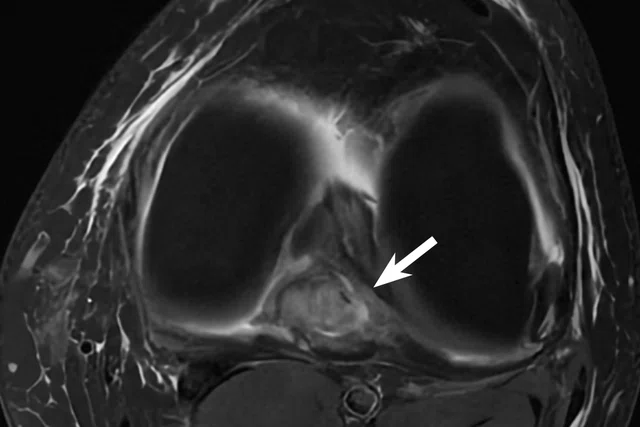
A
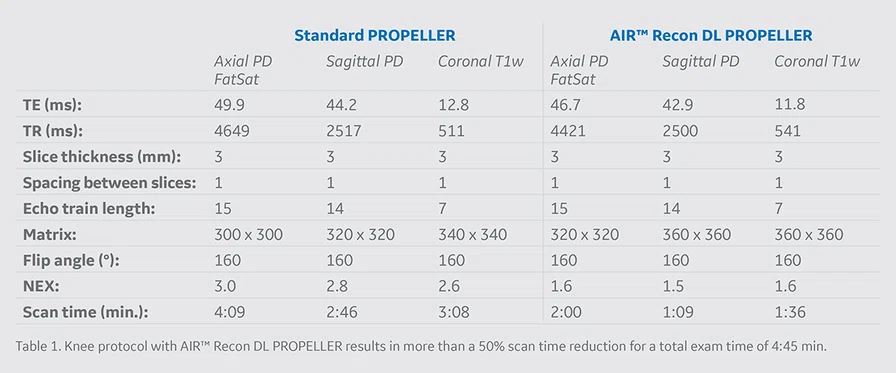
Figure 1.
Case 1: A 42-year-old patient with a PCL tear (arrow). (A) Sagittal PD and (C) axial PD FatSat PROPELLER with conventional reconstruction. (B) Sagittal PD and (D) axial PD FatSat with AIR™ Recon DL PROPELLER reconstruction.
B
Figure 1.
Case 1: A 42-year-old patient with a PCL tear (arrow). (A) Sagittal PD and (C) axial PD FatSat PROPELLER with conventional reconstruction. (B) Sagittal PD and (D) axial PD FatSat with AIR™ Recon DL PROPELLER reconstruction.
C
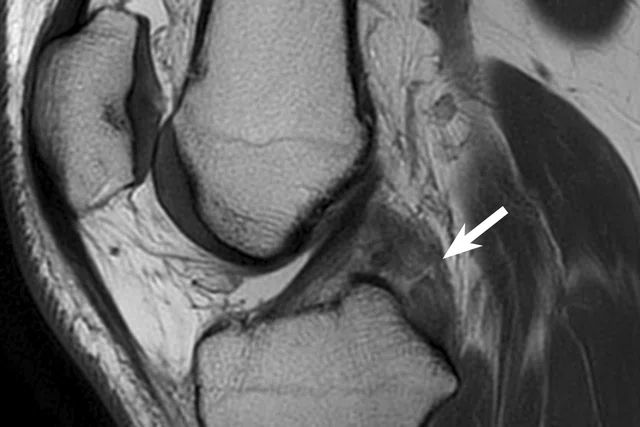
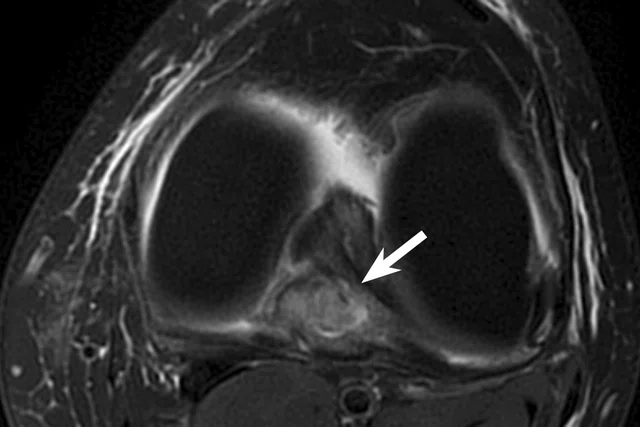
Figure 1.
Case 1: A 42-year-old patient with a PCL tear (arrow). (A) Sagittal PD and (C) axial PD FatSat PROPELLER with conventional reconstruction. (B) Sagittal PD and (D) axial PD FatSat with AIR™ Recon DL PROPELLER reconstruction.
D
Figure 1.
Case 1: A 42-year-old patient with a PCL tear (arrow). (A) Sagittal PD and (C) axial PD FatSat PROPELLER with conventional reconstruction. (B) Sagittal PD and (D) axial PD FatSat with AIR™ Recon DL PROPELLER reconstruction.
A
Figure 2.
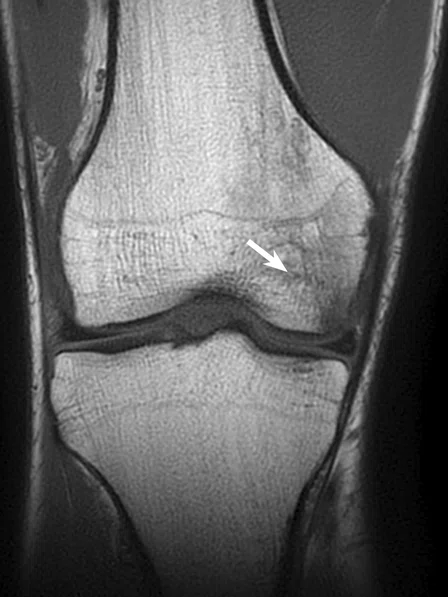
Case 2: A 50-year-old patient with bone marrow edema of the medial femoral condyle (arrow). (A) Coronal T1w PROPELLER and (C) axial PD FatSat PROPELLER with conventional reconstruction. (B) Coronal T1w and (D) axial PD FatSat with AIR™ Recon DL PROPELLER.
B
Figure 2.
Case 2: A 50-year-old patient with bone marrow edema of the medial femoral condyle (arrow). (A) Coronal T1w PROPELLER and (C) axial PD FatSat PROPELLER with conventional reconstruction. (B) Coronal T1w and (D) axial PD FatSat with AIR™ Recon DL PROPELLER.
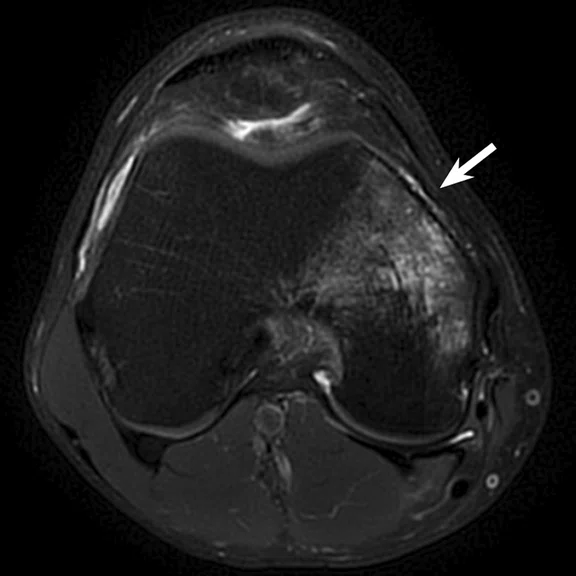
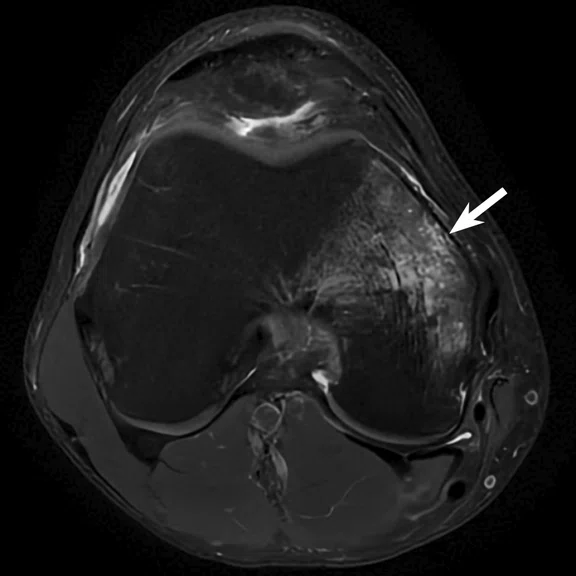
C
Figure 2.
Case 2: A 50-year-old patient with bone marrow edema of the medial femoral condyle (arrow). (A) Coronal T1w PROPELLER and (C) axial PD FatSat PROPELLER with conventional reconstruction. (B) Coronal T1w and (D) axial PD FatSat with AIR™ Recon DL PROPELLER.
D
Figure 2.
Case 2: A 50-year-old patient with bone marrow edema of the medial femoral condyle (arrow). (A) Coronal T1w PROPELLER and (C) axial PD FatSat PROPELLER with conventional reconstruction. (B) Coronal T1w and (D) axial PD FatSat with AIR™ Recon DL PROPELLER.
A
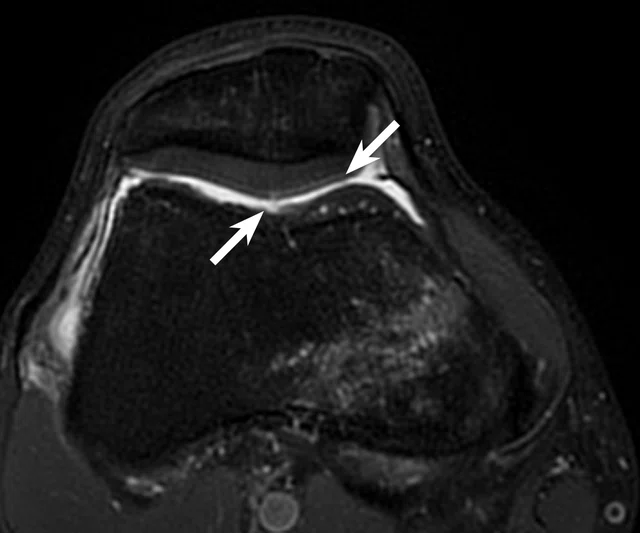
Figure 3.
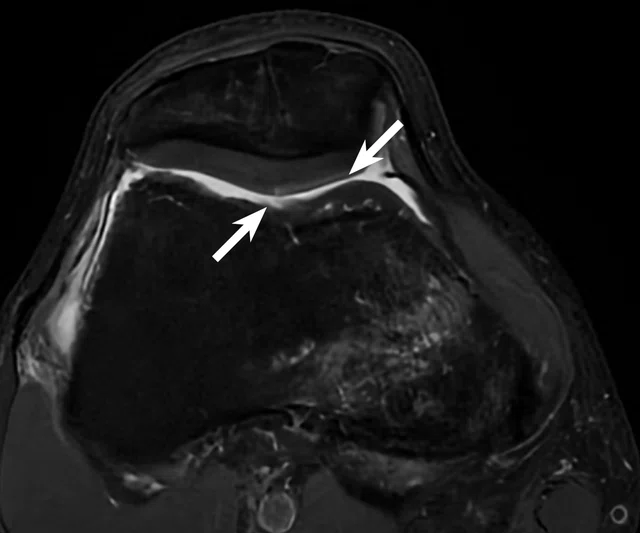
Case 3: A 39-year-old patient with a non-displaced delamination of retropatellar cartilage. (A) Conventional axial PD and (B) AIR™ Recon DL PROPELLER axial PD images.
B
Figure 3.
Case 3: A 39-year-old patient with a non-displaced delamination of retropatellar cartilage. (A) Conventional axial PD and (B) AIR™ Recon DL PROPELLER axial PD images.
A
Figure 4.
Comparison of MR imaging processed with (A, C, E, G) conventional PROPELLER reconstruction and (B, D, F, H) AIR™ Recon DL PROPELLER.
B
Figure 4.
Comparison of MR imaging processed with (A, C, E, G) conventional PROPELLER reconstruction and (B, D, F, H) AIR™ Recon DL PROPELLER.
C
Figure 4.
Comparison of MR imaging processed with (A, C, E, G) conventional PROPELLER reconstruction and (B, D, F, H) AIR™ Recon DL PROPELLER.
D
Figure 4.
Comparison of MR imaging processed with (A, C, E, G) conventional PROPELLER reconstruction and (B, D, F, H) AIR™ Recon DL PROPELLER.
E
Figure 4.
Comparison of MR imaging processed with (A, C, E, G) conventional PROPELLER reconstruction and (B, D, F, H) AIR™ Recon DL PROPELLER.
F
Figure 4.
Comparison of MR imaging processed with (A, C, E, G) conventional PROPELLER reconstruction and (B, D, F, H) AIR™ Recon DL PROPELLER.
G
Figure 4.
Comparison of MR imaging processed with (A, C, E, G) conventional PROPELLER reconstruction and (B, D, F, H) AIR™ Recon DL PROPELLER.
H
Figure 4.
Comparison of MR imaging processed with (A, C, E, G) conventional PROPELLER reconstruction and (B, D, F, H) AIR™ Recon DL PROPELLER.
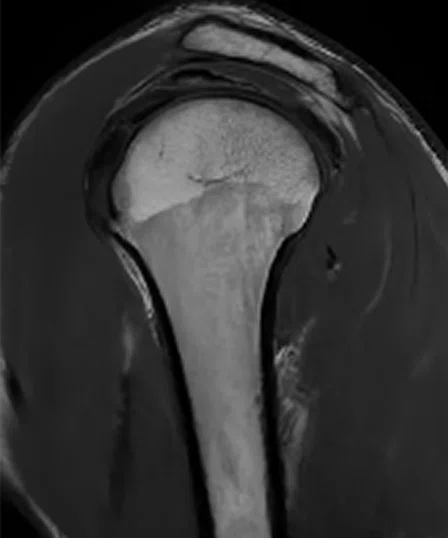
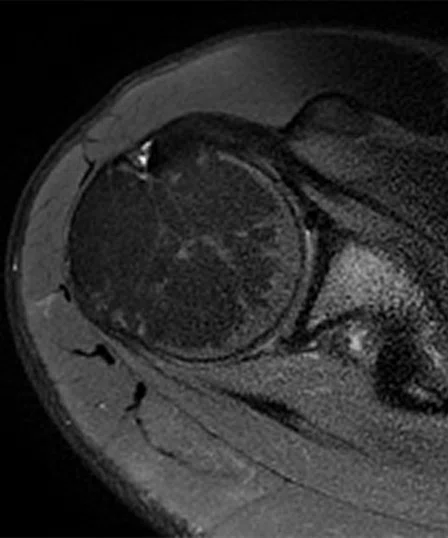
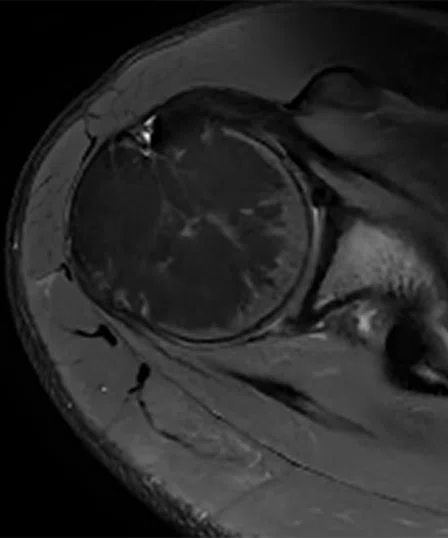
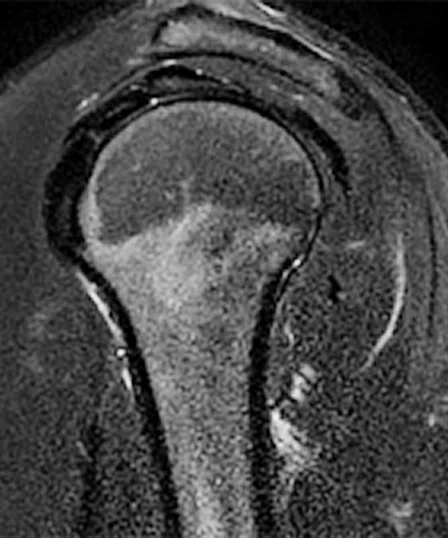
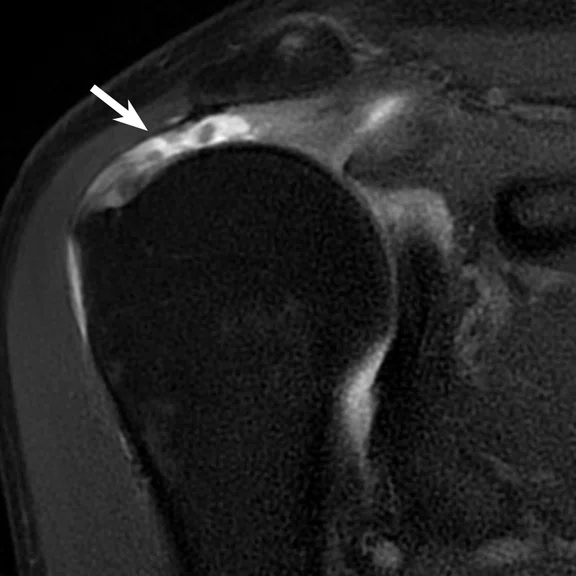
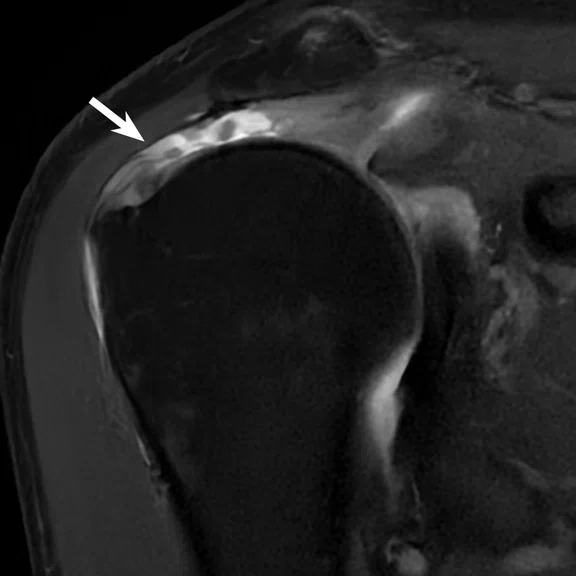
A
Figure 5.
Case 4: A 53-year-old patient with a full-thickness tear of the supraspinatus tendon (arrow). (A) coronal PD FatSat PROPELLER and (C) sagittal PD FatSat PROPELLER with conventional reconstruction and (B) coronal PD FatSat and (D) sagittal PD FatSat with AIR™ Recon DL PROPELLER.
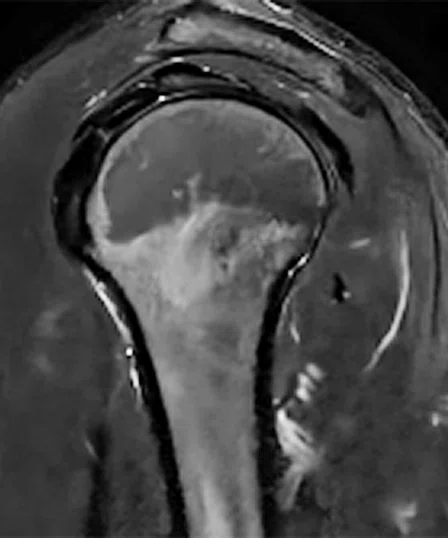
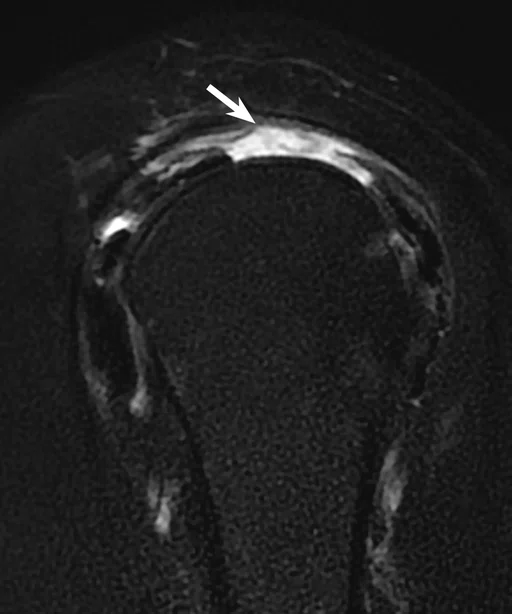
B
Figure 5.
Case 4: A 53-year-old patient with a full-thickness tear of the supraspinatus tendon (arrow). (A) coronal PD FatSat PROPELLER and (C) sagittal PD FatSat PROPELLER with conventional reconstruction and (B) coronal PD FatSat and (D) sagittal PD FatSat with AIR™ Recon DL PROPELLER.
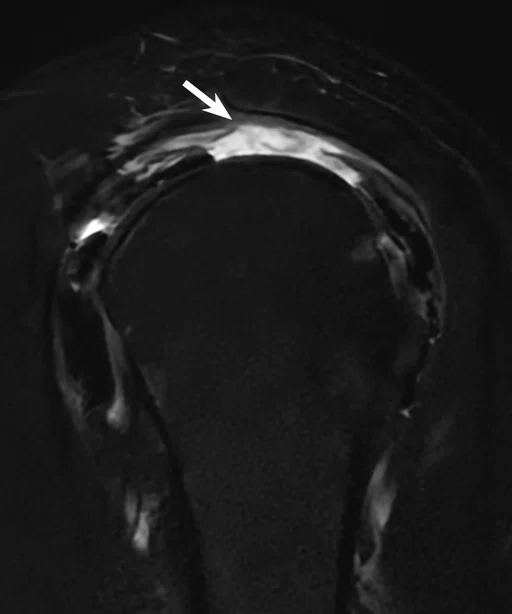
C
Figure 5.
Case 4: A 53-year-old patient with a full-thickness tear of the supraspinatus tendon (arrow). (A) coronal PD FatSat PROPELLER and (C) sagittal PD FatSat PROPELLER with conventional reconstruction and (B) coronal PD FatSat and (D) sagittal PD FatSat with AIR™ Recon DL PROPELLER.
D
Figure 5.
Case 4: A 53-year-old patient with a full-thickness tear of the supraspinatus tendon (arrow). (A) coronal PD FatSat PROPELLER and (C) sagittal PD FatSat PROPELLER with conventional reconstruction and (B) coronal PD FatSat and (D) sagittal PD FatSat with AIR™ Recon DL PROPELLER.
1. Kaniewska M, Deininger-Czermak E, Getzmann JM, Wang X, Lohezic M, Guggenberger R. Application of deep learning-based image reconstruction in MR imaging of the shoulder joint to improve image quality and reduce scan time. Eur Radiol. 2023;33(3):1513-1525.
2. Kaniewskaa M, Deininger-Czermaka E, Lohezic M, Enslea F, Guggenberger R. Combination of deep learning convolutional neural network reconstruction and radial k-space acquisition MR technique for imaging of the knee: impact on image quality and diagnostic performance. Scientific Reports (in review).
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
IN PRACTICE
Accelerated, motion-robust imaging of the shoulder and knee joints
Accelerated, motion-robust imaging of the shoulder and knee joints
By Malwina Kaniewska-Pelczar, MD, Senior Physician, and Roman Guggenberger, MD, Professor of Radiology and Head of MSK Imaging, Institute for Diagnostic and Interventional Radiology, University Hospital Zürich, Zürich, Switzerland
MR is the preferred imaging modality for the assessment of soft tissues in and around joints and is thus widely used in musculoskeletal (MSK) imaging.
MR is the preferred imaging modality for the assessment of soft tissues in and around joints and is thus widely used in musculoskeletal (MSK) imaging.
For instance, structures in and around the shoulder joint, such as rotator cuff tendons, biceps tendon, labrum and cartilage, as well as respective pathologies, can be depicted with high accuracy. When imaging the knee joint, MR allows precise visualization of internal and external structures of the knee joint, such as menisci, cruciate and collateral ligaments; cartilage; and soft tissues, such as muscle and fat around the joint. In these cases, fast spin echo (FSE) sequences are usually acquired in 2D or 3D, resulting in the acquisition of high-resolution images in different contrast weightings.
However, motion artifacts caused by blood flow of the adjacent vessels, patient motion or breathing can degrade image quality and may be an important limiting factor when reporting MR exams.
In clinical practice, different strategies can be implemented to mitigate motion artifacts: accelerating acquisition to shorten scan time, limit patient discomfort and reduce the likelihood of motion occurring during the scan, or using motion-robust sequences such as PROPELLER. Until now, acceleration techniques available on commercial scanners, such as parallel imaging or compressed sensing, have enabled a significant reduction in scan time in MSK imaging. However, these come at the cost of lower signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) compared to conventional acquisition techniques. In contrast, AIR™ Recon DL allows the acceleration of MR scanning while maintaining optimal image contrast and simultaneously reducing image noise. However, prior to MR 30 for SIGNA™, AIR™ Recon DL was only compatible with 2D Cartesian acquisitions, such as standard FSE imaging.
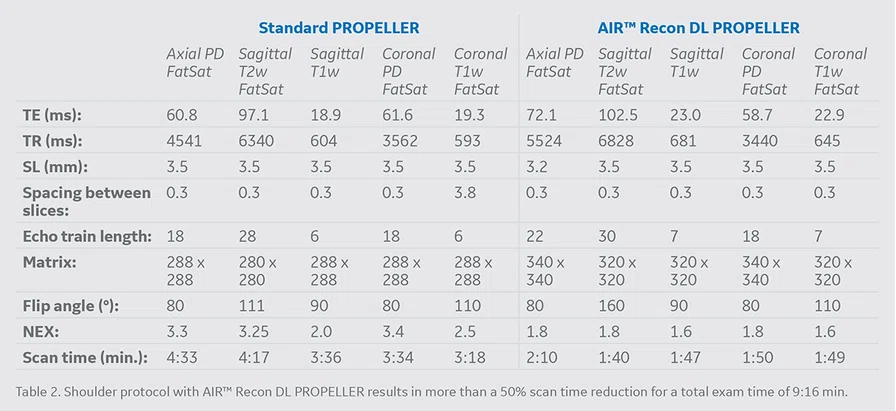
Our institution was involved in the clinical evaluation of AIR™ Recon DL PROPELLER, an extension of AIR™ Recon DL to the PROPELLER acquisition technique, in order to assess its potential to simultaneously reduce motion artifacts and image noise in addition to delivering substantial scan time reductions for MSK imaging at 1.5T.1,2 Protocols were optimized for multi-contrast examination of the knee (Table 1) and shoulder (Table 2). Accelerated scan time was below 5 minutes and 10 minutes, respectively, thus resulting in more than a 50% scan time reduction compared to our standard PROPELLER examination. AIR™ Recon DL PROPELLER allowed us to recover image quality in the final images, both in terms of SNR and CNR, and AIR™ Recon DL reconstructed images overall delivered the same diagnostic power compared to standard PROPELLER images, but with increased accuracy for certain anatomies, e.g. retropatellar cartilage.
Case 1
A PCL tear in a 42-year-old patient.
Case 2
A 50-year-old patient with bone marrow edema of the medial femoral condyle.
Case 3
A 39-year-old patient with a non-displaced delamination of retropatellar cartilage.
Case 4
Full-thickness tear of supraspinatus tendon in a 53-year-old patient.
Conclusion
MR imaging of the knee and shoulder using accelerated PROPELLER sequences combined with AIR™ Recon DL showed significantly higher image quality and diagnostic confidence compared to the standard PROPELLER sequences, while reducing scan time substantially. Both sequences performed comparably in the detection of knee or shoulder joint pathologies, while in the retropatellar cartilage case, the AIR™ Recon DL PROPELLER images were found to be superior for evaluation of the lesion.
These findings suggest that a combination of the PROPELLER acquisition and AIR™ Recon DL (e.g., AIR™ Recon DL PROPELLER) may become the new standard protocol in our institution for motion-artifact-free, fast MR imaging of large joints, such as the shoulder and knee