A
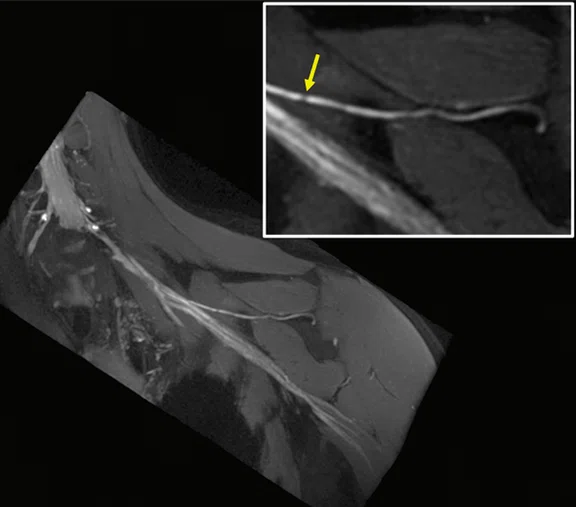
Figure 1.
A 43-year-old male with Parsonage-Turner syndrome and right shoulder weakness. Oblique coronal curved maximum intensity projections were generated from a 1 mm isotropic Cube STIR acquisition (4:30 min., TR/TE=3000/60 ms). (A) Standard and (B) AIR™ Recon DL reconstructions provide excellent depiction of the brachial plexus and hourglass-like constriction of the suprascapular (yellow arrow) nerve. AIR™ Recon DL provides additional denoising and sharpness (inset, 1B) for greater diagnostic confidence.
B
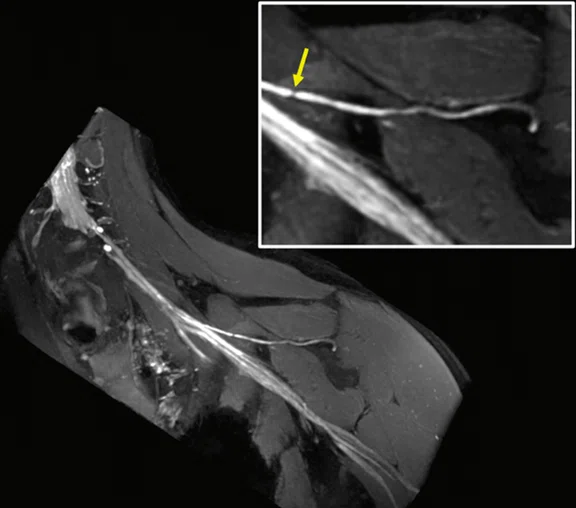
Figure 1.
A 43-year-old male with Parsonage-Turner syndrome and right shoulder weakness. Oblique coronal curved maximum intensity projections were generated from a 1 mm isotropic Cube STIR acquisition (4:30 min., TR/TE=3000/60 ms). (A) Standard and (B) AIR™ Recon DL reconstructions provide excellent depiction of the brachial plexus and hourglass-like constriction of the suprascapular (yellow arrow) nerve. AIR™ Recon DL provides additional denoising and sharpness (inset, 1B) for greater diagnostic confidence.
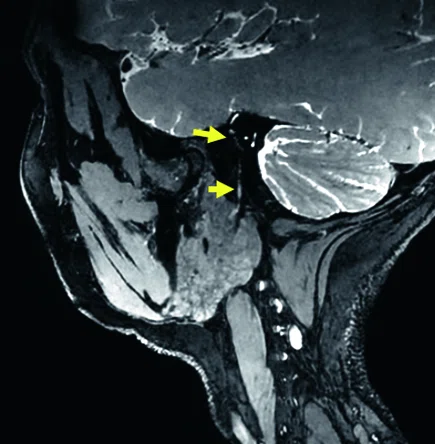
A
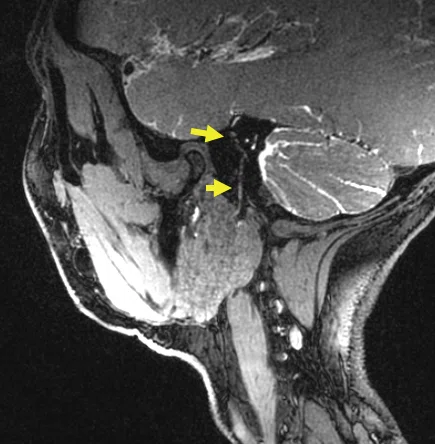
Figure 2.
A 36-year-old female with left-sided Bell’s palsy (facial nerve paralysis). (A) As compared to the 1st echo from a 3D MENSA NERVE unilateral sagittal acquisition (0.7 mm isotropic, 5:29 min., TR/TE=14.4/5.1-9.3 ms) of the left facial region, the (B, D) MENSA NERVE 2nd echo has greater T2-weighting and vascular suppression, but much lower signal. (C, E) AIR™ Recon DL improves the image quality of the 2nd echo MENSA NERVE, providing improved conspicuity and visualization of the facial nerve extending through the parotid gland and more superficially into the face, as shown in the 7 mm maximum intensity projections in (E) the oblique sagittal and oblique axial planes.
B
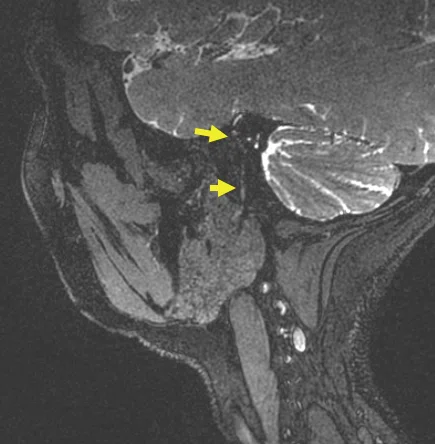
Figure 2.
A 36-year-old female with left-sided Bell’s palsy (facial nerve paralysis). (A) As compared to the 1st echo from a 3D MENSA NERVE unilateral sagittal acquisition (0.7 mm isotropic, 5:29 min., TR/TE=14.4/5.1-9.3 ms) of the left facial region, the (B, D) MENSA NERVE 2nd echo has greater T2-weighting and vascular suppression, but much lower signal. (C, E) AIR™ Recon DL improves the image quality of the 2nd echo MENSA NERVE, providing improved conspicuity and visualization of the facial nerve extending through the parotid gland and more superficially into the face, as shown in the 7 mm maximum intensity projections in (E) the oblique sagittal and oblique axial planes.
C
Figure 2.
A 36-year-old female with left-sided Bell’s palsy (facial nerve paralysis). (A) As compared to the 1st echo from a 3D MENSA NERVE unilateral sagittal acquisition (0.7 mm isotropic, 5:29 min., TR/TE=14.4/5.1-9.3 ms) of the left facial region, the (B, D) MENSA NERVE 2nd echo has greater T2-weighting and vascular suppression, but much lower signal. (C, E) AIR™ Recon DL improves the image quality of the 2nd echo MENSA NERVE, providing improved conspicuity and visualization of the facial nerve extending through the parotid gland and more superficially into the face, as shown in the 7 mm maximum intensity projections in (E) the oblique sagittal and oblique axial planes.
D
Figure 2.
A 36-year-old female with left-sided Bell’s palsy (facial nerve paralysis). (A) As compared to the 1st echo from a 3D MENSA NERVE unilateral sagittal acquisition (0.7 mm isotropic, 5:29 min., TR/TE=14.4/5.1-9.3 ms) of the left facial region, the (B, D) MENSA NERVE 2nd echo has greater T2-weighting and vascular suppression, but much lower signal. (C, E) AIR™ Recon DL improves the image quality of the 2nd echo MENSA NERVE, providing improved conspicuity and visualization of the facial nerve extending through the parotid gland and more superficially into the face, as shown in the 7 mm maximum intensity projections in (E) the oblique sagittal and oblique axial planes.
E
Figure 2.
A 36-year-old female with left-sided Bell’s palsy (facial nerve paralysis). (A) As compared to the 1st echo from a 3D MENSA NERVE unilateral sagittal acquisition (0.7 mm isotropic, 5:29 min., TR/TE=14.4/5.1-9.3 ms) of the left facial region, the (B, D) MENSA NERVE 2nd echo has greater T2-weighting and vascular suppression, but much lower signal. (C, E) AIR™ Recon DL improves the image quality of the 2nd echo MENSA NERVE, providing improved conspicuity and visualization of the facial nerve extending through the parotid gland and more superficially into the face, as shown in the 7 mm maximum intensity projections in (E) the oblique sagittal and oblique axial planes.
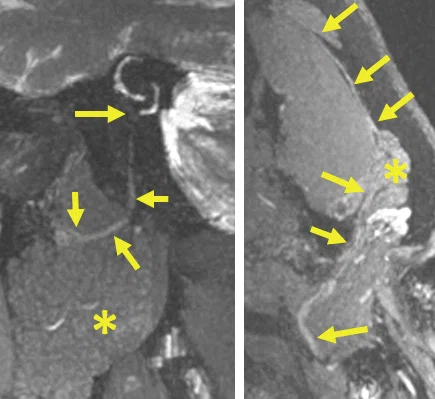
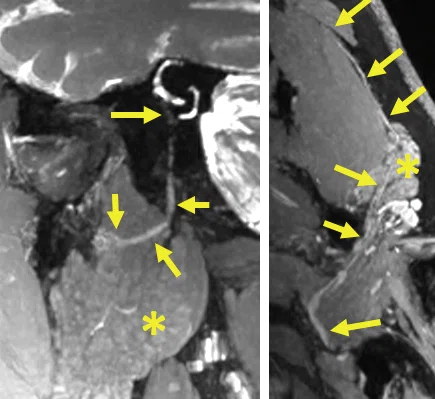
A
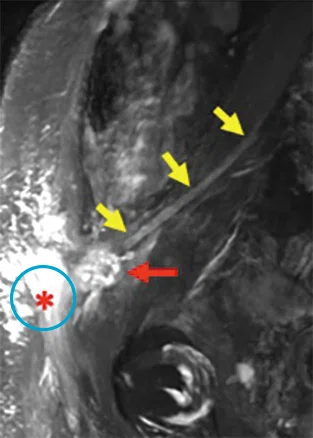
Figure 3.
A 78-year-old woman with endometrial cancer presents with a cystic mass (presumed metastasis) (red arrow) impinging the right femoral nerve (yellow arrows) and resulting in denervation of the iliacus muscle (red asterisk). These structures are well visualized with AIR™ Recon DL reconstructions of both (A, B) Cube-STIR (1.2 mm isotropic, 6:25 min.) and (C, D) MENSA NERVE (0.9 mm isotropic, 5:52 min.), but MENSA NERVE demonstrates increased sharpness and conspicuity of the overall lumbosacral plexi on coronal images and of the femoral nerve in the 8 mm oblique-coronal maximum intensity projection.
B
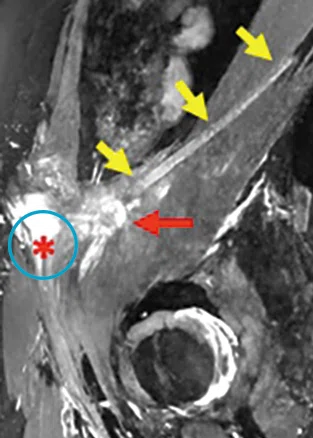
Figure 3.
A 78-year-old woman with endometrial cancer presents with a cystic mass (presumed metastasis) (red arrow) impinging the right femoral nerve (yellow arrows) and resulting in denervation of the iliacus muscle (red asterisk). These structures are well visualized with AIR™ Recon DL reconstructions of both (A, B) Cube-STIR (1.2 mm isotropic, 6:25 min.) and (C, D) MENSA NERVE (0.9 mm isotropic, 5:52 min.), but MENSA NERVE demonstrates increased sharpness and conspicuity of the overall lumbosacral plexi on coronal images and of the femoral nerve in the 8 mm oblique-coronal maximum intensity projection.
C
Figure 3.
A 78-year-old woman with endometrial cancer presents with a cystic mass (presumed metastasis) (red arrow) impinging the right femoral nerve (yellow arrows) and resulting in denervation of the iliacus muscle (red asterisk). These structures are well visualized with AIR™ Recon DL reconstructions of both (A, B) Cube-STIR (1.2 mm isotropic, 6:25 min.) and (C, D) MENSA NERVE (0.9 mm isotropic, 5:52 min.), but MENSA NERVE demonstrates increased sharpness and conspicuity of the overall lumbosacral plexi on coronal images and of the femoral nerve in the 8 mm oblique-coronal maximum intensity projection.
D
Figure 3.
A 78-year-old woman with endometrial cancer presents with a cystic mass (presumed metastasis) (red arrow) impinging the right femoral nerve (yellow arrows) and resulting in denervation of the iliacus muscle (red asterisk). These structures are well visualized with AIR™ Recon DL reconstructions of both (A, B) Cube-STIR (1.2 mm isotropic, 6:25 min.) and (C, D) MENSA NERVE (0.9 mm isotropic, 5:52 min.), but MENSA NERVE demonstrates increased sharpness and conspicuity of the overall lumbosacral plexi on coronal images and of the femoral nerve in the 8 mm oblique-coronal maximum intensity projection.
1. Fisher S, Wadhwa V, Manthuruthil C, Cheng J, Chhabra A. Clinical impact of magnetic resonance neurography in patients with brachial plexus neuropathies. Br J Radiol. 2016 Nov;89(1067):20160503.
2. Upadhyaya V, Upadhyaya DN, Kumar A, Gujral RB. MR neurography in traumatic brachial plexopathy. Eur J Radiol. 2015;84(5):927-932.
3. Chhabra A, Belzberg AJ, Rosson GD, et al. Impact of high resolution 3 tesla MR neurography (MRN) on diagnostic thinking and therapeutic patient management. Eur Radiol. 2016;26(5):1235-1244.
4. Sneag DB, Queler SC, Campbell G, et al. Optimized 3D brachial plexus MR neurography using deep learning reconstruction [published online ahead of print, 2023 Nov 2]. Skeletal Radiol. 2023;10.1007/s00256-023-04484-4.
A
Figure 4.
A 66-year-old man with sensory disturbance within the left median nerve distribution. (A, B) Axial and (C, D) oblique coronal reformatted images of 3D MENSA NERVE (0.4 x 0.4 x 1.6 mm, 1:48 min., 2nd echo shown) acquired through the distal left forearm. As compared to (A, C) standard reconstruction, (B, D) AIR™ Recon DL provides improved sharpness for depiction of a large peripheral nerve sheath tumor (PNST) arising from the median nerve. (E) AIR™ Recon DL enables a clean 3D rendering of the PNST by fusing MENSA NERVE and oZTEo (bone) images using Volume Viewer 15.0.
B
Figure 4.
A 66-year-old man with sensory disturbance within the left median nerve distribution. (A, B) Axial and (C, D) oblique coronal reformatted images of 3D MENSA NERVE (0.4 x 0.4 x 1.6 mm, 1:48 min., 2nd echo shown) acquired through the distal left forearm. As compared to (A, C) standard reconstruction, (B, D) AIR™ Recon DL provides improved sharpness for depiction of a large peripheral nerve sheath tumor (PNST) arising from the median nerve. (E) AIR™ Recon DL enables a clean 3D rendering of the PNST by fusing MENSA NERVE and oZTEo (bone) images using Volume Viewer 15.0.
E
Figure 4.
A 66-year-old man with sensory disturbance within the left median nerve distribution. (A, B) Axial and (C, D) oblique coronal reformatted images of 3D MENSA NERVE (0.4 x 0.4 x 1.6 mm, 1:48 min., 2nd echo shown) acquired through the distal left forearm. As compared to (A, C) standard reconstruction, (B, D) AIR™ Recon DL provides improved sharpness for depiction of a large peripheral nerve sheath tumor (PNST) arising from the median nerve. (E) AIR™ Recon DL enables a clean 3D rendering of the PNST by fusing MENSA NERVE and oZTEo (bone) images using Volume Viewer 15.0.
C
Figure 4.
A 66-year-old man with sensory disturbance within the left median nerve distribution. (A, B) Axial and (C, D) oblique coronal reformatted images of 3D MENSA NERVE (0.4 x 0.4 x 1.6 mm, 1:48 min., 2nd echo shown) acquired through the distal left forearm. As compared to (A, C) standard reconstruction, (B, D) AIR™ Recon DL provides improved sharpness for depiction of a large peripheral nerve sheath tumor (PNST) arising from the median nerve. (E) AIR™ Recon DL enables a clean 3D rendering of the PNST by fusing MENSA NERVE and oZTEo (bone) images using Volume Viewer 15.0.
D
Figure 4.
A 66-year-old man with sensory disturbance within the left median nerve distribution. (A, B) Axial and (C, D) oblique coronal reformatted images of 3D MENSA NERVE (0.4 x 0.4 x 1.6 mm, 1:48 min., 2nd echo shown) acquired through the distal left forearm. As compared to (A, C) standard reconstruction, (B, D) AIR™ Recon DL provides improved sharpness for depiction of a large peripheral nerve sheath tumor (PNST) arising from the median nerve. (E) AIR™ Recon DL enables a clean 3D rendering of the PNST by fusing MENSA NERVE and oZTEo (bone) images using Volume Viewer 15.0.
4. Sneag DB, Queler SC, Campbell G, et al. Optimized 3D brachial plexus MR neurography using deep learning reconstruction [published online ahead of print, 2023 Nov 2]. Skeletal Radiol. 2023;10.1007/s00256-023-04484-4.
4. Sneag DB, Queler SC, Campbell G, et al. Optimized 3D brachial plexus MR neurography using deep learning reconstruction [published online ahead of print, 2023 Nov 2]. Skeletal Radiol. 2023;10.1007/s00256-023-04484-4.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
In Practice
Technical and practical considerations for robust MR neurography
Technical and practical considerations for robust MR neurography
By Ek Tsoon Tan, PhD, Co-Director, MRI Lab and Darryl B. Sneag, MD, Director MR Neurography and MRI Research at the Hospital for Special Surgery, New York, NY
MR neurography serves as an important adjunct to electrodiagnostic testing (EDX).1 It is helpful for localization of nerve injury, especially when multifocal or fascicular (i.e., involvement of only a portion of the cross-sectional diameter of the nerve), under which conditions nerve lesions can be difficult to precisely localize with EDX. MR neurography has been shown to influence surgical planning and outcomes2,3 and in doing so, provides a global assessment of nerves and muscles. MR neurography also provides visual clues about whether the muscles that an injured nerve supplies have lost function.
At the Hospital for Special Surgery (HSS), MR neurography is used to diagnose many traumatic and atraumatic conditions that cause nerve compression, entrapment or disruption throughout the body, including in the upper cervical region, brachial and lumbosacral plexi, and upper/lower extremities. MR neurography poses several technical challenges, particularly the demand for high SNR to accommodate submillimeter acquisitions, given the small size (many less than 1 mm diameter) of peripheral nerves.
At HSS, MR neurography is frequently acquired on one of our SIGNA™ Premier 3.0T systems due to the inherent increase in SNR at 3.0T and the tight echo spacing and wide bore configuration of this particular system that facilitates positioning of the target anatomy closer to isocenter. A wide bore is also more comfortable for patients, particularly those with broad shoulders or torsos. There is also an added benefit to using the AIR™ Coils in these NYtypes of examinations. Technologists can reliably and repeatably position the AIR™ Coils using the markings that indicate where the coil center (“sweet spot”) is located. When covering a large area, the AIR™ Coils provide good superior-inferior coverage with high SNR within each segment of the coil. These coils are flexible for positioning around anatomy that may otherwise be difficult to cover, such as extremities that cannot be fully extended, for instance, due to an injury or post-surgery. The coils’ flexibility enables close positioning to the targeted anatomy to boost SNR. The AIR™ Coils also provide the potential for obtaining SNR from otherwise challenging anatomic regions with a concave surface, such as the axilla, neck and inner thigh.
Modifying sequence parameters and applying specialized “nerve-sensitive” sequences in MR neurography differentiate small nerves from other adjacent structures, particularly blood vessels, that may appear similar in size and signal intensity. Sequences are typically heavily T2-weighted to enhance pathologic changes and of sufficient spatial resolution to depict focal nerve enlargement and any alterations in the nerve’s morphology or course.
As with any type of imaging in the chest or abdomen, there is the potential for breathing or bowel motion that can lead to artifacts. Extremity imaging is frequently acquired off-isocenter, thereby requiring robust fat suppression techniques due to inherently poorer field homogeneities off-isocenter.
Figure 1.
A 43-year-old male with Parsonage-Turner syndrome and right shoulder weakness. Oblique coronal curved maximum intensity projections were generated from a 1 mm isotropic Cube STIR acquisition (4:30 min., TR/TE=3000/60 ms). (A) Standard and (B) AIR™ Recon DL reconstructions provide excellent depiction of the brachial plexus and hourglass-like constriction of the suprascapular (yellow arrow) nerve. AIR™ Recon DL provides additional denoising and sharpness (inset, 1B) for greater diagnostic confidence.
Figure 2.
A 36-year-old female with left-sided Bell’s palsy (facial nerve paralysis). (A) As compared to the 1st echo from a 3D MENSA NERVE unilateral sagittal acquisition (0.7 mm isotropic, 5:29 min., TR/TE=14.4/5.1-9.3 ms) of the left facial region, the (B, D) MENSA NERVE 2nd echo has greater T2-weighting and vascular suppression, but much lower signal. (C, E) AIR™ Recon DL improves the image quality of the 2nd echo MENSA NERVE, providing improved conspicuity and visualization of the facial nerve extending through the parotid gland and more superficially into the face, as shown in the 7 mm maximum intensity projections in (E) the oblique sagittal and oblique axial planes.
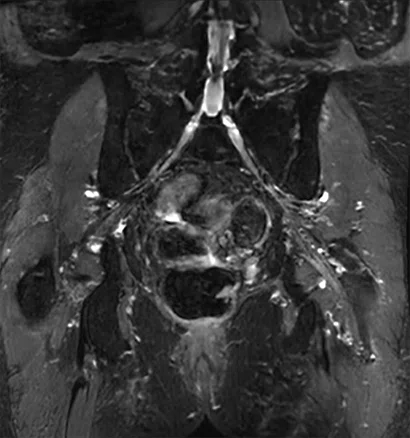
Figure 3.
A 78-year-old woman with endometrial cancer presents with a cystic mass (presumed metastasis) (red arrow) impinging the right femoral nerve (yellow arrows) and resulting in denervation of the iliacus muscle (red asterisk). These structures are well visualized with AIR™ Recon DL reconstructions of both (A, B) Cube-STIR (1.2 mm isotropic, 6:25 min.) and (C, D) MENSA NERVE (0.9 mm isotropic, 5:52 min.), but MENSA NERVE demonstrates increased sharpness and conspicuity of the overall lumbosacral plexi on coronal images and of the femoral nerve in the 8 mm oblique-coronal maximum intensity projection.
Figure 4.
A 66-year-old man with sensory disturbance within the left median nerve distribution. (A, B) Axial and (C, D) oblique coronal reformatted images of 3D MENSA NERVE (0.4 x 0.4 x 1.6 mm, 1:48 min., 2nd echo shown) acquired through the distal left forearm. As compared to (A, C) standard reconstruction, (B, D) AIR™ Recon DL provides improved sharpness for depiction of a large peripheral nerve sheath tumor (PNST) arising from the median nerve. (E) AIR™ Recon DL enables a clean 3D rendering of the PNST by fusing MENSA NERVE and oZTEo (bone) images using Volume Viewer 15.0.
As an orthopedic hospital, we are often asked to evaluate peripheral nerves in the presence of MR-Conditional implants, such as a total joint replacement or fracture fixation hardware. In these cases, where susceptibility artifacts can obscure visualization of the nerve, the use of metal artifact reduction techniques such as MAVRIC SL are instrumental.
In our experience, employing metal artifact reduction sequences (MARS) such as MAVRIC SL is helpful to reduce artifacts resulting from the presence of metal that may obscure direct visualization of the nerves. The decision to utilize MARS should depend upon the radiologist’s experience as to the severity of the artifact produced by the particular hardware type, as well as its proximity to the nerve of interest. In some cases, the MR-Conditional implants may not interfere with the depiction of the nerve, for which imaging may be performed without the use of MARS.
When imaging small nerves, we attempt to acquire images at the highest feasible spatial resolution, which may sometimes result in variable SNR between patients, especially in larger-sized patients or in anatomies such as the brachial plexus where it is difficult to position more conventional, rigid coils close to the nerves. However, with the combination of AIR™ Recon DL and the highly flexible AIR™ Coils, the latter closely conforming to the targeted anatomical region, we can improve sharpness by up to 60% and increase SNR to provide more detailed depiction of the nerves. Hence, the availability of both AIR™ technologies are integral to performing robust MR neurography.
At HSS, we have recently been working with GE HealthCare to optimize a non-contrast technique, 3D MENSA NERVE, that suppresses signal from the vasculature. MENSA NERVE is a two-echo, steady-state free precession acquisition using a prolonged and unbalanced readout gradient. It obtains the FID signal of FIESTA (T1/T2-weighted) and the echo-signal of a time-reversed FIESTA (more T2-weighted) separately. The echo-signal (2nd echo) provides vascular suppression and T2-weighting, while the FID signal (1st echo) provides high SNR anatomical reference. In addition, water selective excitation pulse is used to achieve fat suppression. When reconstructed separately, users can compare either image to better visualize the nerve anatomy. MENSA NERVE acquisitions are also reconstructed with AIR™ Recon DL to improve SNR and sharpness.4
MENSA NERVE is ideal for imaging the lumbosacral plexus and upper/lower peripheral extremity nerves. It provides superior sharpness for evaluation of smaller nerves, as compared to 3D Cube STIR fast spin echo, and tends to be SNR sufficient, enabling high (0.7-1 mm) through-plane resolution. For example, we can now obtain an 0.8 mm isotropic acquisition of the lumbosacral plexus within a 5 minute scan time, whereas a 1.4 mm isotropic 3D Cube STIR sequence would typically require a 7-8 minute acquisition time.
In summary, hardware (e.g., SIGNA™ Premier 3.0T and AIR™ Coils) and software (e.g., MENSA NERVE and AIR™ Recon DL) components collectively enable robust MR neurography exams to maximize diagnostic yield and efficiency for our patients.
DOWNLOAD ARTICLE HERE