1. Mai DT, Dao XC, Luong NK, et al. Current State of Stroke Care in Vietnam. Stroke vasc. interv. neurol. 2022;2(2): e000331.
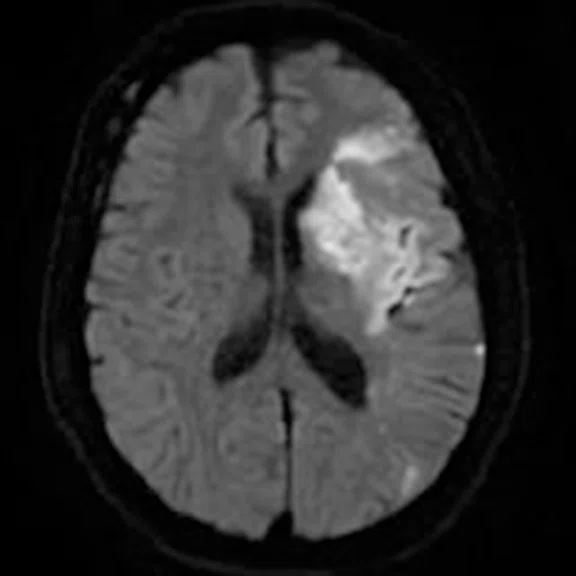
2. Lindner T, Bolar DS, Achten E, et al. Current state and guidance on arterial spin labeling perfusion MRI in clinical neuroimaging. Magn Reson Med. 2023; 89: 2024-2047.
3. Belani P, Kihira S, Pacheco F, Pawha P, Cruciata G, Nael K. Addition of arterial spin-labelled MR perfusion to conventional brain MRI: clinical experience in a retrospective cohort study. BMJ Open. 2020 Jun 11;10(6):e036785.
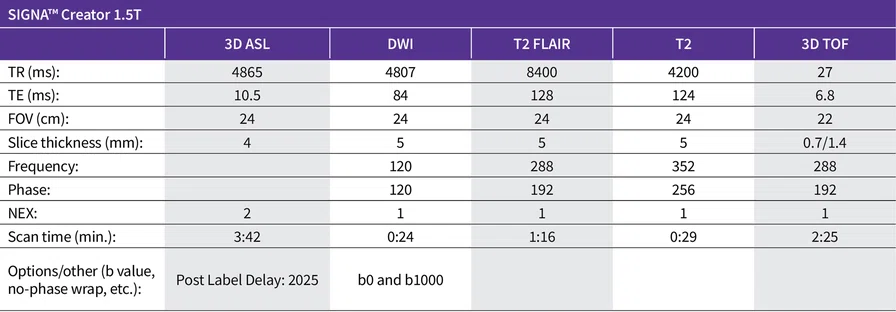
A
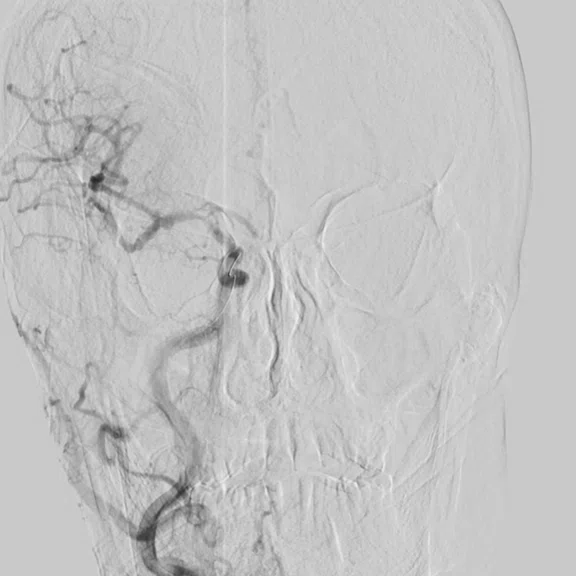
Figure 2.
Same patient as Figure 1. (A) Angiography image before intervention, demonstrating occlusion of the M1 segment of MCA with collateral circulation from the left anterior cerebral artery. (B) Angiography image after intervention with Solitaire™ stent revascularization, demonstrating restoration of blood flow with stenosis of the M1 segment of the MCA.
B
Figure 2.
Same patient as Figure 1. (A) Angiography image before intervention, demonstrating occlusion of the M1 segment of MCA with collateral circulation from the left anterior cerebral artery. (B) Angiography image after intervention with Solitaire™ stent revascularization, demonstrating restoration of blood flow with stenosis of the M1 segment of the MCA.
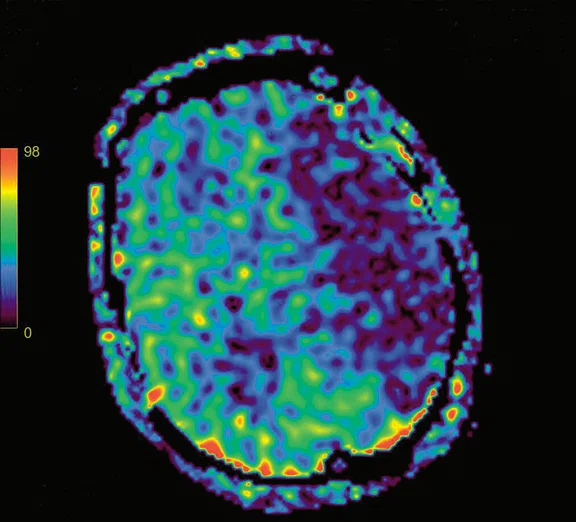
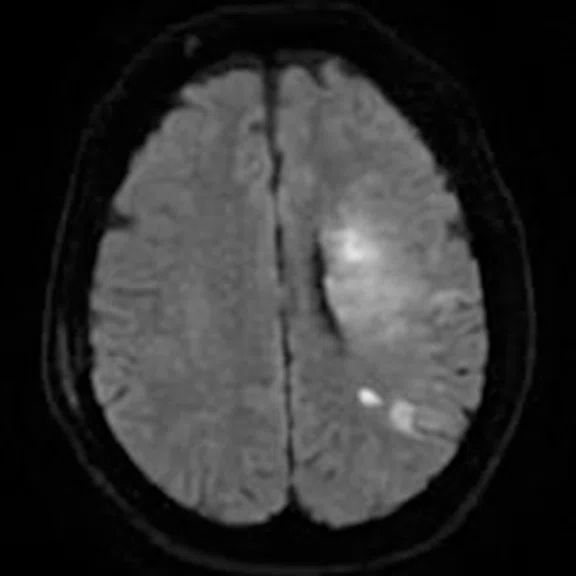
A
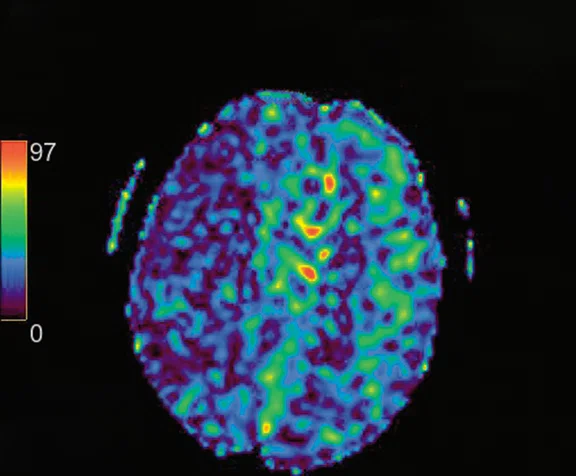
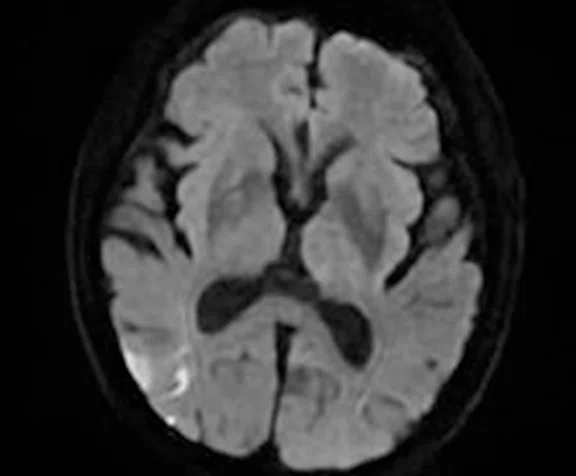
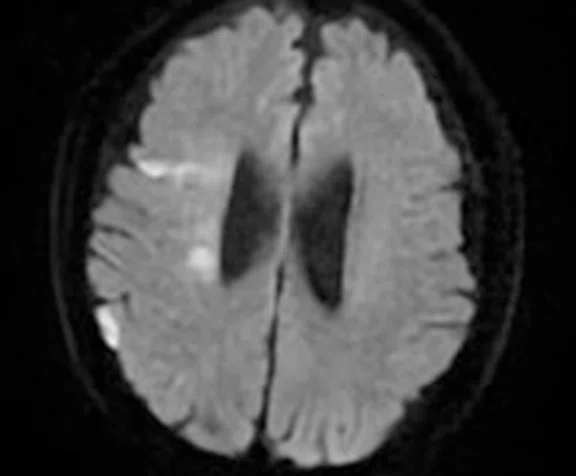
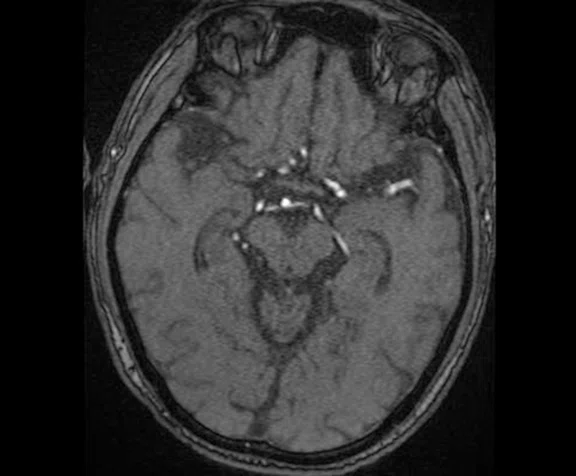
Figure 3.
Case 2, 58-year-old male with left hemiparesis and speech difficulty, initially occurring 11 hours before hospitalization. (A) 3D ASL CBF map, demonstrating hypoperfusion of the right cerebral parenchyma. DWI (B) lower level and (C) upper level showing multiple small infarcts in the territory of the right middle cerebral artery. (D) 3D TOF reveals absent signal from vessels in the same territory. CBF mapping with DWI highlights a large mismatch. The patient was subsequently sent for intervention.
B
Figure 3.
Case 2, 58-year-old male with left hemiparesis and speech difficulty, initially occurring 11 hours before hospitalization. (A) 3D ASL CBF map, demonstrating hypoperfusion of the right cerebral parenchyma. DWI (B) lower level and (C) upper level showing multiple small infarcts in the territory of the right middle cerebral artery. (D) 3D TOF reveals absent signal from vessels in the same territory. CBF mapping with DWI highlights a large mismatch. The patient was subsequently sent for intervention.
C
Figure 3.
Case 2, 58-year-old male with left hemiparesis and speech difficulty, initially occurring 11 hours before hospitalization. (A) 3D ASL CBF map, demonstrating hypoperfusion of the right cerebral parenchyma. DWI (B) lower level and (C) upper level showing multiple small infarcts in the territory of the right middle cerebral artery. (D) 3D TOF reveals absent signal from vessels in the same territory. CBF mapping with DWI highlights a large mismatch. The patient was subsequently sent for intervention.
D
Figure 3.
Case 2, 58-year-old male with left hemiparesis and speech difficulty, initially occurring 11 hours before hospitalization. (A) 3D ASL CBF map, demonstrating hypoperfusion of the right cerebral parenchyma. DWI (B) lower level and (C) upper level showing multiple small infarcts in the territory of the right middle cerebral artery. (D) 3D TOF reveals absent signal from vessels in the same territory. CBF mapping with DWI highlights a large mismatch. The patient was subsequently sent for intervention.
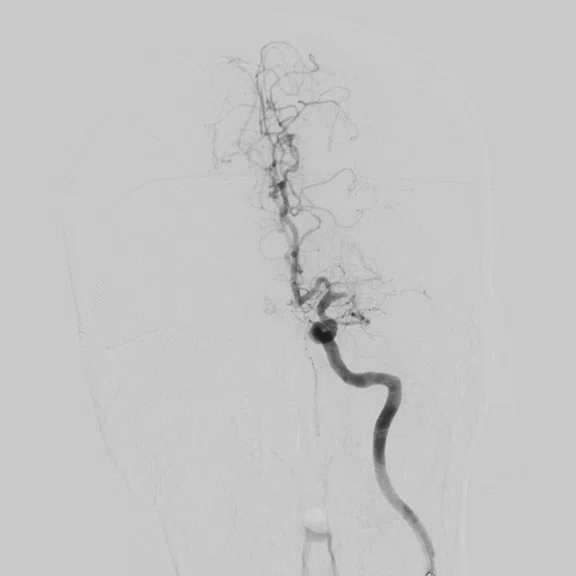
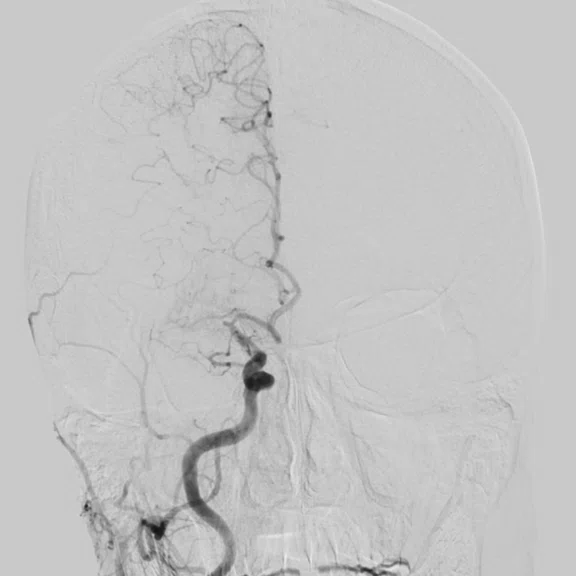
A
Figure 4.
Same patient as Figure 3. (A) Angiography image before intervention, demonstrating stenosis of the M1 segment of the right MCA. (B) Angiography image after intervention with 3MAX thromboaspiration, demonstrating revascularization with 30%-40% stenosis remaining.
B
Figure 4.
Same patient as Figure 3. (A) Angiography image before intervention, demonstrating stenosis of the M1 segment of the right MCA. (B) Angiography image after intervention with 3MAX thromboaspiration, demonstrating revascularization with 30%-40% stenosis remaining.
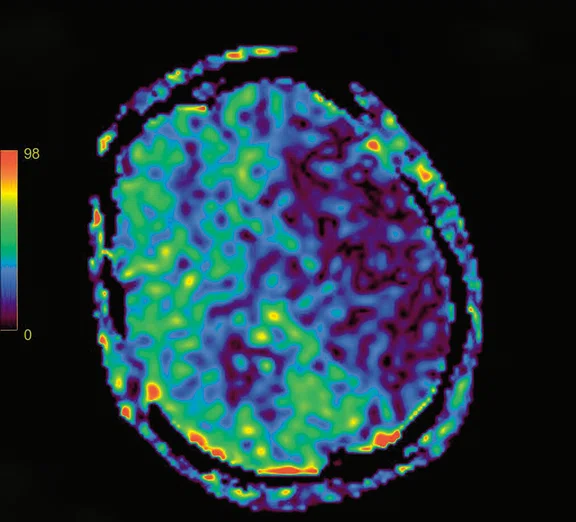
A
Figure 1.
Case 1, 33-year-old male experiencing speech difficulty and right hemiplegia four hours prior to hospitalization. (A, B) The 3D ASL CBF maps, (A) lower level and (B) upper level, demonstrate hypoperfusion in the left cerebral parenchyma within the territory of the middle cerebral artery. (C) T2 FLAIR reveals occlusion of the left middle cerebral artery characterized by a lack of paradoxical vessel enhancement in the same territory on the (D) 3D TOF. The DWI (E) upper level and (F) lower level show hyperintensity of a smaller size compared to that observed on the CBF maps.
B
Figure 1.
Case 1, 33-year-old male experiencing speech difficulty and right hemiplegia four hours prior to hospitalization. (A, B) The 3D ASL CBF maps, (A) lower level and (B) upper level, demonstrate hypoperfusion in the left cerebral parenchyma within the territory of the middle cerebral artery. (C) T2 FLAIR reveals occlusion of the left middle cerebral artery characterized by a lack of paradoxical vessel enhancement in the same territory on the (D) 3D TOF. The DWI (E) upper level and (F) lower level show hyperintensity of a smaller size compared to that observed on the CBF maps.
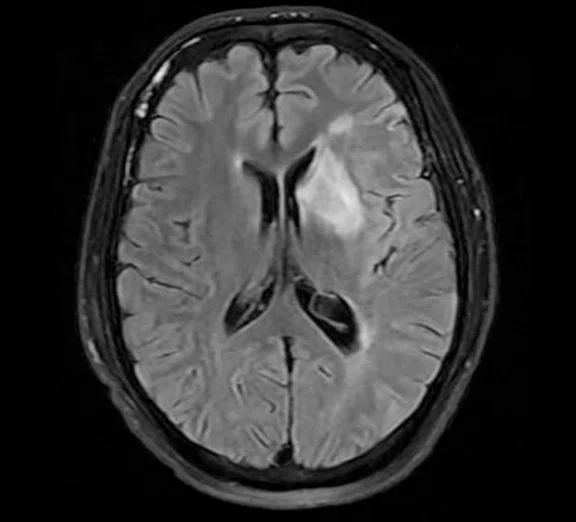
C
Figure 1.
Case 1, 33-year-old male experiencing speech difficulty and right hemiplegia four hours prior to hospitalization. (A, B) The 3D ASL CBF maps, (A) lower level and (B) upper level, demonstrate hypoperfusion in the left cerebral parenchyma within the territory of the middle cerebral artery. (C) T2 FLAIR reveals occlusion of the left middle cerebral artery characterized by a lack of paradoxical vessel enhancement in the same territory on the (D) 3D TOF. The DWI (E) upper level and (F) lower level show hyperintensity of a smaller size compared to that observed on the CBF maps.
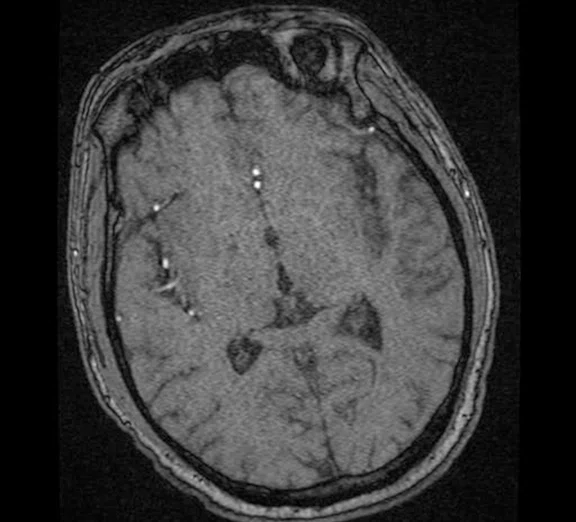
D
Figure 1.
Case 1, 33-year-old male experiencing speech difficulty and right hemiplegia four hours prior to hospitalization. (A, B) The 3D ASL CBF maps, (A) lower level and (B) upper level, demonstrate hypoperfusion in the left cerebral parenchyma within the territory of the middle cerebral artery. (C) T2 FLAIR reveals occlusion of the left middle cerebral artery characterized by a lack of paradoxical vessel enhancement in the same territory on the (D) 3D TOF. The DWI (E) upper level and (F) lower level show hyperintensity of a smaller size compared to that observed on the CBF maps.
E
Figure 1.
Case 1, 33-year-old male experiencing speech difficulty and right hemiplegia four hours prior to hospitalization. (A, B) The 3D ASL CBF maps, (A) lower level and (B) upper level, demonstrate hypoperfusion in the left cerebral parenchyma within the territory of the middle cerebral artery. (C) T2 FLAIR reveals occlusion of the left middle cerebral artery characterized by a lack of paradoxical vessel enhancement in the same territory on the (D) 3D TOF. The DWI (E) upper level and (F) lower level show hyperintensity of a smaller size compared to that observed on the CBF maps.
F
Figure 1.
Case 1, 33-year-old male experiencing speech difficulty and right hemiplegia four hours prior to hospitalization. (A, B) The 3D ASL CBF maps, (A) lower level and (B) upper level, demonstrate hypoperfusion in the left cerebral parenchyma within the territory of the middle cerebral artery. (C) T2 FLAIR reveals occlusion of the left middle cerebral artery characterized by a lack of paradoxical vessel enhancement in the same territory on the (D) 3D TOF. The DWI (E) upper level and (F) lower level show hyperintensity of a smaller size compared to that observed on the CBF maps.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
Case Studies
Non-contrast MR with
deep-learning-based reconstruction
for fast stroke protocol
in acute patient cases
Non-contrast MR with
deep-learning-based reconstruction
for fast stroke protocol
in acute patient cases
By Viet Hung Tran, MD, Radiologist, Hanoi Medical University Hospital, Vietnam
Stroke is the leading cause of death and disability in Vietnam, with an incidence and prevalence at 161 and 415 per 100,000 people, respectively. This is despite only 7.7% of the total population in Vietnam is aged 65 years or older, an age where strokes are most likely to occur.1
At Hanoi Medical University Hospital (HMUH), the protocol for hyper-acute infarcted patients who are within 6 hours of onset undergo a CT angiography examination to evaluate bleeding and large vessel occlusion for thrombolysis or intervention procedures. For patients with unclear onset or onset over 6 hours, a brain MR including MR angiography (MRA) is prescribed.
Patients having small infarction cores, large vessel occlusion (middle cerebral artery [MCA], internal carotid) on TOF 3D and/or suspected thrombosis on SWAN imaging undergo dynamic susceptibility contrast (DSC) MR perfusion. However, the availability of 3D ASL has nearly replaced the DSC MR perfusion for scanning of emergency stroke patients at HMUH.
3D ASL is a non-contrast technique, using hydrogen protons as an endogenous contrast to produce the quantitative mapping of cerebral blood flow (CBF), which we have found is almost equivalent in value to the DSC technique in emergency cases. It can identify the mismatch zone between the infarct core (brain parenchyma that has been infarcted or will be infarcted regardless of reperfusion) and the penumbra zone (severely hypoperfused area on 3D ASL). Penumbra is a region of brain tissue surrounding the core infarct area that is at risk of irreversible damage, but still potentially salvageable with prompt intervention.
3D ASL is an alternative solution that acquires similar image quality of CBF maps compared to the DSC technique. Therefore, it can be used for evaluation of acute stroke in high-risk cases, such as patients with kidney disease, allergic to gadolinium, or unable to tolerate contrast media due to other adverse effects. 3D ASL provides valuable diagnostic information comparable to DSC MR perfusion in a routine brain MR and MRA for evaluating acute stroke, as has been shown in several published studies.2,3
The addition of deep-learning-based reconstruction techniques, such as AIR™ Recon DL in compatible sequences, is a game changer in clinical practice. The scanning time reduction enhances patients’ comfort while maintaining the image quality in difficult acute cases such as stroke.
Figure 1.
Case 1, 33-year-old male experiencing speech difficulty and right hemiplegia four hours prior to hospitalization. (A, B) The 3D ASL CBF maps, (A) lower level and (B) upper level, demonstrate hypoperfusion in the left cerebral parenchyma within the territory of the middle cerebral artery. (C) T2 FLAIR reveals occlusion of the left middle cerebral artery characterized by a lack of paradoxical vessel enhancement in the same territory on the (D) 3D TOF. The DWI (E) upper level and (F) lower level show hyperintensity of a smaller size compared to that observed on the CBF maps.
Case 1
Patient history
A 33-year-old male weighing 176 lbs. (80 kg) experiencing speech difficulty and right hemiplegia 4 hours prior to hospitalization. Muscle strength was rated 1/5.
Results
Based on the MR exam, the infarcts were located in the territory of the MCA, and an occlusion of the left MCA was noticed on the routine sequences.
The use of 3D ASL confirmed the penumbra, which was found to be larger on the 3D ASL CBF maps compared to DWI, resulting in a large mismatch. In cases of a DWI-3D ASL mismatch or an Alberta Stroke Program Early CT score of more than 7, the patient will undergo endovascular clot removal.
In this case, the patient was indicated for intervention of the occlusion in the M1 segment of the MCA, with collateral circulation from the left anterior cerebral artery. After Solitaire™ stent revascularization, the blood flow was restored; however, stenosis of the M1 segment of the MCA was noted. Patient was referred to cardiologist for anticoagulation therapy. Patient demonstrated significant improvement post-intervention, with muscle strength 4/5 in right legs and 3/5 in right hands. Gait remained unsteady and patient was unable to hold objects in their right hand. Patient was discharged 10 days after treatment.
Figure 2.
Same patient as Figure 1. (A) Angiography image before intervention, demonstrating occlusion of the M1 segment of MCA with collateral circulation from the left anterior cerebral artery. (B) Angiography image after intervention with Solitaire™ stent revascularization, demonstrating restoration of blood flow with stenosis of the M1 segment of the MCA.
Figure 3.
Case 2, 58-year-old male with left hemiparesis and speech difficulty, initially occurring 11 hours before hospitalization. (A) 3D ASL CBF map, demonstrating hypoperfusion of the right cerebral parenchyma. DWI (B) lower level and (C) upper level showing multiple small infarcts in the territory of the right middle cerebral artery. (D) 3D TOF reveals absent signal from vessels in the same territory. CBF mapping with DWI highlights a large mismatch. The patient was subsequently sent for intervention.
Case 2
Patient history
A 58-year-old male weighing 123 lbs. (56 kg) presented with left hemiparesis and speech difficulty, initially occurring 11 hours before hospitalization. Muscle strength of left hemiplegia was rated 1/5.
Results
Multiple small infarcts scattered on the right cerebral hemisphere (the right middle cerebral artery territory) were noted on MR examination. The right hypoperfusion area was obvious on 3D ASL derived CBF map. A large mismatch was noted between DWI and 3D ASL. Patient was referred for intervention.
Revascularization and balloon angioplasty for the right MCA stenosis (thrombolysis in Cerebral Infarction scale: grade 3) was performed. 3MAX catheter for thromboaspiration was previously performed and no thrombosis was noted. However, the stenosis of the M1 segment of right MCA was detected. Patient previously underwent three PTA balloon catheter, 2.5/10mm, to treat the stenosis. Angiography depicts good blood flow restoration although 30%-40% stenosis remains. The patient’s left muscle strength improved to 3-4/5 and was discharged 10 days after treatment.
Discussion
At HMUH, AIR™ Recon DL improves image quality while also reducing scanning time. The 3D ASL sequence has a similar acquisition time as the DSC perfusion technique (including preparation time) of approximately 4 minutes; however, the 3D ASL post-processing is integrated in the MR reconstruction and does not require any additional post-processing steps to produce maps or reports. As a result, we can evaluate the CBF map and quantitative values within 5 minutes after the sequence is acquired. 3D ASL image quality and quantitative hemodynamic CBF maps are comparable to contrast-enhanced MR perfusion (DSC) without the time or preparation required for an intravenous line. Utilizing the non-contrast 3D ASL technique also allows for use in patients who would otherwise be contraindicated for gadolinium, such as patients with renal disease/failure or allergy.
As a result of implementing AIR™ Recon DL and 3D ASL, we have achieved a fast stroke protocol of approximately 10 minutes, compared to 20 minutes previously, while maintaining image quality. This is pivotal for stroke patients who urgently need the proper treatment and intervention.
Based on our experience with 3D ASL, our protocol for all patients with suspected ischemic stroke, excluding hemorrhagic stroke, includes a brain MR and MRA with the 3D ASL pulse sequence replacing DSC. 3D ASL is an important sequence that guides the clinician in the decision to undergo interventional treatment on patients.
Clinicians (i.e., interventional neurologists and emergency physicians) and radiologists all agree that 3D ASL has good diagnostic image quality comparable to the conventional DSC perfusion in stroke cases, although there is a limitation that only the CBF map is acquired. 3D ASL provides a reliable diagnosis and supports emergency physicians and interventional neurologists in providing the proper treatment strategies (intravenous fibrinolytic therapy, endovascular thrombectomy, balloon angioplasty, etc.).
The effectiveness of the interventions are relatively good as shown in the two cases presented, with the improvement of patient symptoms and the reduction of the degree of paralysis.
DOWNLOAD ARTICLE HERE