A
Figure 1.
(A) Coronal whole-body DWI and (B) sagittal spine STIR.
B
Figure 1.
(A) Coronal whole-body DWI and (B) sagittal spine STIR.
A
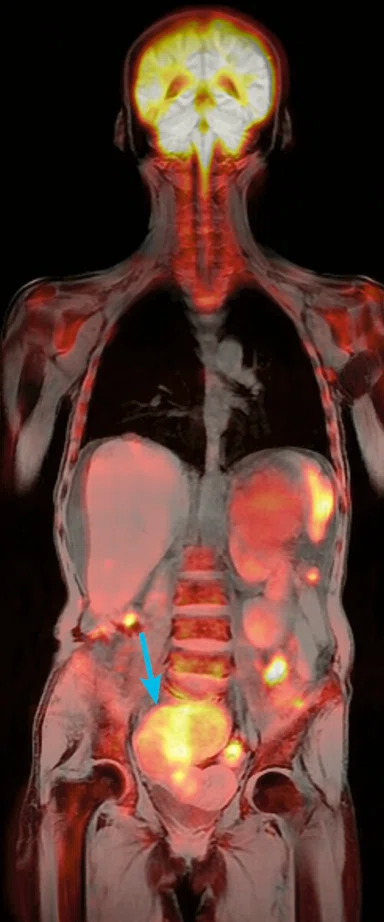
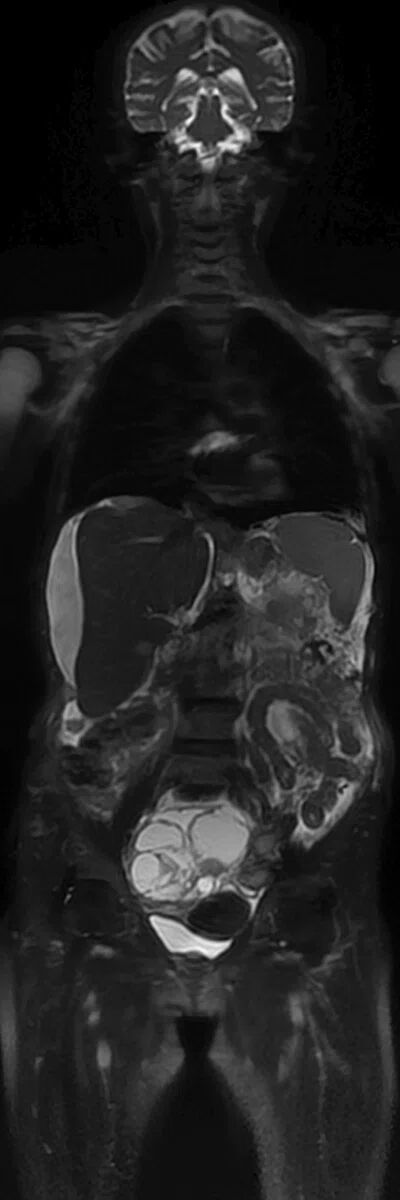
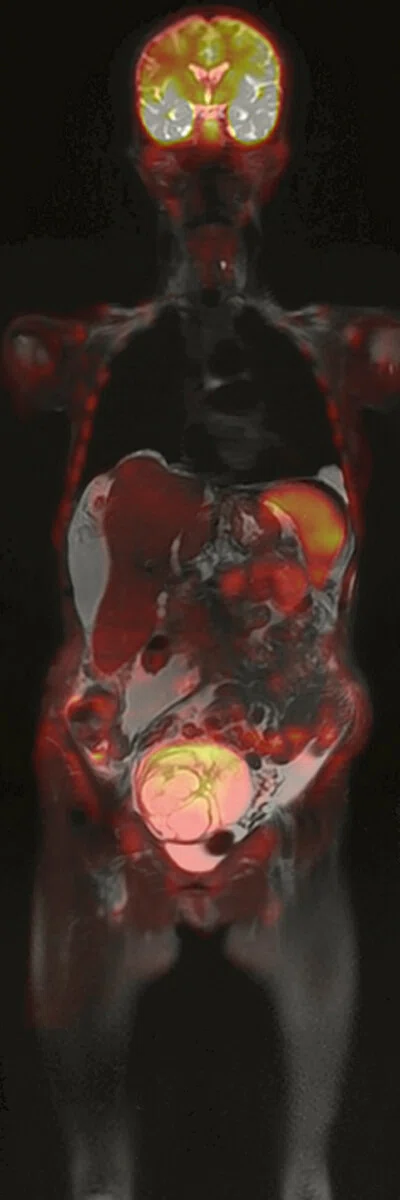
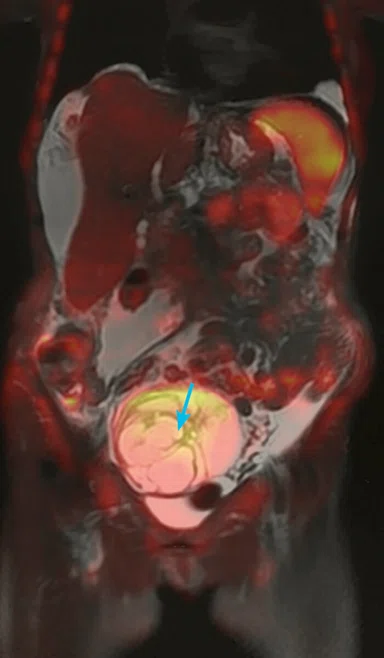
Figure 4.
(A) Coronal LAVA Flex and DWI fused; (B) coronal T2 SSFSE FatSat; and (C) coronal T2 SSFSE FatSat and DWI fused.
B
Figure 4.
(A) Coronal LAVA Flex and DWI fused; (B) coronal T2 SSFSE FatSat; and (C) coronal T2 SSFSE FatSat and DWI fused.
C
Figure 4.
(A) Coronal LAVA Flex and DWI fused; (B) coronal T2 SSFSE FatSat; and (C) coronal T2 SSFSE FatSat and DWI fused.
5 Barakat E, Kirchgesner T, Triqueneaux P, Galant C, Stoenoiu M, Lecouvet FE. Whole Body Magnetic Resonance Imaging in Rheumatic and Systemic Diseases From Emerging to Validated Indications. Magn Reson Imaging Clin N Am, 2018 Nov;26(4):581 597.
6 Lecouvet, F.E.; Van Nieuwenhove, S.;Jamar, F.; Lhommel, R.; Guermazi, A.; Pasoglou, V.P. Whole-Body MR Imaging The Novel, “Intrinsically Hybrid,” Approach to Metastases, Myeloma, Lymphoma, in Bones and Beyond. PET Clin, 2018 Oct;13(4):505-522.
1 Lecouvet FE, Talbot JN. Monitoring the response of bone metastases to treatment with magnetic resonance imaging and nuclear medicine techniques: A review and position statement by the European organization for research and treatment of cancer imaging group. Eur. J. Cancer 2014;50:2519–2531.
2 Barchetti F, Stagnitti A. Unenhanced whole-body MRI versus PET-CT for the detection of prostate cancer metastases after primary treatment. Eur. Rev. Med. Pharmacol. Sci. 2016;20:3770–3776.
3 Jambor I, Kuisma A. Prospective evaluation of planar bone scintigraphy, SPECT, SPECT/CT, PET/CT and whole body 1.5T MRI, including DWI, for the detection of bone metastases in high risk breast and prostate cancer patients: SKELETA clinical trial. Acta Oncol. 2016;55:59–67.
4 Villani MF, Tanturri de Horatio L, Garganese MC, et al. Whole-Body MRI versus bone scintigraphy: which is the best diagnostic tool in patients with chronic recurrent multifocal osteomyelitis (CRMO)? From 8th International Congress of Familial Mediterranean Fever and Systemic Autoinflammatory Diseases Dresden, Germany. 30 September - 3 October 2015.
A
Figure 5.
(A) Coronal T2 SSFSE FatSat and DWI fused and (B) coronal whole-body DWI.
B
Figure 5.
(A) Coronal T2 SSFSE FatSat and DWI fused and (B) coronal whole-body DWI.
A
Figure 2.
(A) Coronal LAVA Flex and DWI fused and (B) coronal DWI.
B
Figure 2.
(A) Coronal LAVA Flex and DWI fused and (B) coronal DWI.
A
Figure 3.
(A) Inverted coronal whole-body DWI and (B) coronal whole-body LAVA Flex.
B
Figure 3.
(A) Inverted coronal whole-body DWI and (B) coronal whole-body LAVA Flex.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
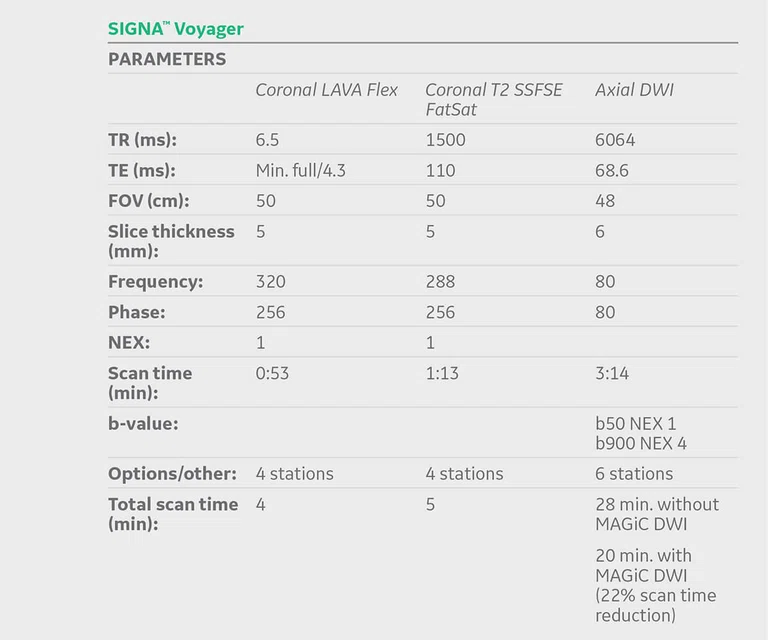
CASE STUDIES
Whole-body imaging for oncology patients
Whole-body imaging for oncology patients
By Costy Kheir, MD, Head of the Medical Imaging Department, Haykel Hospital, Tripoli, Lebanon
Whole-body MR imaging has been utilized in clinical practice for over a decade. However, recent improvements in system hardware and sequences, particularly diffusion-weighted imaging (DWI), have increased image quality and reduced acquisition time. Several recently published studies demonstrated the high sensitivity and specificity of this technique that surpasses those of bone scintigraphy and rivals those of PET/CT and PET/MR for cancer detection, staging and treatment monitoring.1-4 Whole-body MR is also being used for the diagnosis and evaluation of systemic and inflammatory diseases.5,6 Some centers venture to use it as a screening tool for healthy patients. Furthermore, it is an important tool for cancer detection and monitoring in children and pregnant women.
In Lebanon, access to PET/CT is limited and it is often not reimbursed by third-party payers. In fact, our country continues to suffer from an economic crisis that has impacted national health policy and left many patients without proper medical coverage. As the incidence of all types of cancer continues to increase in our country, whole-body MR is emerging as an alternative exam for diagnosing these patients at less cost than PET.
To provide more rigorous diagnostic and treatment pathways for our patients, we installed SIGNA™ Voyager in May 2018. Whole-body MR provides non-ionizing radiation and non-contrast exams. In the case of oncology patients, it can be repeated often to monitor treatment response without the added concern for a patient’s total exposure to ionizing radiation. MR can scan the entire body for physical abnormalities, depict tumors in early formative stages and deliver an overall snapshot of a patient’s general health.
A whole-body MR exam typically consists of the following core sequences: T1-weighted, T2-weighted STIR, T2 Single Shot Fast Spin Echo (SSFSE), FatSat and DWI. Combined, these sequences allow the radiologist to thoroughly assess the anatomy, body composition and functional information of the whole body.
There are certain considerations to address when implementing whole-body MR. The protocol must be robust and accurate to deliver the information the radiologist needs for interpretation. It should also be as fast as possible to ease the patient’s experience.
Scan orientation is typically in the coronal plane. The radiologist will need to adapt to viewing the anatomy in this plane if no multi-planar reconstruction is available. Patient motion and magnetic field distortions, such as susceptibility effects, are common issues impacting image quality and resolution. Also, exam times can take up to 60 minutes, which can be difficult for the patient even when using a wide bore magnet.
To overcome these burdens, we worked with GE Healthcare clinical applications specialists to implement our whole-body MR protocols and achieve gains in spatial and temporal resolution. We opted to use T1 LAVA Flex, which provides excellent reliability for fat/water separation to enable the assessment of body composition. Instead of T2 STIR we selected T2 SSFSE FatSat, which provides shorter acquisition times compared to FSE and better resolution with excellent FatSat homogeneity. We were able to acquire a slice thickness of 5 mm with consecutive cuts, preserving a high SNR.
In July 2019 we upgraded our SIGNA™ Voyager to expand the SIGNA™Works productivity platform, including HyperWorks. The upgrade provides value-added technologies that are flexible and customizable to meet our imaging needs and workload.
While we have integrated HyperSense and HyperCube in many of our daily protocols, we found that MAGiC DWI had the most significant impact in whole-body MR exams. With MAGiC DWI, we can shorten acquisition times by using two b-values with low NEX values and then synthesize the higher b-value images. Previously, conventional whole-body DWI exams would take 60 minutes; now, by incorporating MAGiC DWI instead of the conventional DWI, the total exam time is down to 45 minutes, on average. The results of calculating multiple b-values from a single MAGiC DWI scan are more than satisfactory.
There is a saying that it takes a village to raise a child. When it comes to healthcare, it takes a community to make a difference in patient care. The GE MR community, through continued innovation and the sharing of best practices, is helping us to deliver higher quality care for our patients.
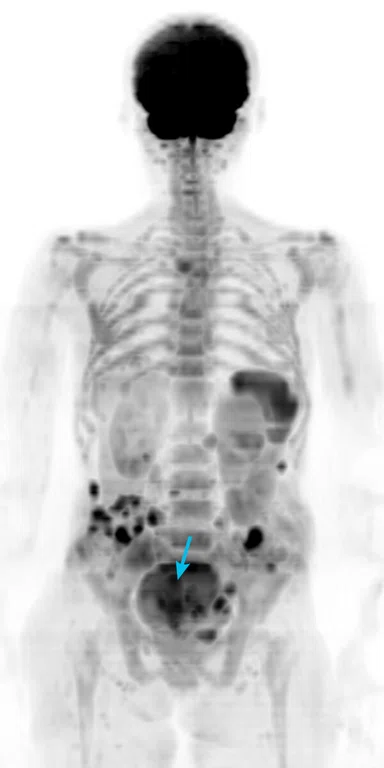
Case 1
Patient history
A 61-year-old man weighing 90 kg (198 lbs.) was referred to our institution for follow-up of multiple myeloma while undergoing treatment. No prior exams (e.g., PET/CT) were available; comparison was performed with a prior whole-body MR performed at another hospital.
MR findings
Restriction on eDWI sequence receded on the scapular and rib lesions that were described in the prior MR exam and on both parotid glands and thoracic spine. However, there was accentuated diffusion restriction showing multiple lesions of the pelvic girdle and both femurs, proximally. Several active lesions were also noted on the lumbar spine.
These findings are consistent with disease progression, although several lesions in the upper body did respond to treatment. As a result of this whole-body MR exam, the treatment protocol was adjusted accordingly.
Discussion
The benefit of whole-body MR being accessible and repeatable with no radiation, contrast media or other side effects will affect and reshape treatment processes in oncology imaging. We anticipate this will impact patient response and outcomes, as well as enable lower costs in our healthcare system by alleviating the need for additional tests and shortening treatment duration.
The approach of combining multiple sequences in the whole-body MR protocol provides the information the radiologist needs to be more confident about the anatomy, inflammatory changes and pathological correlation with the diffusion restriction. Interestingly, fusing the eDWI and the T1 LAVA Flex images delivers a similar appearance as PET/MR images, with the difference being the absence of nucleic secretion in the kidneys and bladder, which prohibits the detection of lesions in these areas. Normal diffusion restriction of the spleen was not an issue for depicting a lesion.
SIGNA™ Voyager has great potential to deliver diagnostic images with high SNR while allowing us to maintain shortened exam times for the whole-body protocol. New emerging protocols that deliver shorter acquisition times and better resolution, as well as new higher channel arrays, such as the AIR™ Coils, will further boost these qualities and help promote whole-body MR for oncology imaging.
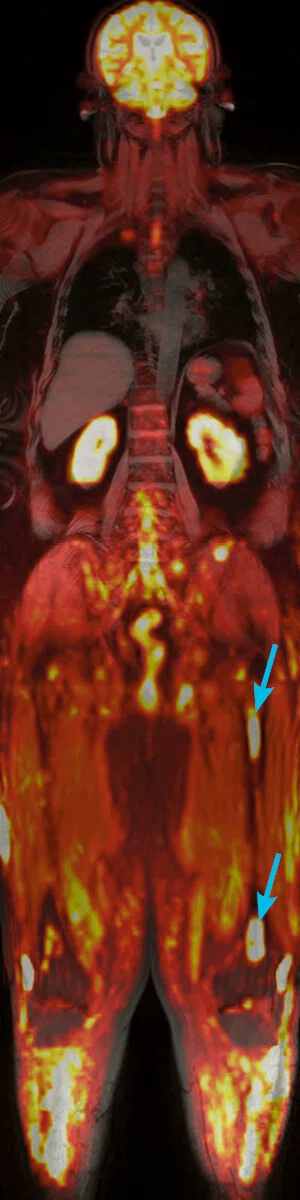
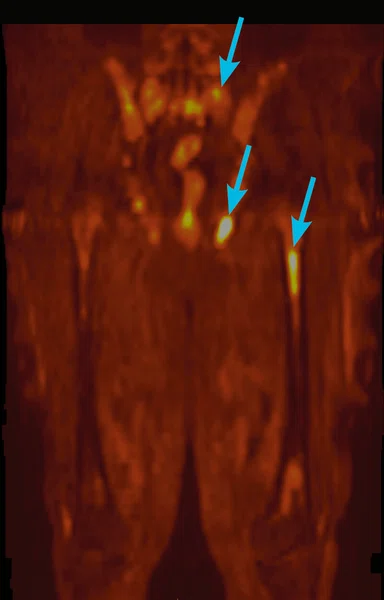
Case 2
Patient history
A 60-year-old woman weighing 45 kg (99 lbs.) was referred for a whole-body MR for investigation of a pelvic mass. No other prior history was known.
MR findings
Whole-body DWI depicted a complex pelvic mass measuring approximately 10 cm, most likely of right adnexal origin that could represent a cystadenocarcinoma requiring histological confirmation. There were multiple peritoneal metastatic seedings but also metastases in the lymph nodes, the liver and bones as shown by the whole-body DWI with ADC map confirmation. Abundant ascites were found around the liver and the pelvis. A large left renal simple cyst was also noted.Most interesting was that the whole-body DWI demonstrated the pelvic lesion and metastases in the same exam. While whole-body MR is not typically recommended for diagnosis of primary lesions, the acquisition depicted the disease and its spread in the abdominal and pelvic cavities. In one exam, MR provided the clinician with a detailed status of visceral and bone spread, removing the need for additional imaging tests such as CT or bone scintigraphy.