A
Figure 1.
AIR™ Recon DL and AIR™ Anterior Array Coil improve SNR and coverage in liver HCC cases. (A) Coronal T2 SnapShot SSFSE, 1.25 x 1.8 x 5.5 mm, 35 sec.; (B) axial T2 SnapShot SSFSE, 1.3 x 1.6 x 5.0 mm, 53 sec.; and (C) axial T2 SnapShot SSFSE ASPIR, 1.3 x 1.6 x 5.0 mm, 53 sec.
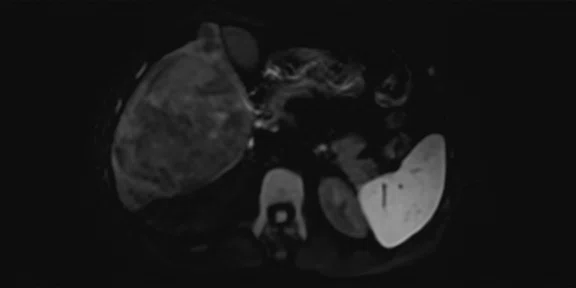
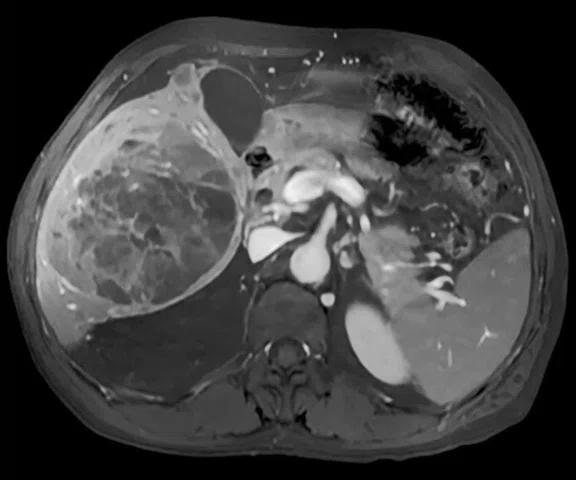
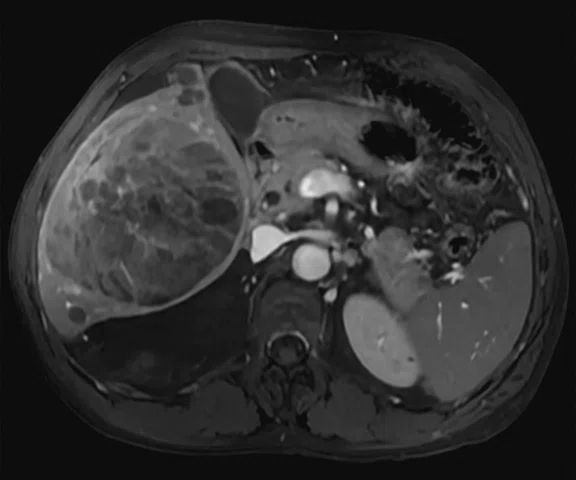
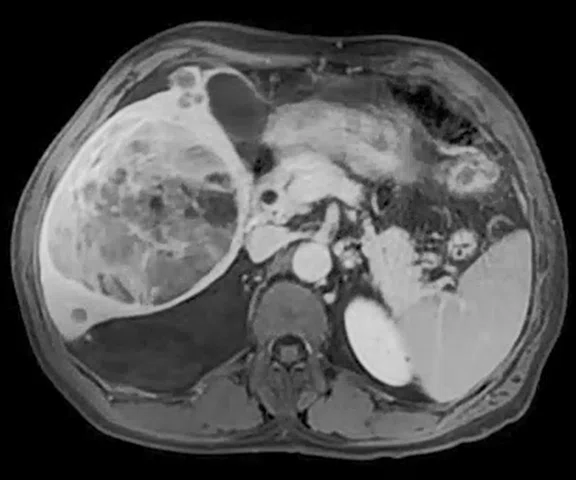
B-1
Figure 1.
AIR™ Recon DL and AIR™ Anterior Array Coil improve SNR and coverage in liver HCC cases. (A) Coronal T2 SnapShot SSFSE, 1.25 x 1.8 x 5.5 mm, 35 sec.; (B) axial T2 SnapShot SSFSE, 1.3 x 1.6 x 5.0 mm, 53 sec.; and (C) axial T2 SnapShot SSFSE ASPIR, 1.3 x 1.6 x 5.0 mm, 53 sec.
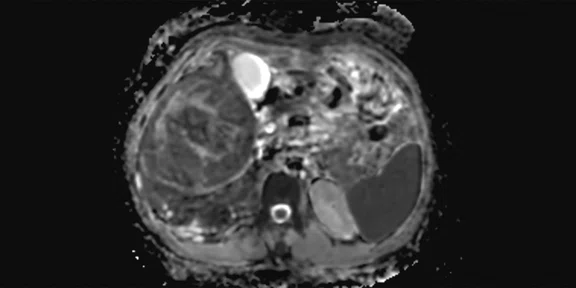
B-2
Figure 1.
AIR™ Recon DL and AIR™ Anterior Array Coil improve SNR and coverage in liver HCC cases. (A) Coronal T2 SnapShot SSFSE, 1.25 x 1.8 x 5.5 mm, 35 sec.; (B) axial T2 SnapShot SSFSE, 1.3 x 1.6 x 5.0 mm, 53 sec.; and (C) axial T2 SnapShot SSFSE ASPIR, 1.3 x 1.6 x 5.0 mm, 53 sec.
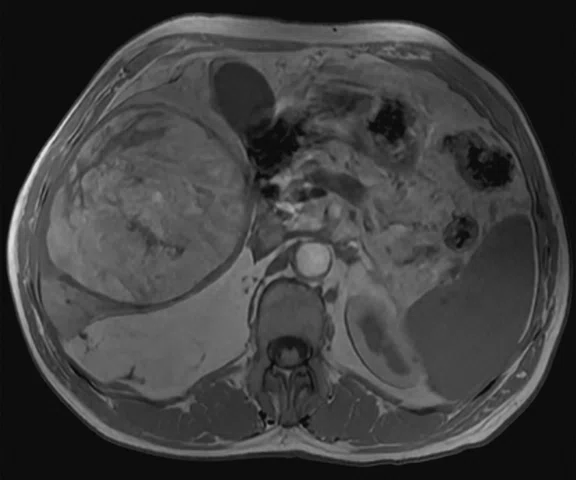
C-1
Figure 1.
AIR™ Recon DL and AIR™ Anterior Array Coil improve SNR and coverage in liver HCC cases. (A) Coronal T2 SnapShot SSFSE, 1.25 x 1.8 x 5.5 mm, 35 sec.; (B) axial T2 SnapShot SSFSE, 1.3 x 1.6 x 5.0 mm, 53 sec.; and (C) axial T2 SnapShot SSFSE ASPIR, 1.3 x 1.6 x 5.0 mm, 53 sec.
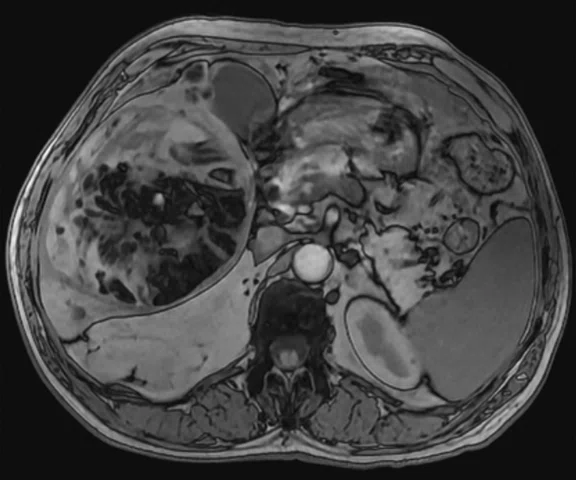
C-2
Figure 1.
AIR™ Recon DL and AIR™ Anterior Array Coil improve SNR and coverage in liver HCC cases. (A) Coronal T2 SnapShot SSFSE, 1.25 x 1.8 x 5.5 mm, 35 sec.; (B) axial T2 SnapShot SSFSE, 1.3 x 1.6 x 5.0 mm, 53 sec.; and (C) axial T2 SnapShot SSFSE ASPIR, 1.3 x 1.6 x 5.0 mm, 53 sec.
A
Figure 2.
Axial eDWI, b50-b700 acquisition with AIR™ Recon DL. (A) eDWI b700, 3.0 x 3.0 x 5.0 mm, 3:36 min. and (B) ADC map.
B
Figure 2.
Axial eDWI, b50-b700 acquisition with AIR™ Recon DL. (A) eDWI b700, 3.0 x 3.0 x 5.0 mm, 3:36 min. and (B) ADC map.
A
Figure 3.
Volumetric acquisition of the abdomen with (A) T2 Cube FatSat with Auto Navigator for free-breathing acquisition, 1.5 x 1.7 x 2.0 mm, 3:35 min., enabling reformatting to (B) sagittal and (C) axial planes.
B
Figure 3.
Volumetric acquisition of the abdomen with (A) T2 Cube FatSat with Auto Navigator for free-breathing acquisition, 1.5 x 1.7 x 2.0 mm, 3:35 min., enabling reformatting to (B) sagittal and (C) axial planes.
C
Figure 3.
Volumetric acquisition of the abdomen with (A) T2 Cube FatSat with Auto Navigator for free-breathing acquisition, 1.5 x 1.7 x 2.0 mm, 3:35 min., enabling reformatting to (B) sagittal and (C) axial planes.
A
Figure 4.
Dynamic DISCO with HyperSense, AIR™ Recon and AIR™ AA Coil. (A) Pre-contrast, (B) arterial phase 1, (C) arterial phase 2, (D) arterial phase 3, (E) portal phase and (F) equilibrium, all acquired at 1.3 x 2.0 x 2.0 mm.
B
Figure 4.
Dynamic DISCO with HyperSense, AIR™ Recon and AIR™ AA Coil. (A) Pre-contrast, (B) arterial phase 1, (C) arterial phase 2, (D) arterial phase 3, (E) portal phase and (F) equilibrium, all acquired at 1.3 x 2.0 x 2.0 mm.
C
Figure 4.
Dynamic DISCO with HyperSense, AIR™ Recon and AIR™ AA Coil. (A) Pre-contrast, (B) arterial phase 1, (C) arterial phase 2, (D) arterial phase 3, (E) portal phase and (F) equilibrium, all acquired at 1.3 x 2.0 x 2.0 mm.
D
Figure 4.
Dynamic DISCO with HyperSense, AIR™ Recon and AIR™ AA Coil. (A) Pre-contrast, (B) arterial phase 1, (C) arterial phase 2, (D) arterial phase 3, (E) portal phase and (F) equilibrium, all acquired at 1.3 x 2.0 x 2.0 mm.
E
Figure 4.
Dynamic DISCO with HyperSense, AIR™ Recon and AIR™ AA Coil. (A) Pre-contrast, (B) arterial phase 1, (C) arterial phase 2, (D) arterial phase 3, (E) portal phase and (F) equilibrium, all acquired at 1.3 x 2.0 x 2.0 mm.
F
Figure 4.
Dynamic DISCO with HyperSense, AIR™ Recon and AIR™ AA Coil. (A) Pre-contrast, (B) arterial phase 1, (C) arterial phase 2, (D) arterial phase 3, (E) portal phase and (F) equilibrium, all acquired at 1.3 x 2.0 x 2.0 mm.
A
Figure 5.
(A, B) Axial 2D T1w dual echo FSPGR, 1.1 x 1.6 x 5.0 mm, 51 sec., (A) in phase and (B) out of phase; (C, D) axial post-contrast FSPGR FatSat, 1.4 x 1.4 x 5.0 mm, 51 sec.; and (E) axial free-breathing 3D LAVA Star, 1.3 x 1.3 x 2.0 mm, 1:45 min. (A–D) Acquired with AIR™ Recon DL and (E) acquired with AIR™ Recon.
B
Figure 5.
(A, B) Axial 2D T1w dual echo FSPGR, 1.1 x 1.6 x 5.0 mm, 51 sec., (A) in phase and (B) out of phase; (C, D) axial post-contrast FSPGR FatSat, 1.4 x 1.4 x 5.0 mm, 51 sec.; and (E) axial free-breathing 3D LAVA Star, 1.3 x 1.3 x 2.0 mm, 1:45 min. (A–D) Acquired with AIR™ Recon DL and (E) acquired with AIR™ Recon.
C
Figure 5.
(A, B) Axial 2D T1w dual echo FSPGR, 1.1 x 1.6 x 5.0 mm, 51 sec., (A) in phase and (B) out of phase; (C, D) axial post-contrast FSPGR FatSat, 1.4 x 1.4 x 5.0 mm, 51 sec.; and (E) axial free-breathing 3D LAVA Star, 1.3 x 1.3 x 2.0 mm, 1:45 min. (A–D) Acquired with AIR™ Recon DL and (E) acquired with AIR™ Recon.
D
Figure 5.
(A, B) Axial 2D T1w dual echo FSPGR, 1.1 x 1.6 x 5.0 mm, 51 sec., (A) in phase and (B) out of phase; (C, D) axial post-contrast FSPGR FatSat, 1.4 x 1.4 x 5.0 mm, 51 sec.; and (E) axial free-breathing 3D LAVA Star, 1.3 x 1.3 x 2.0 mm, 1:45 min. (A–D) Acquired with AIR™ Recon DL and (E) acquired with AIR™ Recon.
E
Figure 5.
(A, B) Axial 2D T1w dual echo FSPGR, 1.1 x 1.6 x 5.0 mm, 51 sec., (A) in phase and (B) out of phase; (C, D) axial post-contrast FSPGR FatSat, 1.4 x 1.4 x 5.0 mm, 51 sec.; and (E) axial free-breathing 3D LAVA Star, 1.3 x 1.3 x 2.0 mm, 1:45 min. (A–D) Acquired with AIR™ Recon DL and (E) acquired with AIR™ Recon.
1. Jiang HY, Chen J, Xia CC, Cao LK, Duan T, Song B. Noninvasive imaging of hepatocellular carcinoma: From diagnosis to prognosis. World J Gastroenterol. 2018 Jun 14;24(22):2348-2362.
1. Jiang HY, Chen J, Xia CC, Cao LK, Duan T, Song B. Noninvasive imaging of hepatocellular carcinoma: From diagnosis to prognosis. World J Gastroenterol. 2018 Jun 14;24(22):2348-2362.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
CASE STUDIES
Advanced 1.5T MR imaging for non-invasive diagnosis of hepatocellular carcinoma
Advanced 1.5T MR imaging for non-invasive diagnosis of hepatocellular carcinoma
by Ercüment Çiftçi, MD, Professor of Radiology, Özgür Çakır, MD, Associate Professor of Radiology, and Mesude Tosun, MD, Radiologist, Kocaeli University Hospital, Kocaeli, Turkey
MR plays a pivotal role in the non-invasive diagnosis of liver diseases, including hepatocellular carcinoma (HCC). In contrast-enhanced MR, enhancement patterns in arterial phase hyperenhancement and portal venous and/or delayed phase wash-out enable diagnosis without histopathologic confirmation.1 In addition, diffusion-weighted imaging (DWI), perfusion imaging and MR elastography (MRE) provide additional insight on a tumor’s biological behavior. The ability to capture tumor imaging characteristics, including nodule size, margin, number, vascular invasion and growth patterns, provides additional insight into the tumor microvascular invasion and patient prognosis.1
Although contrast-enhanced CT is also utilized, definitive non-invasive diagnosis of HCC in multi-detector CT still has diagnostic and dose challenges. MR imaging presents significant advantages for morphological and functional assessments. However, patient compliance, high SNR and the need for high spatial and temporal resolution are key for accurate MR imaging and follow-up studies.
Advances in MR technology have helped address the need for better, more confident diagnosis and treatment planning. These include:
- SnapShot SSFSE: a trusted T2-weighted acquisition technique for abdominal exams, this provides clear edge resolution and high CNR boosted with AIR™ Recon DL and free-breathing alternatives.
- DISCO: multi-arterial parenchymal and vascular assessment.
- HyperSense: improves capability for both temporal and spatial resolution for DISCO and uncompromised image quality.
- 3D Cube: free-breathing 3D acquisition allows for better pre-surgical planning and/or biopsy guidance.
- LAVA Star: free-breathing acquisition addressing high resolution expectations and better image results when the patient is not able to hold their breath.
Patient history
A 58-year-old male with high liver function test results was referred for a follow-up exam to evaluate a liver lesion. The patient had several previous MR exams at other centers with non-definitive diagnostic reports. This exam was requested as a last attempt to use MR for diagnosis before sending the patient to invasive diagnostic procedures.
Results
Lesion is at the level of segment 5-6 in the liver parenchyma, approximately 12 x 10 cm in size. Lesion is observed with a heterogeneous contrast enhancement pattern, containing fat component and capsular staining in the late phases.
Lesion considered as HCC in the foreground. A few similar lesions around the described lesion were approximately 1.5 cm in diameter.
Discussion
The overall quality of our exam guided the radiologist and clinician for a differential diagnosis of HCC. The abdominal MR imaging results are generally considered to be patient dependent based on compliance during the exam. When differential diagnosis is critical for patient follow-up and to manage treatment options, good image quality results facilitate the decision process for radiologists. In this case, excellent homogeneity in the wide bore (70 cm) SIGNA™ Voyager 1.5T system and contribution of the AIR™ Anterior Array (AA) Coil and AIR™ Recon DL provided the MR imaging results for this patient. High- resolution and high-SNR results along with motion-insensitive acquisition methods increased clarity of the lesion and surrounding tissues.
In particular, SnapShot SSFSE provided motion-free results, sharper edge resolution and great T2-weighted image contrast. AIR™ Recon DL, a pioneering, deep-learning-based reconstruction algorithm, improved SNR and image sharpness, enabling shorter scan times. DISCO delivered both high temporal and spatial resolution, allowing evaluation of multi-arterial assessment for 3D dynamic imaging, which is crucial for diagnosing HCC lesions with complex vascularization. High resolution also allows for detecting smaller lesions. HyperSense, a compressed sensing acceleration method, helps shorten scan times with no compromised image quality for a dynamic DISCO exam. The 3D T2 Cube FatSat provided high resolution through-plane assessment for guiding biopsy and procedures.
A
B
C
D
E
F
Figure 4.
Dynamic DISCO with HyperSense, AIR™ Recon and AIR™ AA Coil. (A) Pre-contrast, (B) arterial phase 1, (C) arterial phase 2, (D) arterial phase 3, (E) portal phase and (F) equilibrium, all acquired at 1.3 x 2.0 x 2.0 mm.
Figure 5.
(A, B) Axial 2D T1w dual echo FSPGR, 1.1 x 1.6 x 5.0 mm, 51 sec., (A) in phase and (B) out of phase; (C, D) axial post-contrast FSPGR FatSat, 1.4 x 1.4 x 5.0 mm, 51 sec.; and (E) axial free-breathing 3D LAVA Star, 1.3 x 1.3 x 2.0 mm, 1:45 min. (A–D) Acquired with AIR™ Recon DL and (E) acquired with AIR™ Recon.
After the installation of the SIGNA™ Voyager, the expectation for high image quality has increased for all imaging procedures. Additionally, some 3.0T preferred imaging procedures such as neuro and musculoskeletal were also shifted to the new SIGNA™ Voyager system. Installing SIGNA™Works AIR™ IQ Edition software with AIR™ Recon DL dramatically changed MR image quality expectations in the hospital, improved our workflow results and also changed productivity expectations in the radiology department.