1. Siversson C, Nordstrom F, Nilsson T, et al. Technical Note: MRI only prostate radiotherapy planning using the statistical decomposition algorithm. Med Phys. 2015 Oct;42(10):6090-7.
2. Nyholm T, Svensson S, Andersson S, et al. MR and CT data with multi observer delineations of organs in the pelvic area –
References
1. Siversson C, Nordstrom F, Nilsson T, et al. Technical Note: MRI only prostate radiotherapy planning using the statistical decomposition algorithm. Med Phys. 2015 Oct;42(10):6090-7.
2. Nyholm T, Svensson S, Andersson S, et al. MR and CT data with multi observer delineations of organs in the pelvic area – part of the Gold Atlas project. Med Phys. 2018 Mar;45(3):1295-1300.
3. Persson E, Gustafsson C, Nordström F, et al.MROPERA – A Multi-center/multi-vendor validation of MRI-only prostate treatment planning using synthetic CT images. Int J Radiation Oncol Biol Phys 2017;99(3):692-700.
4. Koivula L, Kapanen M, Seppälä T, et al. Intensity-based dual model method for generation of synthetic CT images from standard T2-weighted MR images – Generalized technique for four different MR scanners. Radiother Oncol. 2017 Dec;125(3):411-419.
5. Gustafsson C, Korhonen J, Persson E, Gunnlaugsson A,
Nyholm T, Olsson LE. Registration free automatic identification of gold fiducial markers in MRI target delineation images for prostate radiotherapy. Med Phys. 2017;44(11):5563-5574.
6. Gustafsson C, Nordström F, Persson E, Brynolfsson J, Olsson LE. Assessment of dosimetric impact of system specific geometric distortion in an MRI only based radiotherapy
workflow for prostate. Phys Med Biol. 2017 Apr 21;62(8):2976-2989.
7. Palmér E, Persson E, Ambolt P, Gustafsson C, Gunnlaugsson A, Olsson LE. Cone beam CT for QA of synthetic CT in MRI only for prostate patients. J Appl Clin Med Phys. 2018 Sep 4. doi: 10.1002/acm2.12429. [Epub ahead of print]
8. Gustafsson C, Persson E, Gunnlaugsson A, Olsson LE. Using C-Arm X-ray images from marker insertion to confirm the gold fiducial marker identification in an MRI-only prostate radiotherapy workflow. J Appl Clin Med Phys. 2018 Nov;19(6):185-192, 2018.
9. Andreasen D, Van Leemput K, Edmund JM. A patch-based pseudo-CT approach for MRI-only radiotherapy in the pelvis. Med Phys 2016;43:4742.
References
1. Siversson C, Nordstrom F, Nilsson T, et al. Technical Note: MRI only prostate radiotherapy planning using the statistical decomposition algorithm. Med Phys. 2015 Oct;42(10):6090-7.
2. Nyholm T, Svensson S, Andersson S, et al. MR and CT data with multi observer delineations of organs in the pelvic area – part of the Gold Atlas project. Med Phys. 2018 Mar;45(3):1295-1300.
3. Persson E, Gustafsson C, Nordström F, et al.MROPERA – A Multi-center/multi-vendor validation of MRI-only prostate treatment planning using synthetic CT images. Int J Radiation Oncol Biol Phys 2017;99(3):692-700.
4. Koivula L, Kapanen M, Seppälä T, et al. Intensity-based dual model method for generation of synthetic CT images from standard T2-weighted MR images – Generalized technique for four different MR scanners. Radiother Oncol. 2017 Dec;125(3):411-419.
5. Gustafsson C, Korhonen J, Persson E, Gunnlaugsson A,
Nyholm T, Olsson LE. Registration free automatic identification of gold fiducial markers in MRI target delineation images for prostate radiotherapy. Med Phys. 2017;44(11):5563-5574.
6. Gustafsson C, Nordström F, Persson E, Brynolfsson J, Olsson LE. Assessment of dosimetric impact of system specific geometric distortion in an MRI only based radiotherapy
workflow for prostate. Phys Med Biol. 2017 Apr 21;62(8):2976-2989.
7. Palmér E, Persson E, Ambolt P, Gustafsson C, Gunnlaugsson A, Olsson LE. Cone beam CT for QA of synthetic CT in MRI only for prostate patients. J Appl Clin Med Phys. 2018 Sep 4. doi: 10.1002/acm2.12429. [Epub ahead of print]
8. Gustafsson C, Persson E, Gunnlaugsson A, Olsson LE. Using C-Arm X-ray images from marker insertion to confirm the gold fiducial marker identification in an MRI-only prostate radiotherapy workflow. J Appl Clin Med Phys. 2018 Nov;19(6):185-192, 2018.
9. Andreasen D, Van Leemput K, Edmund JM. A patch-based pseudo-CT approach for MRI-only radiotherapy in the pelvis. Med Phys 2016;43:4742.
References
1. Siversson C, Nordstrom F, Nilsson T, et al. Technical Note: MRI only prostate radiotherapy planning using the statistical decomposition algorithm. Med Phys. 2015 Oct;42(10):6090-7.
2. Nyholm T, Svensson S, Andersson S, et al. MR and CT data with multi observer delineations of organs in the pelvic area – part of the Gold Atlas project. Med Phys. 2018 Mar;45(3):1295-1300.
3. Persson E, Gustafsson C, Nordström F, et al.MROPERA – A Multi-center/multi-vendor validation of MRI-only prostate treatment planning using synthetic CT images. Int J Radiation Oncol Biol Phys 2017;99(3):692-700.
4. Koivula L, Kapanen M, Seppälä T, et al. Intensity-based dual model method for generation of synthetic CT images from standard T2-weighted MR images – Generalized technique for four different MR scanners. Radiother Oncol. 2017 Dec;125(3):411-419.
5. Gustafsson C, Korhonen J, Persson E, Gunnlaugsson A,
Nyholm T, Olsson LE. Registration free automatic identification of gold fiducial markers in MRI target delineation images for prostate radiotherapy. Med Phys. 2017;44(11):5563-5574.
6. Gustafsson C, Nordström F, Persson E, Brynolfsson J, Olsson LE. Assessment of dosimetric impact of system specific geometric distortion in an MRI only based radiotherapy
workflow for prostate. Phys Med Biol. 2017 Apr 21;62(8):2976-2989.
7. Palmér E, Persson E, Ambolt P, Gustafsson C, Gunnlaugsson A, Olsson LE. Cone beam CT for QA of synthetic CT in MRI only for prostate patients. J Appl Clin Med Phys. 2018 Sep 4. doi: 10.1002/acm2.12429. [Epub ahead of print]
8. Gustafsson C, Persson E, Gunnlaugsson A, Olsson LE. Using C-Arm X-ray images from marker insertion to confirm the gold fiducial marker identification in an MRI-only prostate radiotherapy workflow. J Appl Clin Med Phys. 2018 Nov;19(6):185-192, 2018.
9. Andreasen D, Van Leemput K, Edmund JM. A patch-based pseudo-CT approach for MRI-only radiotherapy in the pelvis. Med Phys 2016;43:4742.
3. Persson E, Gustafsson C, Nordström F, et al.MROPERA – A Multi-center/multi-vendor validation of MRI-only prostate treatment planning using synthetic CT images. Int J Radiation Oncol Biol Phys 2017;99(3):692-700.
References
1. Siversson C, Nordstrom F, Nilsson T, et al. Technical Note: MRI only prostate radiotherapy planning using the statistical decomposition algorithm. Med Phys. 2015 Oct;42(10):6090-7.
2. Nyholm T, Svensson S, Andersson S, et al. MR and CT data with multi observer delineations of organs in the pelvic area – part of the Gold Atlas project. Med Phys. 2018 Mar;45(3):1295-1300.
3. Persson E, Gustafsson C, Nordström F, et al.MROPERA – A Multi-center/multi-vendor validation of MRI-only prostate treatment planning using synthetic CT images. Int J Radiation Oncol Biol Phys 2017;99(3):692-700.
4. Koivula L, Kapanen M, Seppälä T, et al. Intensity-based dual model method for generation of synthetic CT images from standard T2-weighted MR images – Generalized technique for four different MR scanners. Radiother Oncol. 2017 Dec;125(3):411-419.
5. Gustafsson C, Korhonen J, Persson E, Gunnlaugsson A,
Nyholm T, Olsson LE. Registration free automatic identification of gold fiducial markers in MRI target delineation images for prostate radiotherapy. Med Phys. 2017;44(11):5563-5574.
6. Gustafsson C, Nordström F, Persson E, Brynolfsson J, Olsson LE. Assessment of dosimetric impact of system specific geometric distortion in an MRI only based radiotherapy
workflow for prostate. Phys Med Biol. 2017 Apr 21;62(8):2976-2989.
7. Palmér E, Persson E, Ambolt P, Gustafsson C, Gunnlaugsson A, Olsson LE. Cone beam CT for QA of synthetic CT in MRI only for prostate patients. J Appl Clin Med Phys. 2018 Sep 4. doi: 10.1002/acm2.12429. [Epub ahead of print]
8. Gustafsson C, Persson E, Gunnlaugsson A, Olsson LE. Using C-Arm X-ray images from marker insertion to confirm the gold fiducial marker identification in an MRI-only prostate radiotherapy workflow. J Appl Clin Med Phys. 2018 Nov;19(6):185-192, 2018.
9. Andreasen D, Van Leemput K, Edmund JM. A patch-based pseudo-CT approach for MRI-only radiotherapy in the pelvis. Med Phys 2016;43:4742.
7. Palmér E, Persson E, Ambolt P, Gustafsson C, Gunnlaugsson A, Olsson LE. Cone beam CT for QA of synthetic CT in MRI only for prostate patients. J Appl Clin Med Phys. 2018 Sep 4. doi: 10.1002/acm2.12429. [Epub ahead of print]
3. Persson E, Gustafsson C, Nordström F, et al.MROPERA – A Multi-center/multi-vendor validation of MRI-only prostate treatment planning using synthetic CT images. Int J Radiation Oncol Biol Phys 2017;99(3):692-700.
3. Persson E, Gustafsson C, Nordström F, et al.MROPERA – A Multi-center/multi-vendor validation of MRI-only prostate treatment planning using synthetic CT images. Int J Radiation Oncol Biol Phys 2017;99(3):692-700.
4. Koivula L, Kapanen M, Seppälä T, et al. Intensity-based dual model method for generation of synthetic CT images from standard T2-weighted MR images – Generalized technique for four diff erent MR scanners. Radiother Oncol. 2017 Dec;125(3):411-419.
8. Gustafsson C, Persson E, Gunnlaugsson A, Olsson LE. Using C-Arm X-ray images from marker insertion to confirm the gold fiducial marker identification in an MRI-only prostate radiotherapy workflow. J Appl Clin Med Phys. 2018 Nov;19(6):185-192, 2018.
6. Gustafsson C, Nordström F, Persson E, Brynolfsson J, Olsson LE. Assessment of dosimetric impact of system specific geometric distortion in an MRI only based radiotherapy workflow for prostate. Phys Med Biol. 2017 Apr 21;62(8):2976-2989.
7. Palmér E, Persson E, Ambolt P, Gustafsson C, Gunnlaugsson A, Olsson LE. Cone beam CT for QA of synthetic CT in MRI only for prostate patients. J Appl Clin Med Phys. 2018 Sep 4. doi: 10.1002/acm2.12429. [Epub ahead of print]
Figure 4.
Each patient is imaged in the treatment position with patient positioning devices. Image courtesy of Gentle Radiotherapy.
A
Figure 5.
T2-weighted images are predominantly used for target delineation in the prostate. (A-D) PROPELLER is used to compensate for motion. Images copyrighted by Christian Jamtheim Gustafsson, Lund University, reprinted with permission. Thesis: MRI-Only Radiotherapy of Prostate Cancer - Development and evaluation of methods to assess fiducial marker detection, geometric accuracy and dosimetric integrity ISBN: 978-91-7619-775-2.
B
Figure 5.
T2-weighted images are predominantly used for target delineation in the prostate. (A-D) PROPELLER is used to compensate for motion. Images copyrighted by Christian Jamtheim Gustafsson, Lund University, reprinted with permission. Thesis: MRI-Only Radiotherapy of Prostate Cancer - Development and evaluation of methods to assess fiducial marker detection, geometric accuracy and dosimetric integrity ISBN: 978-91-7619-775-2.
C
Figure 5.
T2-weighted images are predominantly used for target delineation in the prostate. (A-D) PROPELLER is used to compensate for motion. Images copyrighted by Christian Jamtheim Gustafsson, Lund University, reprinted with permission. Thesis: MRI-Only Radiotherapy of Prostate Cancer - Development and evaluation of methods to assess fiducial marker detection, geometric accuracy and dosimetric integrity ISBN: 978-91-7619-775-2.
D
Figure 5.
T2-weighted images are predominantly used for target delineation in the prostate. (A-D) PROPELLER is used to compensate for motion. Images copyrighted by Christian Jamtheim Gustafsson, Lund University, reprinted with permission. Thesis: MRI-Only Radiotherapy of Prostate Cancer - Development and evaluation of methods to assess fiducial marker detection, geometric accuracy and dosimetric integrity ISBN: 978-91-7619-775-2.
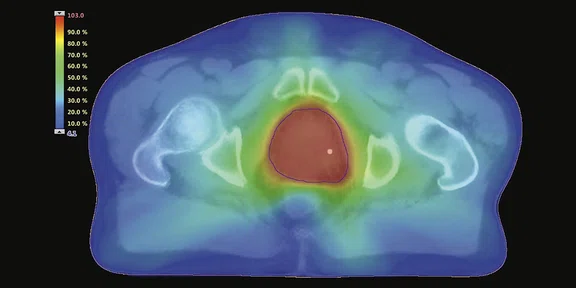
Figure 6.
MR images are used in the treatment planning system for target delineation and dose distributions. Image courtesy of Gentle Radiotherapy.
Figure 3.
Onboard kV X-ray images are used to verify the patient position. The fiducial markers seen in the kV images match very well to the markers seen in the digitally reconstructed radiograph generated from the sCT. If the patient does not have fiducial marker implants, bony structures can be used for position verification. Image courtesy of Gentle Radiotherapy.
3. Persson E, Gustafsson C, Nordström F, et al.MROPERA – A Multi-center/multi-vendor validation of MRI-only prostate treatment planning using synthetic CT images. Int J Radiation Oncol Biol Phys 2017;99(3):692-700.
9. Andreasen D, Van Leemput K, Edmund JM. A patch-based pseudo-CT approach for MRI-only radiotherapy in the pelvis. Med Phys 2016;43:4742.
5. Gustafsson C, Korhonen J, Persson E, Gunnlaugsson A, Nyholm T, Olsson LE. Registration free automatic identification of gold fiducial markers in MRI target delineation images for prostate radiotherapy. Med Phys. 2017;44(11):5563-5574.
6. Gustafsson C, Nordström F, Persson E, Brynolfsson J, Olsson LE. Assessment of dosimetric impact of system specific geometric distortion in an MRI only based radiotherapy workflow for prostate. Phys Med Biol. 2017 Apr 21;62(8):2976-2989.
5. Gustafsson C, Korhonen J, Persson E, Gunnlaugsson A, Nyholm T, Olsson LE. Registration free automatic identification of gold fiducial markers in MRI target delineation images for prostate radiotherapy. Med Phys. 2017;44(11):5563-5574.
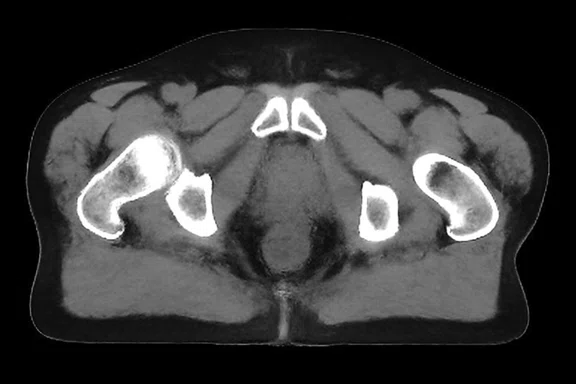
A
Figure 1.
Comparison of (A) CT and (B) sCT images. Images copyrighted by Christian Jamtheim Gustafsson, Lund University, reprinted with permission. Thesis: MRI-Only Radiotherapy of Prostate Cancer - Development and evaluation of methods to assess fiducial marker detection, geometric accuracy and dosimetric integrity ISBN: 978-91-7619-775-2.
B
Figure 1.
Comparison of (A) CT and (B) sCT images. Images copyrighted by Christian Jamtheim Gustafsson, Lund University, reprinted with permission. Thesis: MRI-Only Radiotherapy of Prostate Cancer - Development and evaluation of methods to assess fiducial marker detection, geometric accuracy and dosimetric integrity ISBN: 978-91-7619-775-2.
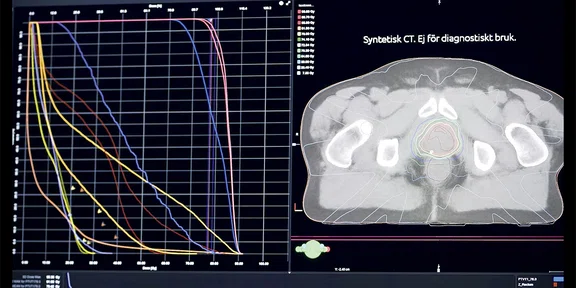
A
Figure 2.
(A) sCT is used for dose calculations in treatment planning system; (B) sCT with dose distributions. Images copyrighted by Christian Jamtheim Gustafsson, Lund University, reprinted with permission. Thesis: MRI-Only Radiotherapy of Prostate Cancer - Development and evaluation of methods to assess fiducial marker detection, geometric accuracy and dosimetric integrity ISBN: 978-91-7619-775-2.
B
Figure 2.
(A) sCT is used for dose calculations in treatment planning system; (B) sCT with dose distributions. Images copyrighted by Christian Jamtheim Gustafsson, Lund University, reprinted with permission. Thesis: MRI-Only Radiotherapy of Prostate Cancer - Development and evaluation of methods to assess fiducial marker detection, geometric accuracy and dosimetric integrity ISBN: 978-91-7619-775-2.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
Although the MR-OPERA study validated
the generation of sCT images for the male pelvis from T2-weighted images using MriPlanner, an independent QA evaluation of the sCT data was desired prior to the first treatment. Armed with published data that demonstrated the use of CBCT for patient-specific QA in brain radiotherapy9, the team explored the use of CBCT for QA of sCT data for prostate cancer patients and to verify the sCT data in regard to absorbed dose.
Not only was the CBCT system shown to be equivalent to CT in terms of HU, but dose calculations based on CT and sCT data sets had absorbed dose differences that were within clinically acceptable criteria. Further, errors introduced into the sCT data to test the QA capabilities were detected in the study.7
From bench to bedside
From the start, the motivation behind the research conducted by Skåne University Hospital has been to validate the use of MR imaging in radiation therapy and to rely only on MR imaging data in an effort to improve the accuracy of treatment delivery. This effort has been consolidated into a guide published by Gentle Radiotherapy.
Minna Lerner, MSc
Skåne University Hospital
Lund, Sweden
SPOTLIGHT
Development of an MR-only radiation therapy workflow
Development of an MR-only radiation therapy workflow
Skåne University Hospital developed a new workflow for MR-only radiation therapy treatments to improve accuracy of treatments and enable further increases in radiation dose to specific areas with more precision. The goal was to have an MR-only workflow that would avoid the introduction of image registration errors by using both MR and CT imaging. This work has been validated through numerous research studies conducted by Skåne University Hospital.
Skåne University Hospital developed a new workflow for MR-only radiation therapy treatments to improve accuracy of treatments and enable further increases in radiation dose to specific areas with more precision. The goal was to have an MR-only workflow that would avoid the introduction of image registration errors by using both MR and CT imaging. This work has been validated through numerous research studies conducted by Skåne University Hospital.
CT has historically been utilized as the primary imaging modality for tumor definition and dose calculation in radiation therapy treatment planning. However, MR provides better soft tissue contrast and resolution than CT and has been explored as an alternative for tumor definition and targeting.
Skåne University Hospital in Lund, Sweden, is a pioneer in the use of MR for radiation therapy planning. The radiation therapy department at Skåne University Hospital installed a Discovery™ MR750w, a 3.0T wide bore scanner, in 2013 to complement its two CT systems used for simulation. Eleven linear accelerators are used at Skåne University Hospital to treat between 6,000-7,000 cancer patients each year. Ten radiation oncologists, 22 radiation therapy physicists, one dedicated MR physicist and a large group of nurses, technologists and engineers staff the department.
By 2015, a team led by Lars E. Olsson, PhD, Professor of Medical Radiation Physics at Lund University and a physicist at Skåne University Hospital, and Adalsteinn Gunnlaugsson, MD, PhD, a Senior Consultant in the Department of Oncology at Skåne University Hospital, began researching the use of MR-only radiation therapy planning in prostate cancer patients.
“With MR, we are able to see the details of what we irradiate,” says Dr. Gunnlaugsson. “This will better allow us to increase the dose to the tumor and spare normal tissues.”
Even when using MR imaging to plan and direct cancer therapy, a CT examination is still acquired for dose calculations in the treatment planning system. However, the MR and CT need to be aligned as accurately as possible, since they are acquired on different systems and at different times.
Unfortunately, the alignment will not be perfect, which leads to additional safety margins around the target that results in a higher radiation dose to healthy, non-cancerous tissues.
“This is a major source of error when working with two different imaging datasets,” says Professor Olsson.
“By eliminating the CT, we can reduce and save resources. Since we don’t have to add the extra margin, we can actually reduce the dose to surrounding healthy tissue. This is the reason why we want to develop an MR-only workflow.”
Professor Lars E. Olsson
To implement an MR-only treatment planning workflow, the team together with Spectronic Medical AB (Helsingborg, Sweden) developed a method for generating Hounsfield Units (HU) maps from synthetic CT (sCT) images derived from the MR data. The Statistical Decomposition Algorithm (SDA) automatically generates sCT images from MR imaging data by using automatic tissue classifications and a model trained with multi-modal template materials. The team validated the accuracy of the SDA model against conventional CT Sim data and found it to be highly accurate.1
Figure 1.
Comparison of (A) CT and (B) sCT images. Images copyrighted by Christian Jamtheim Gustafsson, Lund University, reprinted with permission. Thesis: MRI-Only Radiotherapy of Prostate Cancer - Development and evaluation of methods to assess fiducial marker detection, geometric accuracy and dosimetric integrity ISBN: 978-91-7619-775-2.
As part of this effort and in collaboration with other Swedish academic hospitals, Skåne University Hospital participates in Gentle Radiotherapy, a national program funded by the Swedish Innovation Agency, VINNOVA, and associated hospitals. The long-term goal of Gentle Radiotherapy is to create a large-scale national world-class platform for cancer treatment, including the development of a fully integrated MR-only workflow for radiotherapy. The project has also published the Gold Atlas data, a complete dataset of the male pelvic region that is a source for training and validation of segmentation algorithms and methods to convert MR to sCT.2
Figure 2.
(A) sCT is used for dose calculations in treatment planning system; (B) sCT with dose distributions. Images copyrighted by Christian Jamtheim Gustafsson, Lund University, reprinted with permission. Thesis: MRI-Only Radiotherapy of Prostate Cancer - Development and evaluation of methods to assess fiducial marker detection, geometric accuracy and dosimetric integrity ISBN: 978-91-7619-775-2.
Results of a multi-center study validating MR-only prostate planning using synthetic CT images reported minimal differences between CT and sCT.3 The MR-Only Prostate External Radiotherapy (MR-OPERA) study found that an atlas-based sCT generation software, MriPlanner (Spectronic Medical), provided dosimetrically accurate data compared to CT Sim and delivered a robust workflow that required only minor changes in the clinical routine.3 The study included scanners from two different manufacturers at two field strengths. This important study, performed by PhD student Emilia Persson at Skåne University Hospital, was a significant step forward in the development of an MR-only workflow.
Another research study led by several leading hospitals in Finland with contributions from institutions in Australia, the Netherlands, Denmark and Skåne University Hospital also examined the use of an intensity-based method to generate sCT images from standard T2-weighted images of the pelvis. The authors found this method produced clinically acceptable dose calculation results across 35 prostate cancer patients.4 As with MR-OPERA, this study was conducted on different MR systems to demonstrate reliability across scanners and sequences.
“In many cases, our research is different when it comes to MR-only radiation therapy,” says Professor Olsson. “While many sites are developing different techniques, most will not treat the patient with MR-only imaging. When we started this initiative, our goal was to implement MR-only treatment in the clinic similarly to conventional, CT-based treatments.”
Figure 3.
Onboard kV X-ray images are used to verify the patient position. The fiducial markers seen in the kV images match very well to the markers seen in the digitally reconstructed radiograph generated from the sCT. If the patient does not have fiducial marker implants, bony structures can be used for position verification. Image courtesy of Gentle Radiotherapy.
A body of research
To accomplish the goal of MR-only guided radiation therapy planning, additional methods and tools were developed by the Skåne University Hospital team. This includes an automatic registration-free method for identifying implanted gold fiducial markers using multi-echo gradient echo imaging5, development and evaluation of a technique to quantify the dosimetric effects of MR system specific distortions for sCT images6 and a dose quality assurance procedure for sCT using the cone beam CT (CBCT) imaging device on the linear accelerator.7
In MR, T2-weighted spin echo images depict gold fiducial markers as a small signal void similar to calcifications and post-biopsy fibrosis. While the use of multi-echo gradient echo imaging was shown to be feasible and reliable for identifying gold fiducial markers5, the team also wanted to develop a quality assurance method for this process. The goal is to have an MR-only workflow that would not change the radiation therapy workflow and to avoid the introduction of image registration errors by using both MR and CT imaging. The team addressed this issue using the C-arm X-ray images that are acquired during implantation of the gold fiducial markers to confirm fiducial placement. Their study demonstrated that this approach was feasible and using the method as described in the paper would completely remove the need for CT imaging, as well as potentially provide an MRI-independent redundant method for gold fiducial marker verification.8
The issue of geometric accuracy was also a key concern with the use of MR-only radiation therapy and a potential obstacle to its use. So, it was a logical starting point to investigate whether distortions from a non-linear gradient in an MR system were a true problem or could be resolved.
“As shown in our paper, this is a very manageable issue,” explains Christian Jamtheim Gustafsson, MSc, a medical physicist at Skåne University Hospital. “By using 3D distortion correction and managing patient magnetic susceptibility differences by increasing the receiver bandwidth, we can address this. We’ve shown this in our papers, as well as in studies from other sites, that this really is not a problem.” Gustafsson is in the process of submitting his PhD thesis, and at the end of May he will be the first student in the group to get his PhD exam from the results of this project.
The acquisition of a large field-of-view (FOV) to cover the entire pelvic region for sCT generation could lead to geometric distortions, since the non-linear gradient effect enhances as the radius from the isocenter increases. However, when 3D distortion correction and high acquisition bandwidths were used for images with large FOVs, no clinically relevant dose difference or structure deformation was detected.6
“Our initial investigation in the use of MR-only for brain cancers demonstrates the same answer, that all distortion sources are very manageable.”
Christian Jamtheim Gustafsson
Figure 4.
Each patient is imaged in the treatment position with patient positioning devices. Image courtesy of Gentle Radiotherapy.
Although the MR-OPERA study validated the generation of sCT images for the male pelvis from T2-weighted images using MriPlanner, an independent QA evaluation of the sCT data was desired prior to the first treatment. Armed with published data that demonstrated the use of CBCT for patient-specific QA in brain radiotherapy9, the team explored the use of CBCT for QA of sCT data for prostate cancer patients and to verify the sCT data in regard to absorbed dose.
Not only was the CBCT system shown to be equivalent to CT in terms of HU, but dose calculations based on CT and sCT data sets had absorbed dose differences that were within clinically acceptable criteria. Further, errors introduced into the sCT data to test the QA capabilities were detected in the study.7
From bench to bedside
From the start, the motivation behind the research conducted by Skåne University Hospital has been to validate the use of MR imaging in radiation therapy and to rely only on MR imaging data in an effort to improve the accuracy of treatment delivery. This effort has been consolidated into a guide published by Gentle Radiotherapy.
“Improving the accuracy of our treatment delivery will allow us in the future to further increase dose to specific areas with much more precision.”
Dr. Adalsteinn Gunnlaugsson
Increasing radiation dose to the target is becoming more common in cancer treatments, such as intensity modulated radiation therapy (IMRT) or volumetric modulated arc therapy (VMAT), to improve tumor control and lower the risk of recurrence. Another treatment technique is stereotactic body radiation therapy (SBRT), which delivers very precise, high doses of radiation to cancer cells while minimizing radiation exposure to surrounding healthy cells.
Although the department at Skåne University Hospital is not yet using SBRT in the MR-only prostate workflow, Dr. Gunnlaugsson anticipates the development of the MR-only treatment platform will enable SBRT treatments in the future. Even for brachytherapy, another treatment for prostate cancer that involves the placement of radioactive implants directly into the tissue, there is an expectation that an MR-only workflow could be beneficial.
“We also aspire to have gynecological brachytherapy treatments move to MR-only and remove the CT imaging,” adds Gustafsson. “Most of the target delineation today is performed on T2- weighted MR imaging, and we are in the process of optimizing and evaluating the Cube sequences for brachytherapy of the cervix.”
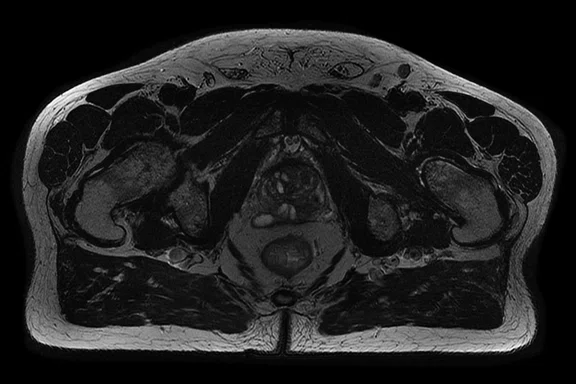
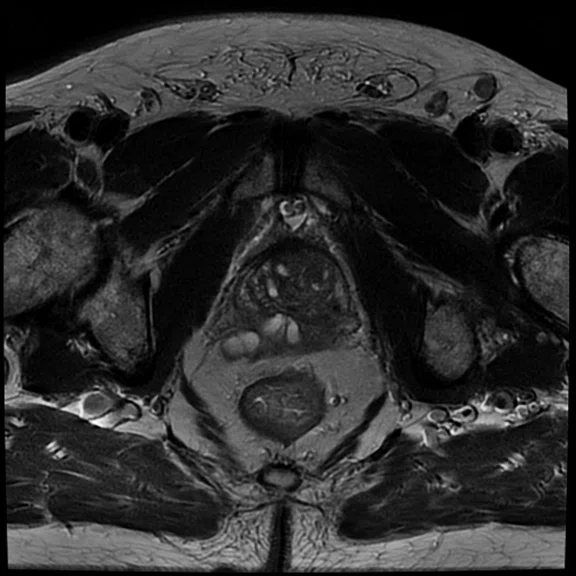
T2-weighted images are predominantly used for target delineation in the prostate and, more recently, in the brain as well. Skåne University Hospital also uses 3D T1 Cube sequences in brain imaging to visualize contrast uptake in the tumors and PROPELLER to compensate for motion. Currently, most of the clinical research has been on morphological rather than functional MR sequences. However, FOCUS, a DWI sequence, is applied in both the prostate and brain using b-values of 200 and 800.
Other protocol adaptations may occur for patients who require the use of vacuum pillows for patient positioning and fixation. “The implication of the use of vacuum pillows or other patient immobilization devices is that the coil may be placed further from the patient’s anatomy, which in turn decreases SNR,” Gustafsson says.
Recently, the last patient was enrolled in the Skåne University Hospital study of prostate patients treated with the MR-only radiation therapy planning process.
Figure 5.
T2-weighted images are predominantly used for target delineation in the prostate. (A-D) PROPELLER is used to compensate for motion. Images copyrighted by Christian Jamtheim Gustafsson, Lund University, reprinted with permission. Thesis: MRI-Only Radiotherapy of Prostate Cancer - Development and evaluation of methods to assess fiducial marker detection, geometric accuracy and dosimetric integrity ISBN: 978-91-7619-775-2.
“Because we tested and validated all aspects of the MR workflow, we were comfortable treating patients in a clinical study,” adds Dr. Gunnlaugsson.
The team is also working to apply the MR-only radiation therapy workflow to brain cancer, including glioma and metastases. For sCT image generation in the brain, IDEAL is utilized to provide water-only, fat-only, out-of-phase and in-phase images. This arm of the research project began in Autumn 2018.
“We are in the validation process and setting up the workflow to implement the same process in the clinic for treatment,” says Minna Lerner, a research PhD student in the department. While much of the workflow developed for prostate cancer can be applied to brain cancers, there are additional considerations that need to be taken into account.
For example, each patient is imaged in the treatment position with their head in an immobilization device. The distance from the back of the head to the MR table must be calculated for dose planning on each patient. Previously, this information would have been manually measured. Lerner is using an ASTM-compatible zero echo time (ZTE) MR imaging technique to calculate the distance.
A key consideration throughout the development of the MR-only radiation therapy planning environment is to replicate the current workflow.
“Once we have all these tools and techniques in place for MR-based radiation therapy, it is not very different from a CT-based workflow. We can use the same clinical criteria as we would in a conventional workflow and we have found the MR-only workflow performs equally well if creating an IMRT or VMAT plan.”
Christian Jamtheim Gustafsson
In addition to using the knowledge gained from MR-only radiation therapy of the prostate in brain cancer cases, the team at Skåne University Hospital is also focused on education. The institution hosted a 2018 GE meeting and two international workshops on the use of MR for radiation therapy planning.
“That is one of our strengths—with the university, we are able to set up educational events around this new technique,” adds Professor Olsson.
From education to sharing protocols to describing the new MR-only workflow, Skåne University Hospital is committed to sharing their insight and expertise in the development of MR-only radiation therapy. While the challenge of being one of the first institutions in the world to embrace an MR-only radiation therapy workflow led to the development of new techniques, tools and processes, the team is eager to continue demonstrating the value of MR imaging in cancer treatment planning.