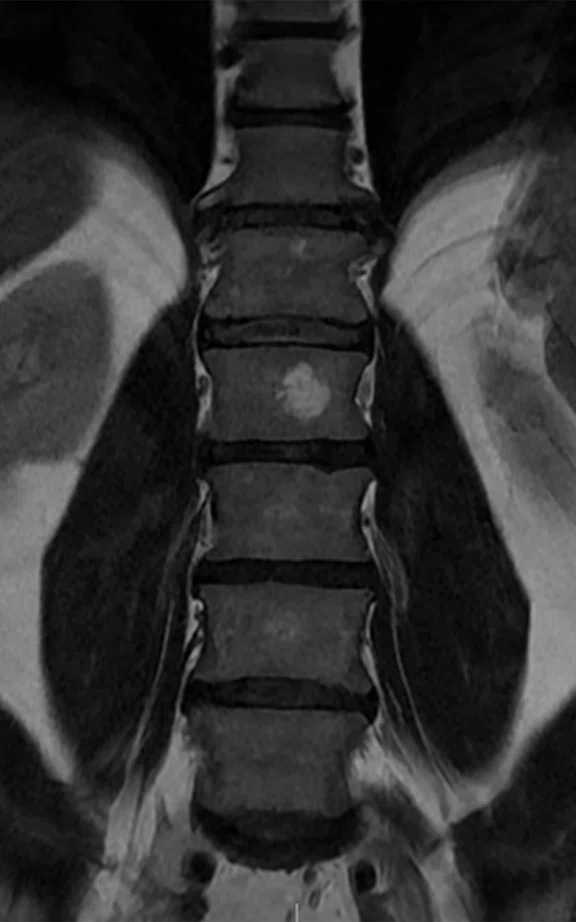
A
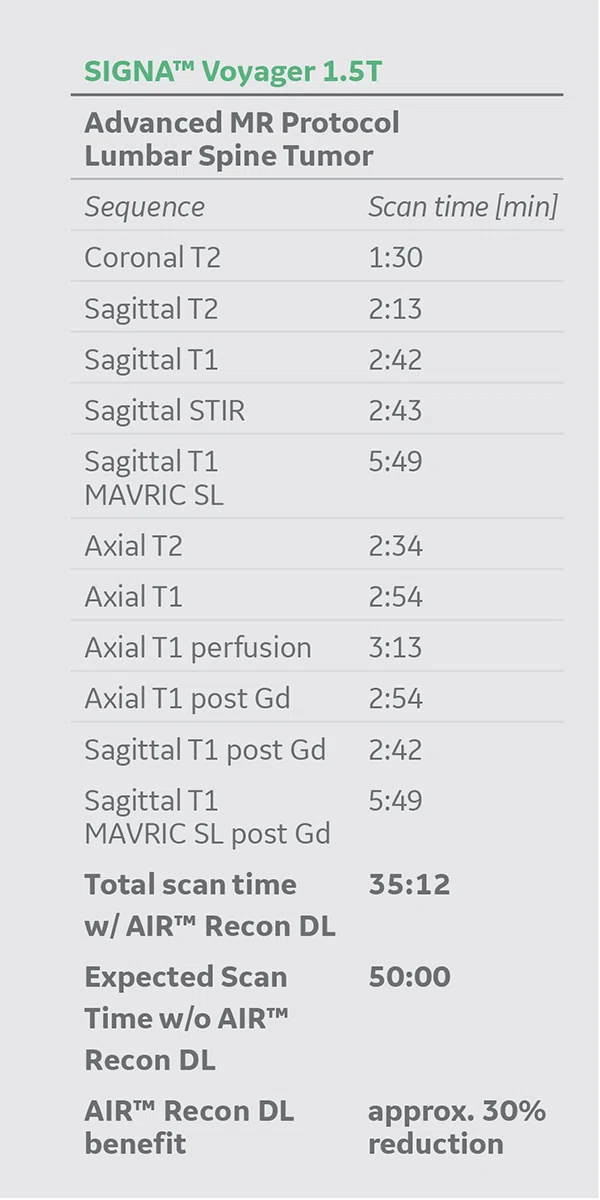
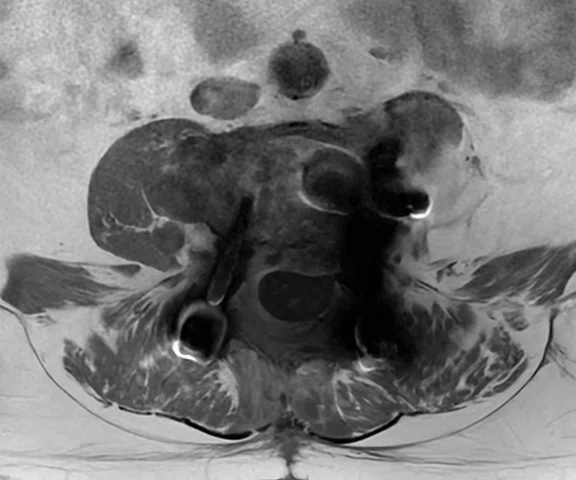
Figure 1.
Lumbar spine post-op protocol with AIR™ Recon DL includes (A) coronal T2, 0.7 x 1 x 5 mm, 1:30 min., (B) sagittal T2, 0.8 x 1 x 4, 2:13 min. and (C) sagittal STIR, 0.8 x 1.2 x 4 mm, 2:43 min.
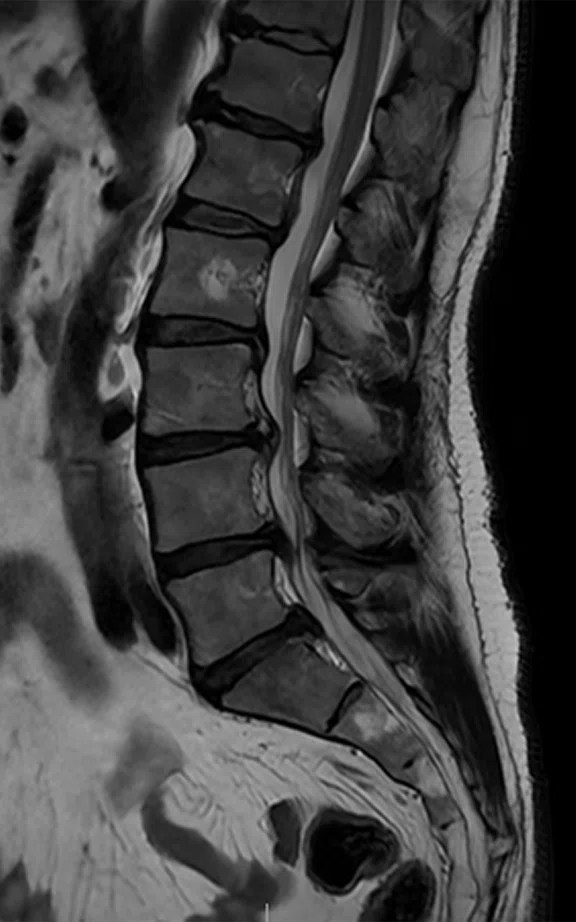
B
Figure 1.
Lumbar spine post-op protocol with AIR™ Recon DL includes (A) coronal T2, 0.7 x 1 x 5 mm, 1:30 min., (B) sagittal T2, 0.8 x 1 x 4, 2:13 min. and (C) sagittal STIR, 0.8 x 1.2 x 4 mm, 2:43 min.
C
Figure 1.
Lumbar spine post-op protocol with AIR™ Recon DL includes (A) coronal T2, 0.7 x 1 x 5 mm, 1:30 min., (B) sagittal T2, 0.8 x 1 x 4, 2:13 min. and (C) sagittal STIR, 0.8 x 1.2 x 4 mm, 2:43 min.
A
Figure 4.
Routine L-spine protocol total scan time was reduced by an average of 38% and spatial resolution was increased by an average of 16% after the AIR™ Recon DL installation. See table below. Total protocol scan time 8:06 min. (A) Coronal T2, 0.74 x 1.08 x 4 mm, 1:16 min.; (B) sagittal T2, 0.78 x 1.08 x 4 mm, 1:05 min.; (C) sagittal T1, 0.78 x 1.08 x 4 mm, 1:16 min.; (D) sagittal T2 FatSat, 0.78 x 1.17 x 4 mm, 1:58 min.; and (E) axial T2, 0.71 x 0.71 x 4 mm, 2:31 min.
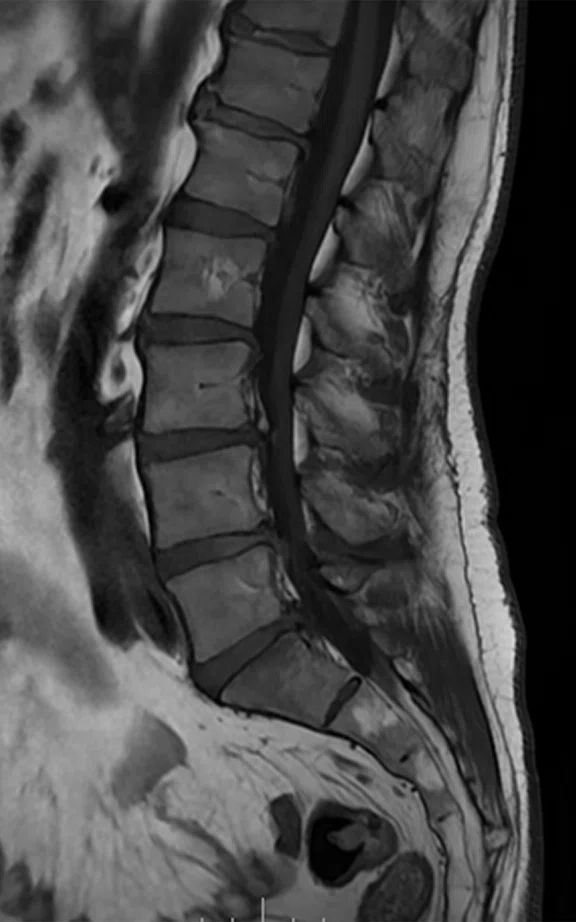
B
Figure 4.
Routine L-spine protocol total scan time was reduced by an average of 38% and spatial resolution was increased by an average of 16% after the AIR™ Recon DL installation. See table below. Total protocol scan time 8:06 min. (A) Coronal T2, 0.74 x 1.08 x 4 mm, 1:16 min.; (B) sagittal T2, 0.78 x 1.08 x 4 mm, 1:05 min.; (C) sagittal T1, 0.78 x 1.08 x 4 mm, 1:16 min.; (D) sagittal T2 FatSat, 0.78 x 1.17 x 4 mm, 1:58 min.; and (E) axial T2, 0.71 x 0.71 x 4 mm, 2:31 min.
C
Figure 4.
Routine L-spine protocol total scan time was reduced by an average of 38% and spatial resolution was increased by an average of 16% after the AIR™ Recon DL installation. See table below. Total protocol scan time 8:06 min. (A) Coronal T2, 0.74 x 1.08 x 4 mm, 1:16 min.; (B) sagittal T2, 0.78 x 1.08 x 4 mm, 1:05 min.; (C) sagittal T1, 0.78 x 1.08 x 4 mm, 1:16 min.; (D) sagittal T2 FatSat, 0.78 x 1.17 x 4 mm, 1:58 min.; and (E) axial T2, 0.71 x 0.71 x 4 mm, 2:31 min.
D
Figure 4.
Routine L-spine protocol total scan time was reduced by an average of 38% and spatial resolution was increased by an average of 16% after the AIR™ Recon DL installation. See table below. Total protocol scan time 8:06 min. (A) Coronal T2, 0.74 x 1.08 x 4 mm, 1:16 min.; (B) sagittal T2, 0.78 x 1.08 x 4 mm, 1:05 min.; (C) sagittal T1, 0.78 x 1.08 x 4 mm, 1:16 min.; (D) sagittal T2 FatSat, 0.78 x 1.17 x 4 mm, 1:58 min.; and (E) axial T2, 0.71 x 0.71 x 4 mm, 2:31 min.
E
Figure 4.
Routine L-spine protocol total scan time was reduced by an average of 38% and spatial resolution was increased by an average of 16% after the AIR™ Recon DL installation. See table below. Total protocol scan time 8:06 min. (A) Coronal T2, 0.74 x 1.08 x 4 mm, 1:16 min.; (B) sagittal T2, 0.78 x 1.08 x 4 mm, 1:05 min.; (C) sagittal T1, 0.78 x 1.08 x 4 mm, 1:16 min.; (D) sagittal T2 FatSat, 0.78 x 1.17 x 4 mm, 1:58 min.; and (E) axial T2, 0.71 x 0.71 x 4 mm, 2:31 min.
1. Physiopedia. Chondrosarcoma. Available at: https://www.physio-pedia.com/Chondrosarcoma#cite_note-p3-3.
2. Lebel, RM. Performance characterization of a novel deep learning-based MR image reconstruction pipeline. August 2020. Available at: http://arxiv.org/abs/2008.06559.
3. Peters RD, Harris H, Lawson S. The clinical benefits of AIR™ Recon DL for MR image reconstruction. Available at: https://www.gehealthcare.com.sg/-/jssmedia/files/m/mr_gbl_air_recon_dl_091720_jb00297xx.pdf?rev=-1.
A
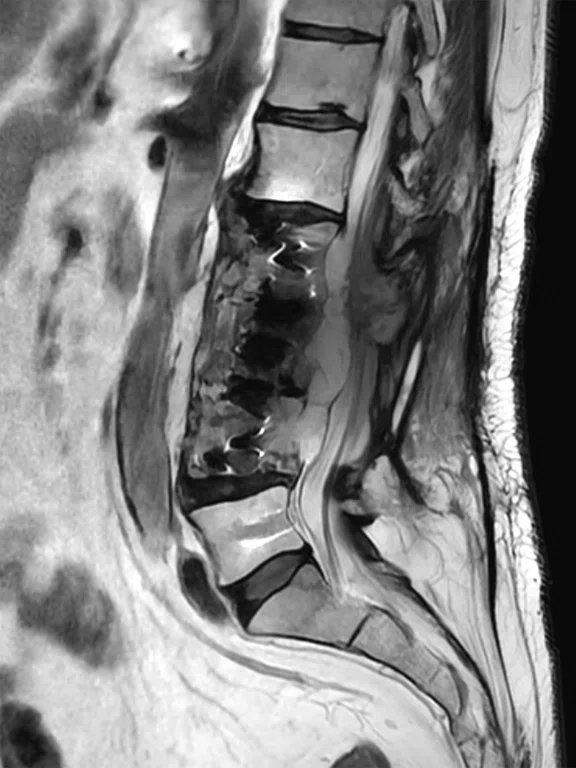
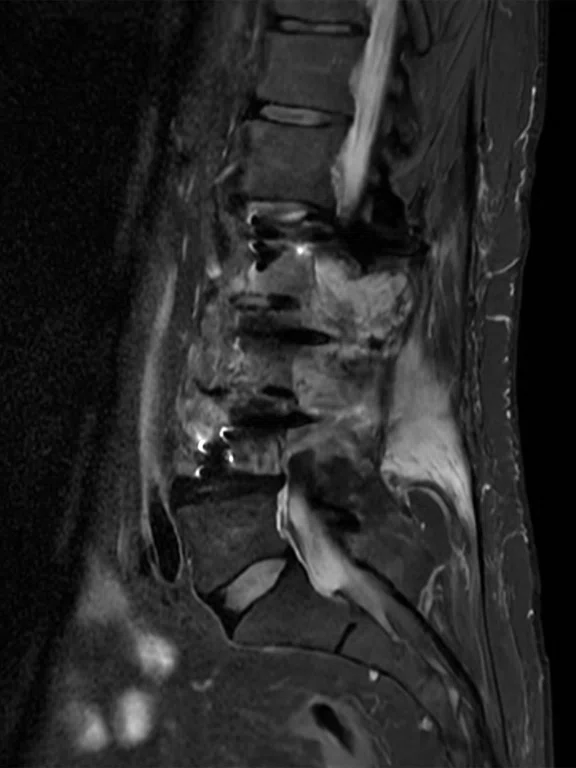
Figure 2.
Lumbar spine post-op protocol with AIR™ Recon DL includes (A) sagittal T1 post-contrast, 0.8 x 1 x 4 mm, 2:42 min, (B) axial T1 post-contrast 0.7 x 0.8 x 4 mm, 2:54 min. and (C) axial T2 post-contrast 0.7 x 0.7 x 4, 2:34 min.
B
Figure 2.
Lumbar spine post-op protocol with AIR™ Recon DL includes (A) sagittal T1 post-contrast, 0.8 x 1 x 4 mm, 2:42 min, (B) axial T1 post-contrast 0.7 x 0.8 x 4 mm, 2:54 min. and (C) axial T2 post-contrast 0.7 x 0.7 x 4, 2:34 min.
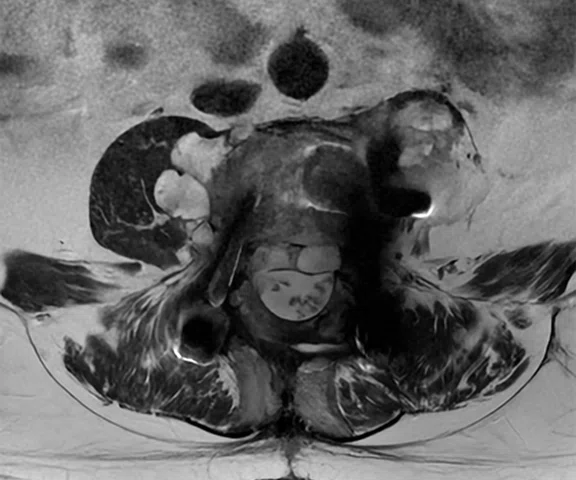
C
Figure 2.
Lumbar spine post-op protocol with AIR™ Recon DL includes (A) sagittal T1 post-contrast, 0.8 x 1 x 4 mm, 2:42 min, (B) axial T1 post-contrast 0.7 x 0.8 x 4 mm, 2:54 min. and (C) axial T2 post-contrast 0.7 x 0.7 x 4, 2:34 min.
A
Figure 3.
Exceptional post-processed subtraction images are obtained with SIGNA™ Voyager AIR™ IQ Edition, including (A) sagittal T1 MAVRIC subtraction, (B) 3D DISCO PEI and (C) 3D DISCO PEI/sagittal T1 subtraction with AIR™ Recon DL.
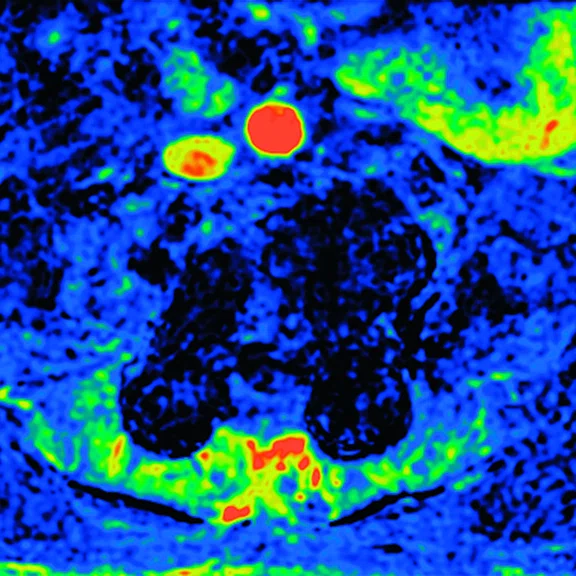
B
Figure 3.
Exceptional post-processed subtraction images are obtained with SIGNA™ Voyager AIR™ IQ Edition, including (A) sagittal T1 MAVRIC subtraction, (B) 3D DISCO PEI and (C) 3D DISCO PEI/sagittal T1 subtraction with AIR™ Recon DL.
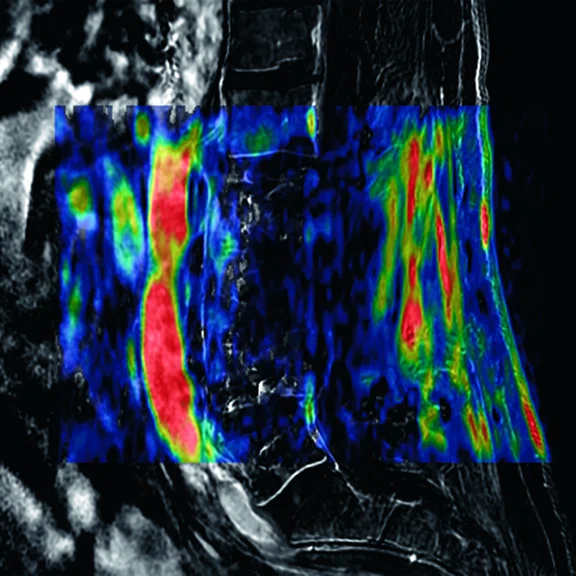
C
Figure 3.
Exceptional post-processed subtraction images are obtained with SIGNA™ Voyager AIR™ IQ Edition, including (A) sagittal T1 MAVRIC subtraction, (B) 3D DISCO PEI and (C) 3D DISCO PEI/sagittal T1 subtraction with AIR™ Recon DL.


result
PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
CASE STUDIES
Advanced spine tumor imaging with shorter scan times to increase patient comfort
Advanced spine tumor imaging with shorter scan times to increase patient comfort
Case submitted by CEDIRP, Ribeirão Preto, São Paulo, Brazil
Chondrosarcoma is a malignant cartilaginous bone tumor that accounts for approximately 25% of all primary malignant bone tumors.1 It is more common at long bones in the hip, shoulder and knee, and more rarely in the spine or ribs. It can sometimes occur in the soft tissue surrounding bones. Typically, chondrosarcomas grow slowly and may not cause many initial signs or symptoms, although some rare types grow rapidly and have a high risk of spreading to other areas of the body, making these tumors more diffcult to treat. The most common treatment for chondrosarcoma is surgery, and other complementary therapies may be utilized.
AIR™ Recon DL is a pioneering, deep-learning-based reconstruction algorithm that improves SNR and image sharpness, enabling shorter scan times. It improves image quality at the foundational level by making use of the raw data to remove image noise and ringing.2,3
In this case report, we will demonstrate the clinical benefits of AIR™ Recon DL in an advanced imaging protocol for the postoperative follow-up evaluation of a chondrosarcoma spine tumor with SIGNA™ Voyager 1.5T MR.
Patient history
A 60-year-old male with a post-op lumbar spine tumor diagnosed as a low-grade chondrosarcoma. Lumbar spine arthrodesis was done to stabilize the spine. Patient evolved with pain and weakness of the lower limbs. Imaging showed the lesion size increased into the spinal canal. A follow-up CT-guided biopsy was performed, however, the collected fragments were not able to determine tumor histology for the recurrent tumor.
An MR study was suggested to pinpoint a viable site for a new biopsy study.
Results
The image findings enabled the physician to monitor the lesion size and extension through MR imaging and help guide patient management, e.g., continued imaging follow-up, another image-guided biopsy or new surgery. Although the patient suffered from pain and discomfort due to the spinal lesion, he found the exam to be bearable due to the shortened scan time.
Figure 4.
Routine L-spine protocol total scan time was reduced by an average of 38% and spatial resolution was increased by an average of 16% after the AIR™ Recon DL installation. See table below. Total protocol scan time 8:06 min. (A) Coronal T2, 0.74 x 1.08 x 4 mm, 1:16 min.; (B) sagittal T2, 0.78 x 1.08 x 4 mm, 1:05 min.; (C) sagittal T1, 0.78 x 1.08 x 4 mm, 1:16 min.; (D) sagittal T2 FatSat, 0.78 x 1.17 x 4 mm, 1:58 min.; and (E) axial T2, 0.71 x 0.71 x 4 mm, 2:31 min.
Discussion
For a complete examination and diagnosis of complex spine tumors, such as chondrosarcoma, an advanced MR acquisition protocol needs to be implemented; however, this increases the overall scan time. In this patient case, AIR™ Recon DL reduced the routine lumbar spine MR protocol by approximately 38% and increased spatial resolution by 16%. The shorter scan time enabled the addition of advanced imaging techniques, such as MAVRIC T1 and DISCO T1 perfusion, for a complete examination and diagnosis of complex chondrosarcoma in a total scan time of just over 35 minutes, well below the allotted examination time slot of 50 minutes. At the same time, image quality was improved.
AIR™ Recon DL enables the practical, clinical use of higher bandwidth/pixel, which normally reduces SNR with conventional reconstruction, to reduce susceptibility effects and improve spatial resolution.
MAVRIC SL is an acquisition and reconstruction technique for imaging soft tissue and bone near MR-Conditional metallic devices. MAVRIC SL helps reduce artifacts caused by presence of metal in both in-plane and through-plane dimensions compared to conventional MR techniques. This greatly reduced susceptibility effects with the use of contrast media.
DISCO T1 perfusion was helpful to produce wash-in and wash-out maps utilizing ReadyView capabilities. Perfusion imaging did not show any areas with a high contrast media uptake rate, suggesting the tumor is slow growing. Sagittal T1 and MAVRIC SL T1 subtracted images were compared and were in accordance with perfusion maps and contrast media uptake in regions of interest.
According to Dr. Gustavo Novelino Simão, all images obtained were very high image quality. Despite the presence of metallic components in the spine, all images were adequate for diagnostic interpretation.
Acknowledgement
CEDIRP is grateful for the assistance and collaboration of Tiago Giacometti, Clinical Marketing Leader, GE Healthcare, Brazil, in preparing this patient case report.