-resolution, 0.6 mm thin section images demonstrating a grade 3-4 chondrosis with fissure and prominent, active subchondral edema/cysts (likely pain generator). Patient was referred for intervention.
A
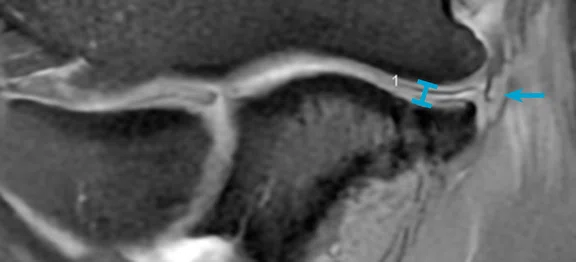
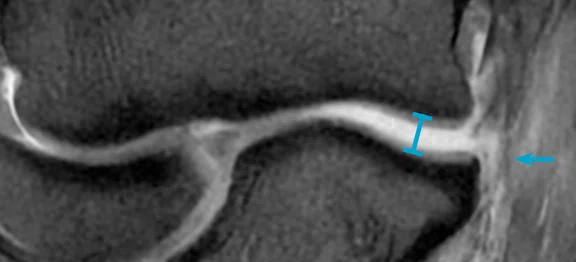
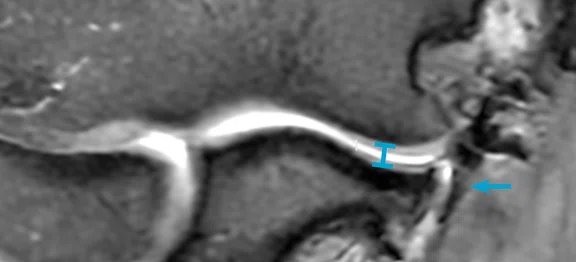
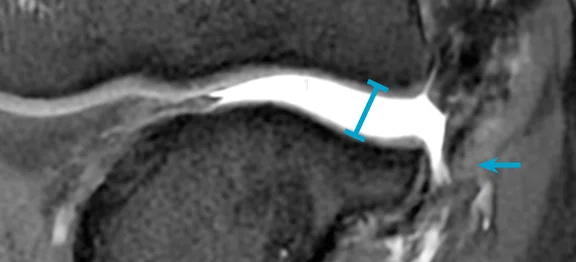
Figure 3.
(A, B) Professional pitcher with initial throwing injury and high-grade distal UCL tear underwent UCL reconstruction and (C, D) sustained re-injury one year later. Elbow thrower’s protocol was performed on SIGNA™ Premier 3.0T with AIR™ Recon DL. (A) Standard coronal 2 mm PD FatSat, TR=2200 ms, TE=40 ms, shows fluid obliteration in majority distal anterior bundle UCL (arrow) and retraction distal fibers. Standard ulnohumeral joint space=2.2 mm (line). (B) FEVER position, PD FatSat, TR=3800 ms, TE=40 ms, showing a high-grade tear with distal UCL fiber obliteration (arrow). FEVER UCL stress view ulnohumeral joint space=3.9 mm (line). (C) Standard coronal 2 mm IW FatSat, TR=3500 ms, TE=40 ms, shows fluid undercutting and traversing distal graft (arrow). Standard coronal ulnohumeral joint space=2.2 mm (line). (D) FEVER position, PD FatSat, TR=4400 ms, TE=50 ms, shows a high-grade tear with distal UCL graft obliteration (arrow). FEVER UCL stress view ulnohumeral joint space=5.2 mm (line).
B
Figure 3.
(A, B) Professional pitcher with initial throwing injury and high-grade distal UCL tear underwent UCL reconstruction and (C, D) sustained re-injury one year later. Elbow thrower’s protocol was performed on SIGNA™ Premier 3.0T with AIR™ Recon DL. (A) Standard coronal 2 mm PD FatSat, TR=2200 ms, TE=40 ms, shows fluid obliteration in majority distal anterior bundle UCL (arrow) and retraction distal fibers. Standard ulnohumeral joint space=2.2 mm (line). (B) FEVER position, PD FatSat, TR=3800 ms, TE=40 ms, showing a high-grade tear with distal UCL fiber obliteration (arrow). FEVER UCL stress view ulnohumeral joint space=3.9 mm (line). (C) Standard coronal 2 mm IW FatSat, TR=3500 ms, TE=40 ms, shows fluid undercutting and traversing distal graft (arrow). Standard coronal ulnohumeral joint space=2.2 mm (line). (D) FEVER position, PD FatSat, TR=4400 ms, TE=50 ms, shows a high-grade tear with distal UCL graft obliteration (arrow). FEVER UCL stress view ulnohumeral joint space=5.2 mm (line).
C
Figure 3.
(A, B) Professional pitcher with initial throwing injury and high-grade distal UCL tear underwent UCL reconstruction and (C, D) sustained re-injury one year later. Elbow thrower’s protocol was performed on SIGNA™ Premier 3.0T with AIR™ Recon DL. (A) Standard coronal 2 mm PD FatSat, TR=2200 ms, TE=40 ms, shows fluid obliteration in majority distal anterior bundle UCL (arrow) and retraction distal fibers. Standard ulnohumeral joint space=2.2 mm (line). (B) FEVER position, PD FatSat, TR=3800 ms, TE=40 ms, showing a high-grade tear with distal UCL fiber obliteration (arrow). FEVER UCL stress view ulnohumeral joint space=3.9 mm (line). (C) Standard coronal 2 mm IW FatSat, TR=3500 ms, TE=40 ms, shows fluid undercutting and traversing distal graft (arrow). Standard coronal ulnohumeral joint space=2.2 mm (line). (D) FEVER position, PD FatSat, TR=4400 ms, TE=50 ms, shows a high-grade tear with distal UCL graft obliteration (arrow). FEVER UCL stress view ulnohumeral joint space=5.2 mm (line).
D
Figure 3.
(A, B) Professional pitcher with initial throwing injury and high-grade distal UCL tear underwent UCL reconstruction and (C, D) sustained re-injury one year later. Elbow thrower’s protocol was performed on SIGNA™ Premier 3.0T with AIR™ Recon DL. (A) Standard coronal 2 mm PD FatSat, TR=2200 ms, TE=40 ms, shows fluid obliteration in majority distal anterior bundle UCL (arrow) and retraction distal fibers. Standard ulnohumeral joint space=2.2 mm (line). (B) FEVER position, PD FatSat, TR=3800 ms, TE=40 ms, showing a high-grade tear with distal UCL fiber obliteration (arrow). FEVER UCL stress view ulnohumeral joint space=3.9 mm (line). (C) Standard coronal 2 mm IW FatSat, TR=3500 ms, TE=40 ms, shows fluid undercutting and traversing distal graft (arrow). Standard coronal ulnohumeral joint space=2.2 mm (line). (D) FEVER position, PD FatSat, TR=4400 ms, TE=50 ms, shows a high-grade tear with distal UCL graft obliteration (arrow). FEVER UCL stress view ulnohumeral joint space=5.2 mm (line).
1. Patel M, Schenk M, Rangan P, Crenshaw K, Caplinger R, Raasch W, Waslewski G, Lederman E, Lund P. Correlation of Joint Space Widening on Valgus Stress Magnetic Resonance Imaging With Level of Play and Innings Pitched in Professional Pitchers. Orthop J Sports Med. 2023 Nov 27;11(11):23259671231209704.
2. Lund P, Waslewski GL, Crenshaw K, Schenk M, Munday G, Knoblauch T, Rodriguez A, Snyder T. FEVER: The Flexed Elbow Valgus External Rotation View for MRI Evaluation of the Ulnar Collateral Ligament in Throwing Athletes-A Pilot Study in Major League Baseball Pitchers. AJR Am J Roentgenol. 2021 Nov;217(5):1176-1183.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
In Practice
SimonMed taps advanced GE HealthCare MR technology to support high-resolution MSK imaging in its outpatient centers
SimonMed taps advanced GE HealthCare MR technology to support high-resolution MSK imaging in its outpatient centers
SimonMed Imaging is one of the largest outpatient medical imaging providers and largest physician radiology practices in the United States. Their motto “See Tomorrow Today” recognizes that new technology can help provide a more accurate diagnosis and should be readily available and affordable.
“Easy accessibility to high-quality imaging equipment that’s affordable in an outpatient setting is important for patients and providers, so we strive to make sure that we not only have advanced technology, but that we’re also affordable,” says John Simon, MD, founder and CEO of SimonMed.
SimonMed has over 25 subspecialty-trained musculoskeletal (MSK) radiologists across the country. It’s that sub specialization combined with the implementation of advanced imaging equipment and standardized protocols that helps ensure quality and consistency in MSK imaging. “Across the country, we can deliver the same kind of sub specialization,” says Dr. Simon.
The unique benefits of working with GE HealthCare
SimonMed has more than 60 GE HealthCare systems across nearly 200 offices. “With SIGNA™, GE HealthCare has a very adaptable platform that enables us to rapidly add new sequences, which is unique compared to other manufacturers. We’ve had tremendous success with GE HealthCare and adapting to the latest MSK sequences and requirements,” says Dr. Simon.
The SIGNA™ Continuum program allows the network to upgrade their machines with the ability to combine hardware, electronics and Imaging Applications for SIGNA™ – without replacing their magnets. “The unique Continuum program allows us to upgrade a system with a high-quality magnet, even taking a conventional (60 cm) bore to a wide bore MR with the latest software and hardware. It’s innovative technology providing both speed and improved quality,” adds Dr. Simon.
SimonMed recently began using AIR™ Recon DL to increase speed and resolution and AIR™ Coils to easily position patients and get high-quality images very quickly. “The coils have made MSK imaging much better. We live and die by our surface coils, and it’s exciting for us to use these coils every day. Together, these technologies help bring in all of the signal we need. It’s hard to get a bad scan on SIGNA™ systems,” says Pamela Lund, MD, Director of MSK Imaging at SimonMed.
The organization is also involved in research and evaluating MR imaging technologies for other novel uses, including the use of GE HealthCare’s zero-TE MR bone imaging (oZTEo) application in non-MSK imaging studies such as in lung and neuro imaging. In the lung, Dr. Simon is investigating if the sequence can help visualize lung parenchyma in low-risk patient cohorts. In the spine, oZTEo is being used in neurospine evaluations to examine the underlying bone structure. “It’s a very interesting sequence that has a lot of potential,” Dr. Simon adds.
Figure 2.
Same patient as Figure 1, underwent follow-up MR. (A) Sagittal and (B) axial 3D FIESTA with AIR™ Recon DL was used for high-resolution, 0.6 mm thin section images demonstrating a grade 3-4 chondrosis with fissure and prominent, active subchondral edema/cysts (likely pain generator). Patient was referred for intervention.
MR imaging of elite and professional athletes
Dr. Lund and the MSK team at SimonMed analyze a variety of MSK MR studies for a large number of elite and professional athletes in Arizona and throughout the country, primarily for injury assessment, treatment and surgical follow-up, as well as pre-participation and team physical screening.
While injury evaluation is often the primary indication for a player to undergo MR imaging, pre-participation scans are very important to help teams identify the potential for injuries and predict player durability. “Football and basketball athletes, often have MR or CT imaging based on prior injuries or surgeries. For baseball athletes we often look at the status of their ulnar collateral ligaments, rotator cuffs and labrum. New or unexpected issues found on these imaging studies might become symptomatic or affect sports skill with the increased intensity of in-season participation or when moving from college to a higher level of play professionally,” says Dr. Lund.
For most athlete MR examinations, SimonMed’s MSK radiologists focus on fluid-sensitive sequences with proton density (PD) weighted and intermediate weighted (IW) FatSat sequences.
“We look for the scan that has the most fluid signal and resolution with the least time and image degradation because we want to see high-resolution anatomy,” explains Dr. Lund. She also believes it’s important to “reconstruct” the injury mechanism based on the combination of MR findings and a solid clinical history. “So, my approach is not just seeing what’s there, but anticipating other findings and problems based on potential combinations of injuries that might require more scrutiny or even additional sequences and images. Distinguishing between normal sports-related adaptive changes and potential injuries is the goal for elite athletes undergoing these exams.”
Figure 3.
(A, B) Professional pitcher with initial throwing injury and high-grade distal UCL tear underwent UCL reconstruction and (C, D) sustained re-injury one year later. Elbow thrower’s protocol was performed on SIGNA™ Premier 3.0T with AIR™ Recon DL. (A) Standard coronal 2 mm PD FatSat, TR=2200 ms, TE=40 ms, shows fluid obliteration in majority distal anterior bundle UCL (arrow) and retraction distal fibers. Standard ulnohumeral joint space=2.2 mm (line). (B) FEVER position, PD FatSat, TR=3800 ms, TE=40 ms, showing a high-grade tear with distal UCL fiber obliteration (arrow). FEVER UCL stress view ulnohumeral joint space=3.9 mm (line). (C) Standard coronal 2 mm IW FatSat, TR=3500 ms, TE=40 ms, shows fluid undercutting and traversing distal graft (arrow). Standard coronal ulnohumeral joint space=2.2 mm (line). (D) FEVER position, PD FatSat, TR=4400 ms, TE=50 ms, shows a high-grade tear with distal UCL graft obliteration (arrow). FEVER UCL stress view ulnohumeral joint space=5.2 mm (line).
Fast, thin section imaging
In her MSK practice at SimonMed, Dr. Lund is using AIR™ Recon DL in conjunction with FIESTA 3D gradient echoes to achieve very thin sections of 0.6 mm, which is useful for T2 mapping of cartilage. “The resolution is amazing, particularly for cartilage scans. With AIR™ Recon DL, our scan times have been reduced from 40 to 60 minutes to 25 minutes, which gives us a full knee and cartilage sequence,” says Dr. Lund. Previously, with the long scan times needed to process the images for T2 mapping, the data wasn’t always acquired and therefore not used by orthopedic surgeons. Now, however, with the faster scanning and high-quality imaging, she anticipates these cartilage studies could potentially be used by orthopedists for pre-surgical planning.
As MR scanning continues to increase in speed, Dr. Lund sees the opportunity to perform a dynamic evaluation of the joint. With wide bore systems, it is possible to capture elbow, knee, foot or wrist joints in different positions. For example, Dr. Lund was a co-author in several papers examining the elbow in the active throwing position in professional baseball pitchers. The flexed elbow valgus external rotation (FEVER) view was found to increase diagnostic confidence when evaluating ulnar collateral ligament (UCL) injuries, as well as helped predict future pitching performance.1,2
“Although investing in AI-enhanced, high-speed and high-resolution MR technologies can be intimidating, a well-structured plan to build technical and professional quality will always drive volume and excellence in patient care,” Dr. Lund adds.
Dr. Lund also envisions using stress views in knee imaging, particularly using an ACL-PCL stress view. “It’s the perfect storm
of wide bore, fast scanning and high-resolution imaging that is going to be very exciting as we move forward in MSK MR imaging,” she says.
To other practices seeking to implement high-resolution MSK imaging in their practices, Dr. Simon advises sub specialization, specifically including MSK-trained radiologists and adding equipment that’s adaptable and high-quality to deliver superb images, saying, “That’s been a strength of GE HealthCare and why we’re a strong supporter of GE HealthCare and their equipment, because they give us innovative technologies that enable us to get high-quality images for better diagnoses.”
DOWNLOAD ARTICLE HERE