A
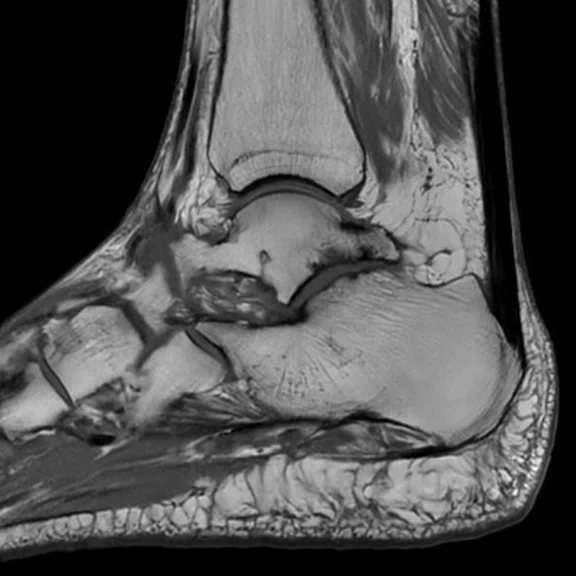
Figure 3.
A 68-year-old patient with pain after ankle sprain. MR depicted a small internal osteochondral lesion in the talar dome and subtalar arthropathy. Images acquired with AIR™ MP Coil and (A-E) AIR™ Recon DL. (A) Sagittal PD FSE FatSat, 0.4 x 0.5 x 2.0 MM, 2:56 min.; (B) sagittal T1 FSE, 0.4 x 0.4 x 2.0 mm, 1:59 min.; (C) axial PD FSE FatSat, 0.3 x 0.3 x 3.0 mm, 2:48 min.; (D) coronal PD FSE FatSat, 0.4 x 0.5 x 2.0 mm, 2:37 min.; (E) coronal T1 FSE, 0.4 x 0.5 x 2.0 mm, 2:20 min.; and (F) coronal reformat of a sagittal oZTEo acquisition.
B
Figure 3.
A 68-year-old patient with pain after ankle sprain. MR depicted a small internal osteochondral lesion in the talar dome and subtalar arthropathy. Images acquired with AIR™ MP Coil and (A-E) AIR™ Recon DL. (A) Sagittal PD FSE FatSat, 0.4 x 0.5 x 2.0 MM, 2:56 min.; (B) sagittal T1 FSE, 0.4 x 0.4 x 2.0 mm, 1:59 min.; (C) axial PD FSE FatSat, 0.3 x 0.3 x 3.0 mm, 2:48 min.; (D) coronal PD FSE FatSat, 0.4 x 0.5 x 2.0 mm, 2:37 min.; (E) coronal T1 FSE, 0.4 x 0.5 x 2.0 mm, 2:20 min.; and (F) coronal reformat of a sagittal oZTEo acquisition.
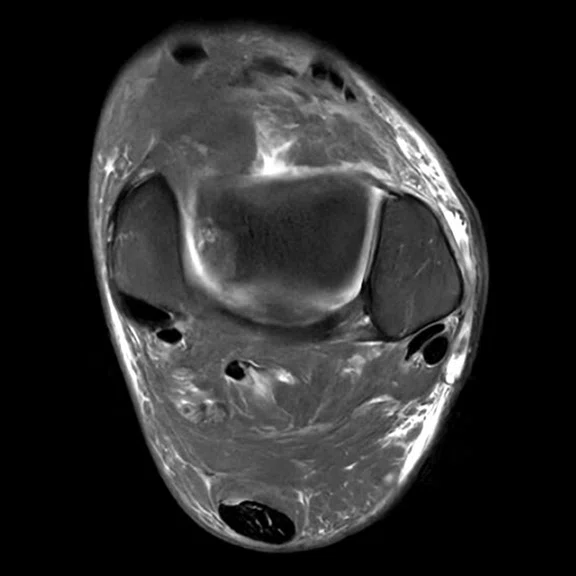
C
Figure 3.
A 68-year-old patient with pain after ankle sprain. MR depicted a small internal osteochondral lesion in the talar dome and subtalar arthropathy. Images acquired with AIR™ MP Coil and (A-E) AIR™ Recon DL. (A) Sagittal PD FSE FatSat, 0.4 x 0.5 x 2.0 MM, 2:56 min.; (B) sagittal T1 FSE, 0.4 x 0.4 x 2.0 mm, 1:59 min.; (C) axial PD FSE FatSat, 0.3 x 0.3 x 3.0 mm, 2:48 min.; (D) coronal PD FSE FatSat, 0.4 x 0.5 x 2.0 mm, 2:37 min.; (E) coronal T1 FSE, 0.4 x 0.5 x 2.0 mm, 2:20 min.; and (F) coronal reformat of a sagittal oZTEo acquisition.
A
Figure 1.
A 73-year-old patient assessed for atypical vertigo was found to have right APC type 2 schwannoma. (A) Axial reformat of a sagittal T2 FLAIR Cube, 1.0 x 1.0 x 1.3 mm, 3:24 min.; (B) coronal reformat of an axial T2 Cube, 0.5 x 0.5 x 0.5 mm, 2:53 min.; (C) axial T1 FSE, 0.5 x 0.7 x 1.5 mm, 2:15 min. with AIR™ Recon DL; and (D) axial T2 Cube, 0.5 x 0.5 x 0.5 mm, 2:53 min.
B
Figure 1.
A 73-year-old patient assessed for atypical vertigo was found to have right APC type 2 schwannoma. (A) Axial reformat of a sagittal T2 FLAIR Cube, 1.0 x 1.0 x 1.3 mm, 3:24 min.; (B) coronal reformat of an axial T2 Cube, 0.5 x 0.5 x 0.5 mm, 2:53 min.; (C) axial T1 FSE, 0.5 x 0.7 x 1.5 mm, 2:15 min. with AIR™ Recon DL; and (D) axial T2 Cube, 0.5 x 0.5 x 0.5 mm, 2:53 min.
C
Figure 1.
A 73-year-old patient assessed for atypical vertigo was found to have right APC type 2 schwannoma. (A) Axial reformat of a sagittal T2 FLAIR Cube, 1.0 x 1.0 x 1.3 mm, 3:24 min.; (B) coronal reformat of an axial T2 Cube, 0.5 x 0.5 x 0.5 mm, 2:53 min.; (C) axial T1 FSE, 0.5 x 0.7 x 1.5 mm, 2:15 min. with AIR™ Recon DL; and (D) axial T2 Cube, 0.5 x 0.5 x 0.5 mm, 2:53 min.
D
Figure 1.
A 73-year-old patient assessed for atypical vertigo was found to have right APC type 2 schwannoma. (A) Axial reformat of a sagittal T2 FLAIR Cube, 1.0 x 1.0 x 1.3 mm, 3:24 min.; (B) coronal reformat of an axial T2 Cube, 0.5 x 0.5 x 0.5 mm, 2:53 min.; (C) axial T1 FSE, 0.5 x 0.7 x 1.5 mm, 2:15 min. with AIR™ Recon DL; and (D) axial T2 Cube, 0.5 x 0.5 x 0.5 mm, 2:53 min.
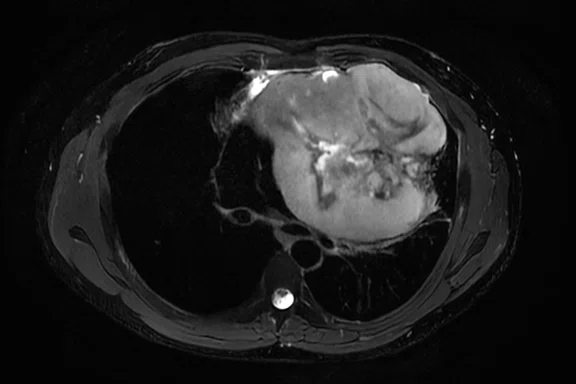
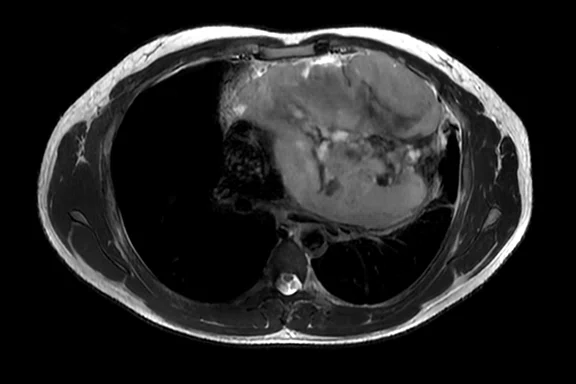
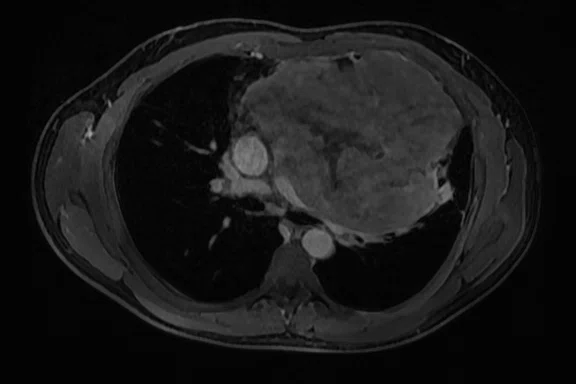
A
Figure 2.
A 30-year-old patient with dyspnea for 6 months. Mediastinal mass found on CT, referred to MR to determine if mass is a thymoma or sarcoma. Images acquired with AIR™ AA Coil and (A-D) AIR™ Recon DL. (A) Axial T2 SSFSE FatSat, 1.2 x 1.8 x 4.0 mm, 37 sec.; (B) axial T2 SSFSE, 1.2 x 1.8 x 4.0 mm, 40 sec.; (C) axial LAVA Flex, 1.4 x 1.7 x 2.2 mm, 17 sec.; (D) coronal T2 SSFSE, 1.0 x 1.6 x 4.0 mm, 47 sec.; and (E) MUSE b800, 4:22 min.
B
Figure 2.
A 30-year-old patient with dyspnea for 6 months. Mediastinal mass found on CT, referred to MR to determine if mass is a thymoma or sarcoma. Images acquired with AIR™ AA Coil and (A-D) AIR™ Recon DL. (A) Axial T2 SSFSE FatSat, 1.2 x 1.8 x 4.0 mm, 37 sec.; (B) axial T2 SSFSE, 1.2 x 1.8 x 4.0 mm, 40 sec.; (C) axial LAVA Flex, 1.4 x 1.7 x 2.2 mm, 17 sec.; (D) coronal T2 SSFSE, 1.0 x 1.6 x 4.0 mm, 47 sec.; and (E) MUSE b800, 4:22 min.
C
Figure 2.
A 30-year-old patient with dyspnea for 6 months. Mediastinal mass found on CT, referred to MR to determine if mass is a thymoma or sarcoma. Images acquired with AIR™ AA Coil and (A-D) AIR™ Recon DL. (A) Axial T2 SSFSE FatSat, 1.2 x 1.8 x 4.0 mm, 37 sec.; (B) axial T2 SSFSE, 1.2 x 1.8 x 4.0 mm, 40 sec.; (C) axial LAVA Flex, 1.4 x 1.7 x 2.2 mm, 17 sec.; (D) coronal T2 SSFSE, 1.0 x 1.6 x 4.0 mm, 47 sec.; and (E) MUSE b800, 4:22 min.
D
Figure 2.
A 30-year-old patient with dyspnea for 6 months. Mediastinal mass found on CT, referred to MR to determine if mass is a thymoma or sarcoma. Images acquired with AIR™ AA Coil and (A-D) AIR™ Recon DL. (A) Axial T2 SSFSE FatSat, 1.2 x 1.8 x 4.0 mm, 37 sec.; (B) axial T2 SSFSE, 1.2 x 1.8 x 4.0 mm, 40 sec.; (C) axial LAVA Flex, 1.4 x 1.7 x 2.2 mm, 17 sec.; (D) coronal T2 SSFSE, 1.0 x 1.6 x 4.0 mm, 47 sec.; and (E) MUSE b800, 4:22 min.
E
Figure 2.
A 30-year-old patient with dyspnea for 6 months. Mediastinal mass found on CT, referred to MR to determine if mass is a thymoma or sarcoma. Images acquired with AIR™ AA Coil and (A-D) AIR™ Recon DL. (A) Axial T2 SSFSE FatSat, 1.2 x 1.8 x 4.0 mm, 37 sec.; (B) axial T2 SSFSE, 1.2 x 1.8 x 4.0 mm, 40 sec.; (C) axial LAVA Flex, 1.4 x 1.7 x 2.2 mm, 17 sec.; (D) coronal T2 SSFSE, 1.0 x 1.6 x 4.0 mm, 47 sec.; and (E) MUSE b800, 4:22 min.
‡ Based on SIGNA™ Hero 3.0T data on file (2021).
D
Figure 3.
A 68-year-old patient with pain after ankle sprain. MR depicted a small internal osteochondral lesion in the talar dome and subtalar arthropathy. Images acquired with AIR™ MP Coil and (A-E) AIR™ Recon DL. (A) Sagittal PD FSE FatSat, 0.4 x 0.5 x 2.0 MM, 2:56 min.; (B) sagittal T1 FSE, 0.4 x 0.4 x 2.0 mm, 1:59 min.; (C) axial PD FSE FatSat, 0.3 x 0.3 x 3.0 mm, 2:48 min.; (D) coronal PD FSE FatSat, 0.4 x 0.5 x 2.0 mm, 2:37 min.; (E) coronal T1 FSE, 0.4 x 0.5 x 2.0 mm, 2:20 min.; and (F) coronal reformat of a sagittal oZTEo acquisition.
E
Figure 3.
A 68-year-old patient with pain after ankle sprain. MR depicted a small internal osteochondral lesion in the talar dome and subtalar arthropathy. Images acquired with AIR™ MP Coil and (A-E) AIR™ Recon DL. (A) Sagittal PD FSE FatSat, 0.4 x 0.5 x 2.0 MM, 2:56 min.; (B) sagittal T1 FSE, 0.4 x 0.4 x 2.0 mm, 1:59 min.; (C) axial PD FSE FatSat, 0.3 x 0.3 x 3.0 mm, 2:48 min.; (D) coronal PD FSE FatSat, 0.4 x 0.5 x 2.0 mm, 2:37 min.; (E) coronal T1 FSE, 0.4 x 0.5 x 2.0 mm, 2:20 min.; and (F) coronal reformat of a sagittal oZTEo acquisition.
F
Figure 3.
A 68-year-old patient with pain after ankle sprain. MR depicted a small internal osteochondral lesion in the talar dome and subtalar arthropathy. Images acquired with AIR™ MP Coil and (A-E) AIR™ Recon DL. (A) Sagittal PD FSE FatSat, 0.4 x 0.5 x 2.0 MM, 2:56 min.; (B) sagittal T1 FSE, 0.4 x 0.4 x 2.0 mm, 1:59 min.; (C) axial PD FSE FatSat, 0.3 x 0.3 x 3.0 mm, 2:48 min.; (D) coronal PD FSE FatSat, 0.4 x 0.5 x 2.0 mm, 2:37 min.; (E) coronal T1 FSE, 0.4 x 0.5 x 2.0 mm, 2:20 min.; and (F) coronal reformat of a sagittal oZTEo acquisition.


result
PREVIOUS
${prev-page}
NEXT
${next-page}



Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
IN PRACTICE
The making of a hero at Imapôle Lyon-Villeurbanne
The making of a hero at Imapôle Lyon-Villeurbanne
Radiology teams are facing more pressure than ever, as both patients and referring physicians demand accurate, fast and reliable results. To address these concerns, Imapôle Lyon–Villeurbanne in Lyon, France, installed the SIGNA™ Hero 3.0T MR system.
Radiology teams are facing more pressure than ever, as both patients and referring physicians demand accurate, fast and reliable results. To address these concerns, Imapôle Lyon–Villeurbanne in Lyon, France, installed the SIGNA™ Hero 3.0T MR system.
The clinic chose SIGNA™ Hero because it’s equipped with the latest technologies to improve imaging capabilities, reduce clinician burden and make difficult MR exams simpler. The system supports AIR™ Recon DL, GE’s deep-learning-based reconstruction algorithm, and intelligent applications such as AIR x™ and AIR Touch™ to ensure both challenging and routine examinations are completed more efficiently so patients spend less time on the table.
“I am now much more comfortable in my diagnoses, and the referring physicians are delighted with the image quality,” says Bertrand Peltier, MD, a radiologist at Imapôle Lyon–Villeurbanne. A large 70 cm bore gives patients more room and, combined with unique blanket-like AIR™ Coils, scanning is less cumbersome. AIR™ Coils also enable larger clinical coverage for whole-body workflows. That means fewer adjustments and more clinical exams.
“It’s a powerful combination of 3.0T and AIR™ Recon DL that’s designed for both patients and users,” says Cédric Poullaouëc, technologist at Imapôle Lyon–Villeurbanne.
Figure 1.
A 73-year-old patient assessed for atypical vertigo was found to have right APC type 2 schwannoma. (A) Axial reformat of a sagittal T2 FLAIR Cube, 1.0 x 1.0 x 1.3 mm, 3:24 min.; (B) coronal reformat of an axial T2 Cube, 0.5 x 0.5 x 0.5 mm, 2:53 min.; (C) axial T1 FSE, 0.5 x 0.7 x 1.5 mm, 2:15 min. with AIR™ Recon DL; and (D) axial T2 Cube, 0.5 x 0.5 x 0.5 mm, 2:53 min.
A seamless transition
SIGNA™ Hero uses intelligent magnet technology that is 1.4 times more efficient than previous models. It also uses 67% less helium and weighs nearly 4,190 lbs (1,900 kg) less than the previous generation magnet.‡ These features simplified the upgrade so the new system could be installed in the center’s existing 1.5T room. The facility simply updated the RF shielding without changing the quench tube or cooling network, which reduced construction costs.
“We’ve had a positive impression from the beginning. Our trepidation around installing a brand new system and moving from 1.5T to 3.0T was immediately resolved, thanks to the lighter weight of SIGNA™ Hero compared to other 3.0T MR systems,” says Samir Lounis, Executive Director at Imapôle Lyon–Villeurbanne.
Upgrading to a 3.0T system has had bottom-line benefits, allowing the facility to maximize its reimbursements from the French government. “Increasing the number of exams by speeding up the workflow is a real benefit,” Mr. Lounis adds.
Figure 2.
A 30-year-old patient with dyspnea for 6 months. Mediastinal mass found on CT, referred to MR to determine if mass is a thymoma or sarcoma. Images acquired with AIR™ AA Coil and (A-D) AIR™ Recon DL. (A) Axial T2 SSFSE FatSat, 1.2 x 1.8 x 4.0 mm, 37 sec.; (B) axial T2 SSFSE, 1.2 x 1.8 x 4.0 mm, 40 sec.; (C) axial LAVA Flex, 1.4 x 1.7 x 2.2 mm, 17 sec.; (D) coronal T2 SSFSE, 1.0 x 1.6 x 4.0 mm, 47 sec.; and (E) MUSE b800, 4:22 min.
A host of clinical benefits
With GE’s pioneering deep-learning-based technology
AIR™ Recon DL, technologists can achieve exceptional images faster for even broader clinical coverage. Scans can be completed up to 50% faster, making it a more comfortable experience for patients, too. Plus, radiologists can be more confident in the images acquired with easy-to-read, high-quality scans that may also reduce eye fatigue.
“The SIGNA™ Hero can probe deeper into the body and organs with excellent image quality. Smaller anatomical elements are visible in musculoskeletal (MSK); ear, nose and throat; and neuro exams. The radiologist can confidently validate the presence of an element or lesion,” adds Mr. Lounis.
Radiologists and technologists routinely use AIR™ technologies to increase exam efficiency and precision, as well as patient comfort.
“AIR x™ significantly increases reproducibility and reduces slice programming time,” says Mr. Lounis.
The AIR™ Coils further improve patient comfort, while delivering excellent images. “The ergonomic AIR™ Coils are great. It’s more comfortable when positioning the patient and it’s less claustrophobic, especially for neuro patients who use the 48-channel coil that doesn’t touch their forehead or shoulders. And I encounter far fewer artifacts,” says Mr. Poullaouëc.
AIR™ Recon DL has significantly improved the facility’s neuro scans of the pituitary gland, as well as MSK imaging of small structures on extremities such as the wrist and ankle. It also delivers higher SNR and shorter scan times. “I find that I can program more and thinner slices with less scan time,” adds Mr. Poullaouëc.
“In neuro scans, 2D AIR™ Recon DL image quality is significantly better than 3D quality with standard imaging,” says Mr. Lounis.
Figure 3.
A 68-year-old patient with pain after ankle sprain. MR depicted a small internal osteochondral lesion in the talar dome and subtalar arthropathy. Images acquired with AIR™ MP Coil and (A-E) AIR™ Recon DL. (A) Sagittal PD FSE FatSat, 0.4 x 0.5 x 2.0 MM, 2:56 min.; (B) sagittal T1 FSE, 0.4 x 0.4 x 2.0 mm, 1:59 min.; (C) axial PD FSE FatSat, 0.3 x 0.3 x 3.0 mm, 2:48 min.; (D) coronal PD FSE FatSat, 0.4 x 0.5 x 2.0 mm, 2:37 min.; (E) coronal T1 FSE, 0.4 x 0.5 x 2.0 mm, 2:20 min.; and (F) coronal reformat of a sagittal oZTEo acquisition.
The technology also helps deliver high-quality exams without lengthening scan time, which enables the SIGNA™ to scan more patients. “AIR™ Recon DL is used in routine protocols, as well as emergency protocols, which allows us to easily integrate an additional exam without overloading the session or penalizing other patients,” says Mr. Lounis.
Dr. Peltier says AIR™ Recon DL has significantly improved his clinical confidence, particularly in challenging anatomies or cases. “I can visualize more anatomical elements, such as a partial rupture of the ACL, damage to the scapho-ulnar or triangular ligaments in the wrist, and edema,” he explains.
The combination of AIR™ Recon DL, AIR™ Coils and AIR x™ has helped the clinic reduce repeat exams, while improving efficiency of technologists. “We’re efficient in conducting exams, and we can spend more time with patients. Working conditions appear to be easing, and feedback from satisfied patients contributes to this,” said Mr. Poullaouëc.
The system will allow the clinic to implement new sequences once they become available, such as MDSE in MR 30. They’re also exploring the use of Cube T2 FLAIR for hydrops, a pathological hallmark of Ménière’s disease.
The SIGNA™ Hero at Imapôle Lyon–Villeurbanne is currently the only 3.0T scanner east of Lyon in France. The excellent image quality is impressing referring physicians, which will allow the facility to further differentiate their MR imaging services from others in the area.
“It’s an extraordinary system,” says Mr. Lounis.