A
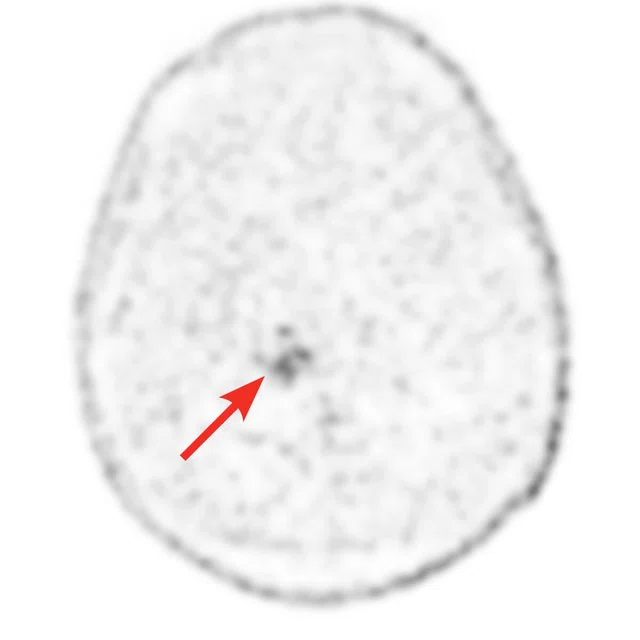
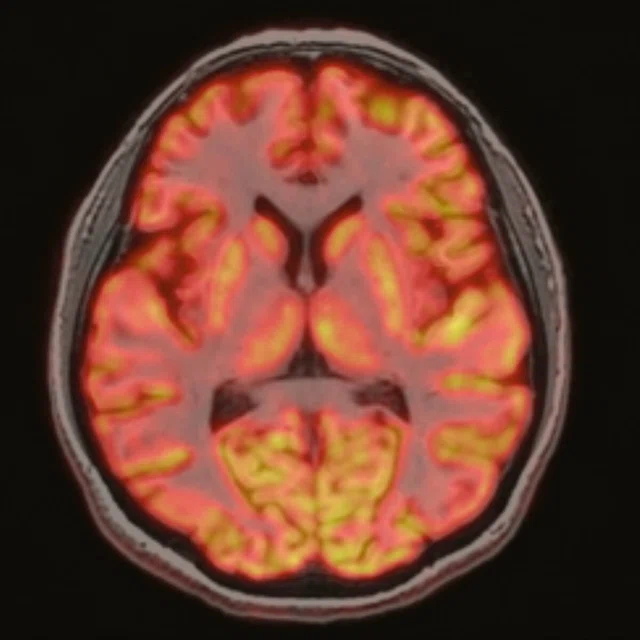
Figure 1.
A 35-year-old male patient with glioblastoma in the right frontal and parietal lobes. On follow-up exam post-surgery, a suspected lesion was observed posterior to right thalamus. The PET exam shown here is positive for recurrence. (A) 18F-FLT PET‡; (B) T2 FLAIR: (C) T1 3D BRAVO; (D) 18F-FDG PET; (E) T2 FLAIR; (F) T1 3D BRAVO.
‡ 18F-FLT PET is not cleared or approved by the US FDA or any other global regulator.
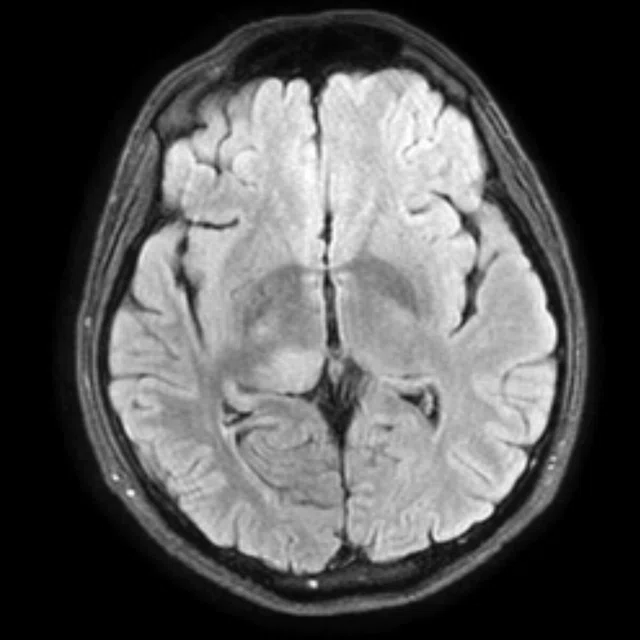
B
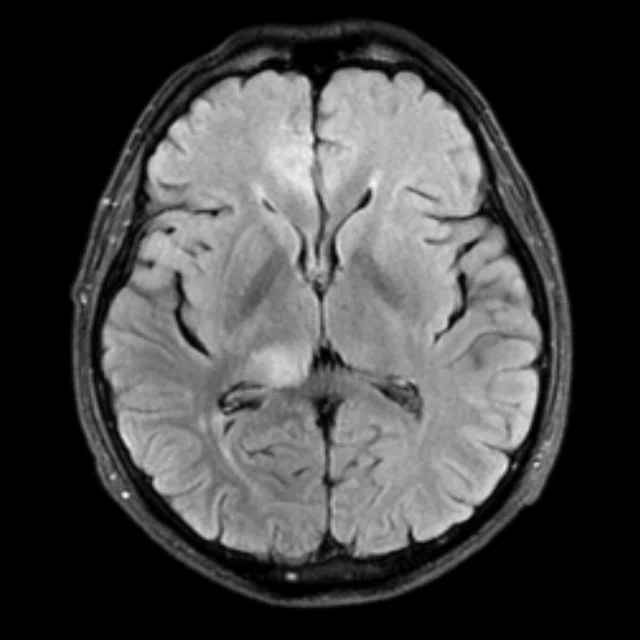
Figure 1.
A 35-year-old male patient with glioblastoma in the right frontal and parietal lobes. On follow-up exam post-surgery, a suspected lesion was observed posterior to right thalamus. The PET exam shown here is positive for recurrence. (A) 18F-FLT PET‡; (B) T2 FLAIR: (C) T1 3D BRAVO; (D) 18F-FDG PET; (E) T2 FLAIR; (F) T1 3D BRAVO.
‡ 18F-FLT PET is not cleared or approved by the US FDA or any other global regulator.
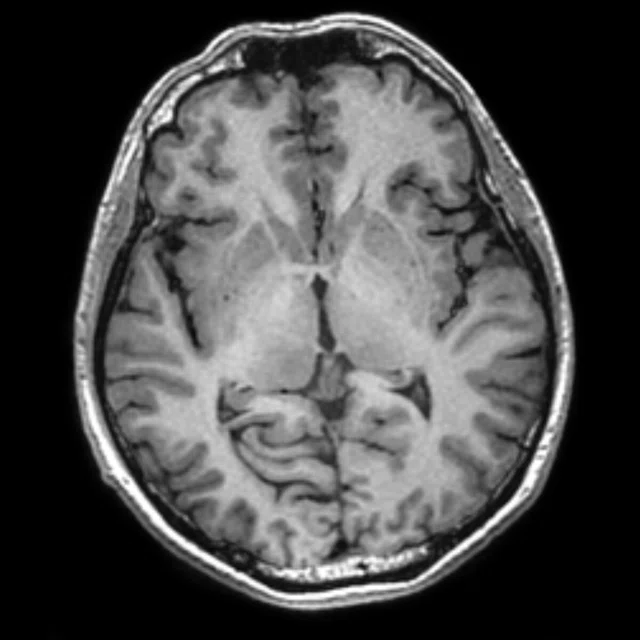
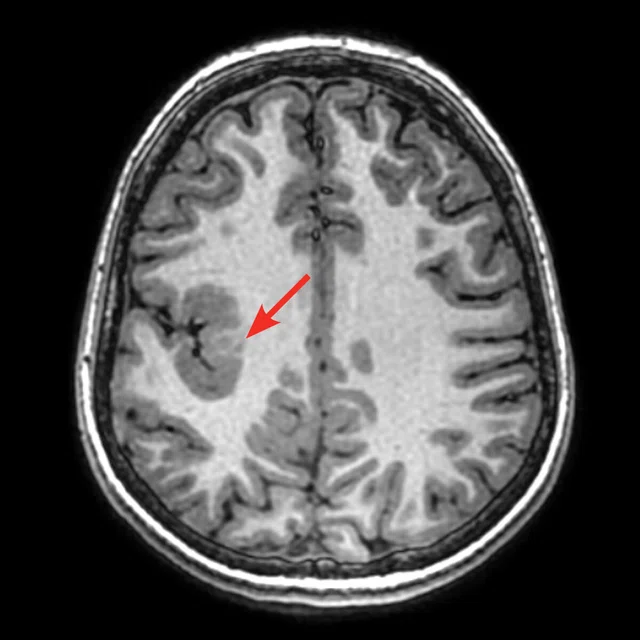
C
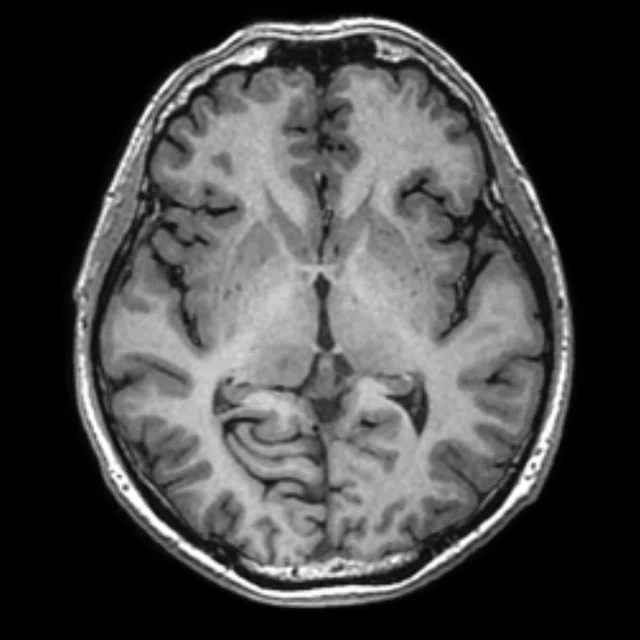
Figure 1.
A 35-year-old male patient with glioblastoma in the right frontal and parietal lobes. On follow-up exam post-surgery, a suspected lesion was observed posterior to right thalamus. The PET exam shown here is positive for recurrence. (A) 18F-FLT PET‡; (B) T2 FLAIR: (C) T1 3D BRAVO; (D) 18F-FDG PET; (E) T2 FLAIR; (F) T1 3D BRAVO.
‡ 18F-FLT PET is not cleared or approved by the US FDA or any other global regulator.
D
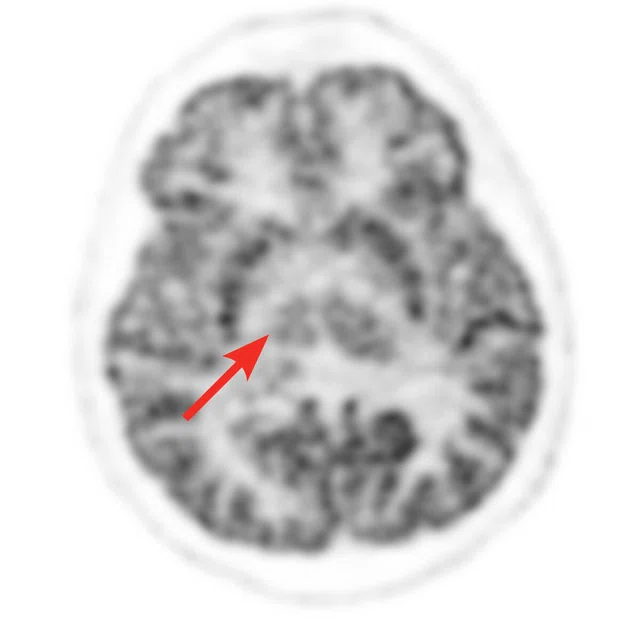
Figure 1.
A 35-year-old male patient with glioblastoma in the right frontal and parietal lobes. On follow-up exam post-surgery, a suspected lesion was observed posterior to right thalamus. The PET exam shown here is positive for recurrence. (A) 18F-FLT PET‡; (B) T2 FLAIR: (C) T1 3D BRAVO; (D) 18F-FDG PET; (E) T2 FLAIR; (F) T1 3D BRAVO.
‡ 18F-FLT PET is not cleared or approved by the US FDA or any other global regulator.
E
Figure 1.
A 35-year-old male patient with glioblastoma in the right frontal and parietal lobes. On follow-up exam post-surgery, a suspected lesion was observed posterior to right thalamus. The PET exam shown here is positive for recurrence. (A) 18F-FLT PET‡; (B) T2 FLAIR: (C) T1 3D BRAVO; (D) 18F-FDG PET; (E) T2 FLAIR; (F) T1 3D BRAVO.
‡ 18F-FLT PET is not cleared or approved by the US FDA or any other global regulator.
F
Figure 1.
A 35-year-old male patient with glioblastoma in the right frontal and parietal lobes. On follow-up exam post-surgery, a suspected lesion was observed posterior to right thalamus. The PET exam shown here is positive for recurrence. (A) 18F-FLT PET‡; (B) T2 FLAIR: (C) T1 3D BRAVO; (D) 18F-FDG PET; (E) T2 FLAIR; (F) T1 3D BRAVO.
‡ 18F-FLT PET is not cleared or approved by the US FDA or any other global regulator.
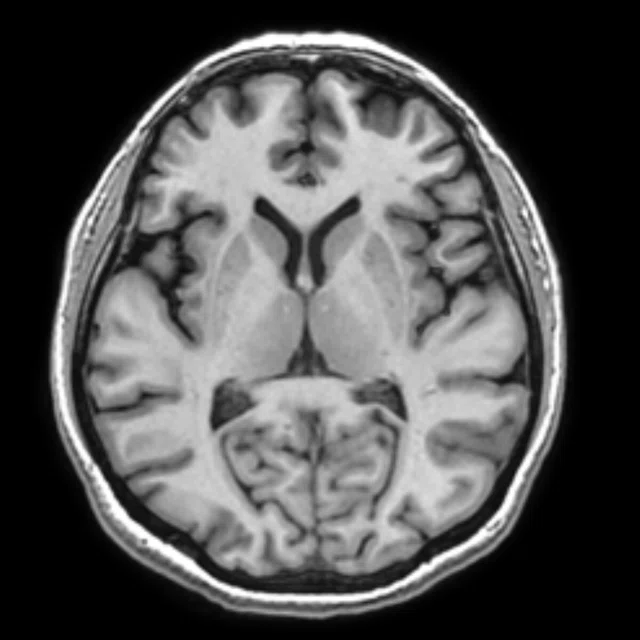
A
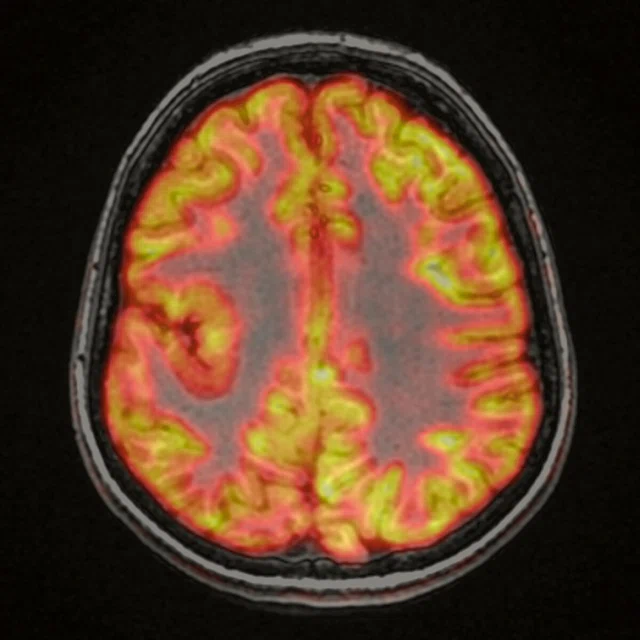
Figure 4.
A 16-year-old female patient with partial seizures. The epileptogenic region was on the right hemisphere according to EGG findings. The MR exam showed a lesion in the right perisylvian region compatible with cortical dysplasia. The lesion was mildly hypometabolic on FDG PET images. The addition of PET/MR has helped with pre-surgical planning and post-surgical success at the hospital. (A) 18F-FDG PET; (B) Fused PET/T1 3D BRAVO; (C) T1 3D BRAVO; (D) T2 FSE-IR.
B
Figure 4.
A 16-year-old female patient with partial seizures. The epileptogenic region was on the right hemisphere according to EGG findings. The MR exam showed a lesion in the right perisylvian region compatible with cortical dysplasia. The lesion was mildly hypometabolic on FDG PET images. The addition of PET/MR has helped with pre-surgical planning and post-surgical success at the hospital. (A) 18F-FDG PET; (B) Fused PET/T1 3D BRAVO; (C) T1 3D BRAVO; (D) T2 FSE-IR.
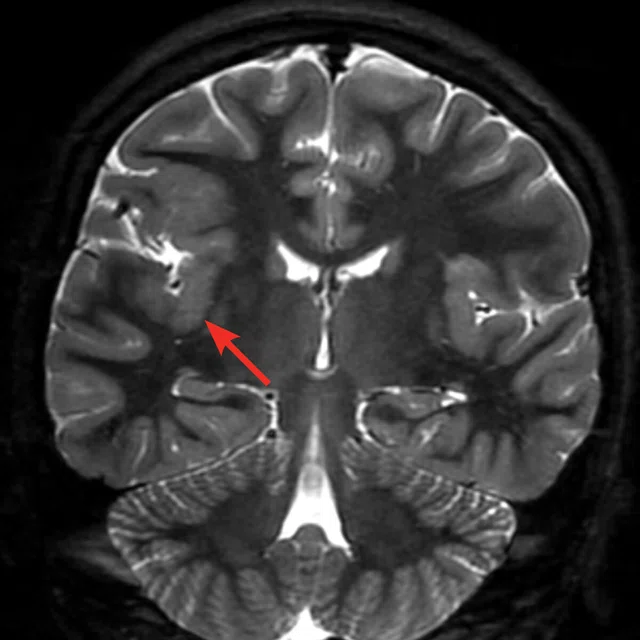
C
Figure 4.
A 16-year-old female patient with partial seizures. The epileptogenic region was on the right hemisphere according to EGG findings. The MR exam showed a lesion in the right perisylvian region compatible with cortical dysplasia. The lesion was mildly hypometabolic on FDG PET images. The addition of PET/MR has helped with pre-surgical planning and post-surgical success at the hospital. (A) 18F-FDG PET; (B) Fused PET/T1 3D BRAVO; (C) T1 3D BRAVO; (D) T2 FSE-IR.
D
Figure 4.
A 16-year-old female patient with partial seizures. The epileptogenic region was on the right hemisphere according to EGG findings. The MR exam showed a lesion in the right perisylvian region compatible with cortical dysplasia. The lesion was mildly hypometabolic on FDG PET images. The addition of PET/MR has helped with pre-surgical planning and post-surgical success at the hospital. (A) 18F-FDG PET; (B) Fused PET/T1 3D BRAVO; (C) T1 3D BRAVO; (D) T2 FSE-IR.
1 Uslu-Beşli L, Atay Kapucu LÖ, Karadeniz C, et al. Comparison of FDG PET/MRI and FDG PET/CT in Pediatric Oncology in Terms of Anatomic Correlation of FDG-positive Lesions. J Pediatr Hematol Oncol. 2019 Oct;41(7):542-550.
2 Hirfanoglu T, Serdaroglu A, Kurt G, et al. Outcomes of resective surgery in children and adolescents with focal lesional epilepsy: The experience of a tertiary epilepsy center. Epilepsy Behav. 2016 Oct;63:67-72.
A
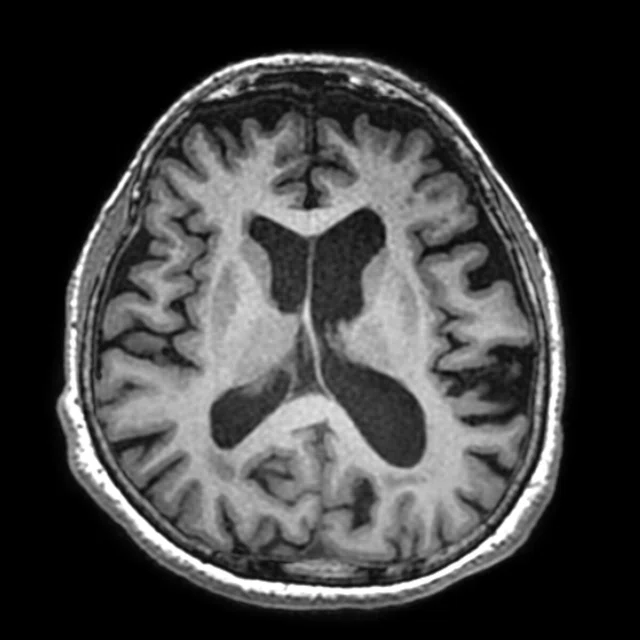
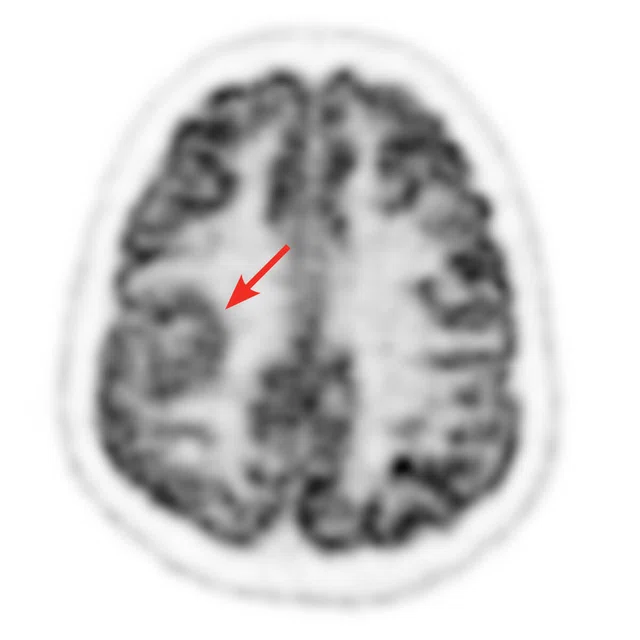
Figure 2.
A 70-year-old female patient with complaints of progressive speech difficulty (naming, repetition). Patient was not suffering memory problems. Neurological physical examination was normal. The clinical diagnosis was frontotemporal dementia. FDG PET exam showed left prominent bilateral frontal and left temporal hypometabolism. Accompanying MR showed cortical atrophy in these regions. PET/MR confirmed neurological exam findings that were compatible with frontotemporal dementia. (A) 18F-FDG PET; (B) T2 PROPELLER; (C) T1 3D BRAVO; (D) Fused PET/T1 3D BRAVO.
B
Figure 2.
A 70-year-old female patient with complaints of progressive speech difficulty (naming, repetition). Patient was not suffering memory problems. Neurological physical examination was normal. The clinical diagnosis was frontotemporal dementia. FDG PET exam showed left prominent bilateral frontal and left temporal hypometabolism. Accompanying MR showed cortical atrophy in these regions. PET/MR confirmed neurological exam findings that were compatible with frontotemporal dementia. (A) 18F-FDG PET; (B) T2 PROPELLER; (C) T1 3D BRAVO; (D) Fused PET/T1 3D BRAVO.
C
Figure 2.
A 70-year-old female patient with complaints of progressive speech difficulty (naming, repetition). Patient was not suffering memory problems. Neurological physical examination was normal. The clinical diagnosis was frontotemporal dementia. FDG PET exam showed left prominent bilateral frontal and left temporal hypometabolism. Accompanying MR showed cortical atrophy in these regions. PET/MR confirmed neurological exam findings that were compatible with frontotemporal dementia. (A) 18F-FDG PET; (B) T2 PROPELLER; (C) T1 3D BRAVO; (D) Fused PET/T1 3D BRAVO.
D
Figure 2.
A 70-year-old female patient with complaints of progressive speech difficulty (naming, repetition). Patient was not suffering memory problems. Neurological physical examination was normal. The clinical diagnosis was frontotemporal dementia. FDG PET exam showed left prominent bilateral frontal and left temporal hypometabolism. Accompanying MR showed cortical atrophy in these regions. PET/MR confirmed neurological exam findings that were compatible with frontotemporal dementia. (A) 18F-FDG PET; (B) T2 PROPELLER; (C) T1 3D BRAVO; (D) Fused PET/T1 3D BRAVO.
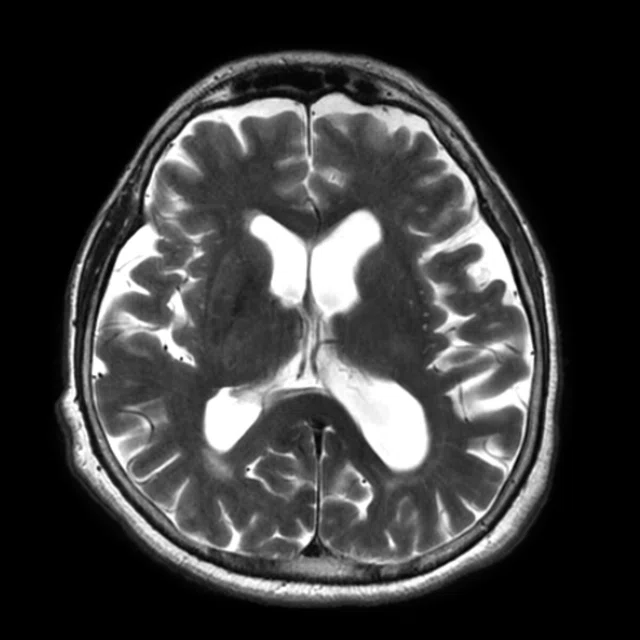
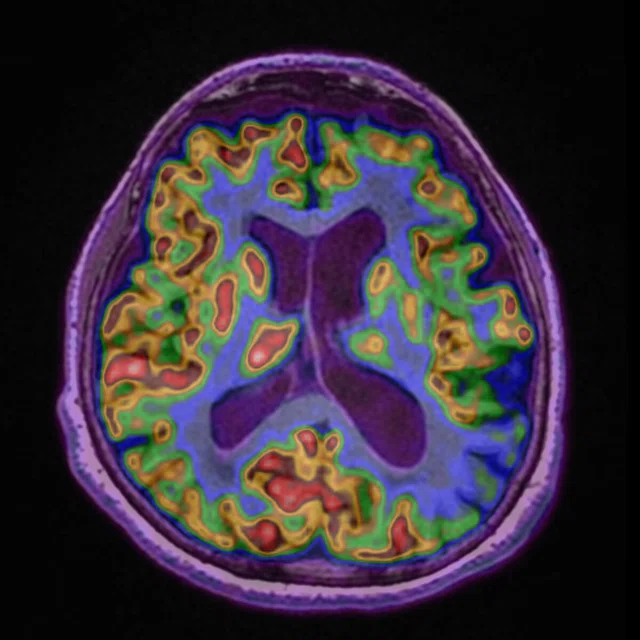
A
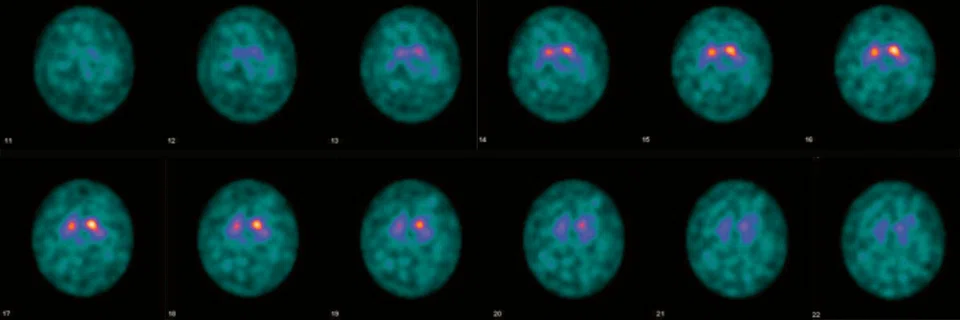
Figure 3.
A 57-year-old female patient with parkinsonism. The suspected clinical diagnosis was multi-system atrophy or corticobasal ganglionic degeneration. The DATSCAN SPECT of the patient showed right dominant bilateral decrease, or uptake, in basal ganglia, indicating the presence of a neurodegenerative parkinsonism syndrome. FDG PET image showed right insular and perisylvian cortical, right basal ganglion and thalamic nucleus hypometabolism, which is compatible with corticobasal ganglionic degeneration. (A) 18F-FDG PET; (B) T1 3D BRAVO; (C) Fused PET/T1 3D BRAVO; (D) DATSCAN SPECT.
B
Figure 3.
A 57-year-old female patient with parkinsonism. The suspected clinical diagnosis was multi-system atrophy or corticobasal ganglionic degeneration. The DATSCAN SPECT of the patient showed right dominant bilateral decrease, or uptake, in basal ganglia, indicating the presence of a neurodegenerative parkinsonism syndrome. FDG PET image showed right insular and perisylvian cortical, right basal ganglion and thalamic nucleus hypometabolism, which is compatible with corticobasal ganglionic degeneration. (A) 18F-FDG PET; (B) T1 3D BRAVO; (C) Fused PET/T1 3D BRAVO; (D) DATSCAN SPECT.
C
Figure 3.
A 57-year-old female patient with parkinsonism. The suspected clinical diagnosis was multi-system atrophy or corticobasal ganglionic degeneration. The DATSCAN SPECT of the patient showed right dominant bilateral decrease, or uptake, in basal ganglia, indicating the presence of a neurodegenerative parkinsonism syndrome. FDG PET image showed right insular and perisylvian cortical, right basal ganglion and thalamic nucleus hypometabolism, which is compatible with corticobasal ganglionic degeneration. (A) 18F-FDG PET; (B) T1 3D BRAVO; (C) Fused PET/T1 3D BRAVO; (D) DATSCAN SPECT.
D
Figure 3.
A 57-year-old female patient with parkinsonism. The suspected clinical diagnosis was multi-system atrophy or corticobasal ganglionic degeneration. The DATSCAN SPECT of the patient showed right dominant bilateral decrease, or uptake, in basal ganglia, indicating the presence of a neurodegenerative parkinsonism syndrome. FDG PET image showed right insular and perisylvian cortical, right basal ganglion and thalamic nucleus hypometabolism, which is compatible with corticobasal ganglionic degeneration. (A) 18F-FDG PET; (B) T1 3D BRAVO; (C) Fused PET/T1 3D BRAVO; (D) DATSCAN SPECT.
2 Hirfanoglu T, Serdaroglu A, Kurt G, et al. Outcomes of resective surgery in children and adolescents with focal lesional epilepsy: The experience of a tertiary epilepsy center. Epilepsy Behav. 2016 Oct;63:67-72.
3 Capraz IY, Kurt G, Akdemir Ö, et al. Surgical outcome in patients with MRI-negative, PET-positive temporal lobe epilepsy. Seizure. 2015 Jul;29:63-8.
4 Afshar-Oromieh A, Haberkorn U, Schlemmer HP, et al. Comparison of PET/CT and PET/MRI hybrid systems using a 68Ga labelled PSMA ligand for the diagnosis of recurrent prostate cancer: initial experience. Eur J Nucl Med Mol Imaging. 2014 May;41(5):887-97.
5 Domachevsky L, Bernstine H, Goldberg N, Nidam M, Catalano OA, Groshar D. Comparison between pelvic PSMA-PET/MR and whole-body PSMA-PET/CT for the initial evaluation of prostate cancer: a proof of concept study. Eur Radiol. 2019 Jul 22. doi: 10.1007/s00330-019-06353-y. [Epub ahead of print]
‡‡ 68Ga PSMA, 68Ga-labeled PSMA and 68Ga-labeled DOTATATE are not cleared or approved by the US FDA and may not be available for clinical use in all markets.
‡‡ 68Ga PSMA, 68Ga-labeled PSMA and 68Ga-labeled DOTATATE are not cleared or approved by the US FDA and may not be available for clinical use in all markets.
‡‡ 68Ga PSMA, 68Ga-labeled PSMA and 68Ga-labeled DOTATATE are not cleared or approved by the US FDA and may not be available for clinical use in all markets.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
IN PRACTICE
Advancing clinical neuroimaging with PET/MR
Advancing clinical neuroimaging with PET/MR
At Gazi University Faculty of Medicine, Application and Research Hospital (Ankara, Turkey), Professor Lütfiye Özlem Atay, MD, Head of the Nuclear Medicine Department, is providing the latest advancements in multimodal imaging with SIGNA™ PET/MR. From oncology to neurodegenerative diseases to epilepsy, Professor Atay’s vision for bringing the technology of the future to her department is changing the way patients are diagnosed and managed with the expectation of better outcomes.
At Gazi University Faculty of Medicine, Application and Research Hospital (Ankara, Turkey), Professor Lütfiye Özlem Atay, MD, Head of the Nuclear Medicine Department, is providing the latest advancements in multimodal imaging with SIGNA™ PET/MR. From oncology to neurodegenerative diseases to epilepsy, Professor Atay’s vision for bringing the technology of the future to her department is changing the way patients are diagnosed and managed with the expectation of better outcomes.
Ten years after Gazi University Hospital opened in 1979, the Department of Nuclear Medicine was formed. In addition to being one of the country’s leading reference centers for nuclear medicine, the department is also an important education and research center. To date, the department has trained 24 nuclear medicine specialists and was accredited by the UEMS (European Association of Medical Specialists) in the field of nuclear medicine education.
Gazi University Faculty of Medicine’s Department of Nuclear Medicine implemented Turkey’s first PET/CT system in 2004, added a dual-head gamma camera in 2008 and acquired their first SIGNA™ PET/MR system in December 2015. This was the first SIGNA™ PET/MR system in the region and beyond — Turkey, Central Asia, Russia, the Middle East and Africa.
“PET/MR is a technology of the future,” says Professor Atay. “In cases where we cannot distinguish soft tissue on PET/CT images, we can distinguish these structures easily when we perform PET/MR on the same patient. The superior soft tissues contrast of PET/MR provides a significant advantage.”
With the importance of PET in patient diagnosis and follow-up, and academic studies in oncology and neurology demonstrated in the literature, Professor Atay was excited to explore both research and clinical use of this hybrid technology. It provides the latest technology in multimodal imaging by combining molecular information and simultaneous multiparametric MR information.
She saw an opportunity to build upon the experience of scanning 40,000 PET/CT patients performed since 2004 at Gazi University Hospital and explore the value of PET/MR in following patients with chronic health disorders and diseases. In addition, the technology could help her further position the hospital as a leading brain research and reference center in the region.
Gazi University Hospital is also a center of excellence in pediatric oncology imaging. The value of the SIGNA™ PET/MR is especially relevant for this patient cohort, as it can reduce total patient ionizing radiation dose.
“Currently, PET/MR is the most important diagnostic imaging method for us in pediatric oncology patients, especially in patients requiring longterm follow-up, such as lymphoma,” Professor Atay adds.
In a recently published study, Professor Atay and co-authors retrospectively evaluated the data of 34 pediatric patients with various oncologic diagnoses and demonstrated that PET/MR exhibits better performance than PET/CT in terms of anatomic correlation of FDG-avid lesions.1
“In most of the pediatric oncology cases in our center, pediatricians prefer PET/MR imaging to PET/CT for whole-body FDG PET examinations. This is due to the decrease in radiation dose and the detection of lesions with high soft tissue contrast,” Professor Atay says.
Implementing PET/MR
As the first center in Turkey to perform FDG PET/CT imaging, Gazi University Hospital’s nuclear medicine physicians had extensive experience in reading these studies. Prior to installing PET/MR, the team participated in PET/MR-related courses and visited sites that already had a system installed for training.
According to Professor Atay, GE Healthcare’s clinical applications team provided support and protocol development guidance. She is impressed by the level of expertise provided by the GE support teams and finds added value in the continued development of GE PET and MR technology.
In the first year, the department performed PET/CT and PET/MR sequentially on most patients. The nuclear medicine physicians participated in multi-disciplinary councils and international workshops, and support staff received additional training on the use and safety of PET/MR. Having technologists experienced in MR imaging was critical to the department’s successful launch of the PET/MR service.
“PET/MR technology is more complex compared to PET/CT. Therefore, its use requires additional training and experience,” Professor Atay says.
Currently, the department performs approximately eight PET/MR exams each nine-hour day, with a total of more than 4,450 PET/MR studies completed since the installation.
Neuro-oncology
At Gazi University Hospital, PET/MR is used to differentiate recurrence from radiation necrosis in primary brain tumor patients, as well as for diagnosis and staging in patients with primary central nervous system lymphoma or brain metastasis. Metastatic patients also receive a whole-body PET/MR in the same scanning session.
Radiation oncology and neurosurgery physicians use PET/MR images similarly to PET/CT for the purpose of treatment planning. Although conventional MR is used for routine follow-up of neurooncology patients, any patient with suspicious findings is referred to PET/MR (Figure 1).
Figure 1.
A 35-year-old male patient with glioblastoma in the right frontal and parietal lobes. On follow-up exam post-surgery, a suspected lesion was observed posterior to right thalamus. The PET exam shown here is positive for recurrence. (A) 18F-FLT PET‡; (B) T2 FLAIR: (C) T1 3D BRAVO; (D) 18F-FDG PET; (E) T2 FLAIR; (F) T1 3D BRAVO.
“We’ve obtained imaging results consistent with the clinical followup data of the patients and the high success of the post- surgical follow-up results has led clinicians to rely on the brain FDG PET/MR imaging,” says Professor Atay. “In one of our ongoing studies we showed that using quantitative analysis and data mining methods increased the diagnostic accuracy above 90 percent in lateralization of brain FDG PET examinations in temporal lobe epilepsy. This is especially true in the evaluation of cortical dysplasia, where brain FDG PET examinations significantly contribute to the detection of pathological findings in MR evaluations and, in some cases, it can offer complementary results. In other words, when PET findings are considered negative, MR findings may contribute to the detection of abnormal PET findings.”
Beyond neuroimaging
Professor Atay believes that PET/MR can have an important role in other areas beyond the brain, particularly in the liver, prostate and breast. In cases of indeterminate PET findings in the liver, the addition of MR benefits the clinician in assessing the presence of lesions.
Professor Atay says, “With an experience of more than 300 68Ga PSMA‡‡ PET/MR primary staging studies of prostate cancer, we have detected the primary intraprostatic lesions and metastatic lesions more precisely in combined PET/MR imaging with superior soft tissue contrast compared with PET/CT.” This observation is consistent with the results of previous studies.4,5
Currently, the department is performing whole-body and high-resolution regional PET/MR imaging using 68Ga-labeled PSMA‡‡ in prostate cancers and 68Ga-labeled DOTATATE‡‡ in neuroendocrine tumors. In the near future, the department will explore the use of novel radiopharmaceuticals beyond FDG in primary rectal and head and neck cancers.
“We are at the beginning of the road for exploring the value of PET/MR imaging and its impact in clinical practice,” Professor Atay says.
“With PET/MR, brain PET findings can be more easily correlated with suspicious lesions on MR compared to PET/CT,” Professor Atay explains. “Therefore, PET/MR images directly affect the patient's follow-up decision and treatment planning in patients with recurrence. PET/MR data is used to determine surgical margins and to plan radiotherapy.”
Neurodegenerative diseases
Since installing the SIGNA™ PET/MR, Gazi University Hospital has been performing FDG PET/MR exams for the differential diagnosis of neurodegenerative diseases such as Alzheimer's disease, frontotemporal dementia, idiopathic Parkinson's disease and atypical parkinsonism syndromes. In Parkinson’s patients, the department also performs dopamine transporter (DAT) imaging with SPECT.
With the incidence of dementia increasing across populations, Professor Atay believes that early diagnosis and treatment of neurodegenerative diseases will be among the most important issues facing modern medicine. It is also critical to differentiate the type of neurodegenerative disease in a patient as new treatments emerge that are specific to the different dementia-related diseases (Figure 2).
Figure 2.
A 70-year-old female patient with complaints of progressive speech difficulty (naming, repetition). Patient was not suffering memory problems. Neurological physical examination was normal. The clinical diagnosis was frontotemporal dementia. FDG PET exam showed left prominent bilateral frontal and left temporal hypometabolism. Accompanying MR showed cortical atrophy in these regions. PET/MR confirmed neurological exam findings that were compatible with frontotemporal dementia. (A) 18F-FDG PET; (B) T2 PROPELLER; (C) T1 3D BRAVO; (D) Fused PET/T1 3D BRAVO.
“In terms of neuroimaging, PET/MR technology will be the most important imaging modality of the future, especially with the introduction of new radiopharmaceuticals targeting pathological proteins, such as amyloid and tau.”
Professor Lütfiye Özlem Atay
Gazi University Hospital Department of Nuclear Medicine is involved in a prospective, multi-center study involving early Alzheimer's patients that will involve amyloid PET imaging for the first time in Turkey. The study aims to evaluate the association of vascular pathologies with amyloid deposition and clinical progression. With the integrated PET/MR system, Professor Atay believes that spatial normalization and quantification of PET data will be performed accurately and the MR imaging will add morphological information about the brain, which will contribute to the investigation of vascular pathologies.
Using brain FDG PET imaging, clinicians at Gazi University Hospital can accurately detect changes in cortical metabolism using an institutional normal brain FDG PET database and quantitative analysis methods. Brain FDG PET/MR provides additional diagnostic information, especially in the identification of disease-specific metabolic patterns, which contribute significantly to the clinician’s ability to make a differential diagnosis. The department is also planning to perform quantitative analysis in more detail by correcting the partial volume effects. In this respect, the use of the PET/MR system is an advantage, says Professor Atay (Figure 3).
Figure 3.
A 57-year-old female patient with parkinsonism. The suspected clinical diagnosis was multi-system atrophy or corticobasal ganglionic degeneration. The DATSCAN SPECT of the patient showed right dominant bilateral decrease, or uptake, in basal ganglia, indicating the presence of a neurodegenerative parkinsonism syndrome. FDG PET image showed right insular and perisylvian cortical, right basal ganglion and thalamic nucleus hypometabolism, which is compatible with corticobasal ganglionic degeneration. (A) 18F-FDG PET; (B) T1 3D BRAVO; (C) Fused PET/T1 3D BRAVO; (D) DATSCAN SPECT.
Over 1,000 brain FDG PET/MR studies have been performed at Gazi University Hospital. Approximately 200 patients with neurodegenerative diseases have been evaluated.
Epilepsy
As a reference center for epilepsy surgery, the Department of Nuclear Medicine has evaluated more than 2,000 epileptic patients.2,3 According to Professor Atay, clinicians in the epilepsy surgery council prefer PET/MR to PET/CT for brain FDG PET studies. Interictal brain FDG PET/MR is performed for each epileptic patient who requires surgery or other invasive intervention (Figure 4). The institution’s normal brain FDG PET database and quantitative analysis are used to evaluate the images.
Figure 4.
A 16-year-old female patient with partial seizures. The epileptogenic region was on the right hemisphere according to EGG findings. The MR exam showed a lesion in the right perisylvian region compatible with cortical dysplasia. The lesion was mildly hypometabolic on FDG PET images. The addition of PET/MR has helped with pre-surgical planning and post-surgical success at the hospital. (A) 18F-FDG PET; (B) Fused PET/T1 3D BRAVO; (C) T1 3D BRAVO; (D) T2 FSE-IR.