2. Artamonov AK, Kaneva MA, Gordeeva NA, Sorokina LS, Kostik MM. Temporomandibular Joint Involvement in Juvenile Idiopathic Arthritis: The Results from a Retrospective Cohort Tertial Center Study. Life (Basel). 2023 May 11;13(5):1164.
1. Arthritis Foundation. Juvenile Idiopathic Arthritis. Available at: https://www.arthritis.org/diseases/juvenile-idiopathic-arthritis. Accessed on Feb. 20, 2024.
4. CureSearch for Children’s Cancer. Diagnosing Wilms Tumor and Other Kidney Tumors. Available at: https://curesearch.org/Wilms-Tumor-Just-Diagnosed#:~:text=Currently %2C%20the%20great%20majority%20of,after%20their%20cancer%20is%20diagnosed. Accessed on Feb. 20, 2024.
3. Vujanić GM, Gessler M, Ooms AHAG, et al. International Society of Paediatric Oncology–Renal Tumour Study Group (SIOP–RTSG). The UMBRELLA SIOP-RTSG 2016 Wilms tumour pathology and molecular biology protocol. Nat Rev Urol. 2018 Nov;15(11):693-701.
5. Grattan-Smith JD, Chow J, Kurugol S, Jones RA. Quantitative renal magnetic resonance imaging: magnetic resonance urography. Pediatr Radiol. 2022 Feb;52(2):228-248.
A
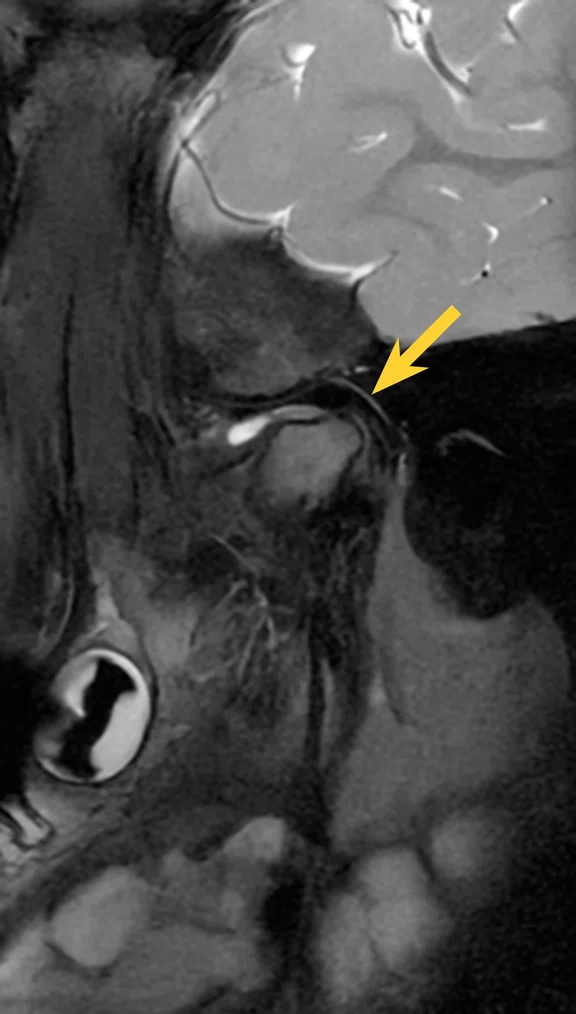
Figure 1.
Case 1, 5-year-old patient with JIA demonstrating thickened synovium and flattened mandibular condyle (arrow). AIR™ Recon DL was used in all sequences shown. (A) Sagittal T2 FatSat, 0.3 x 0.4 x 2 mm, 2:32 min.; (B) sagittal PD, 0.3 x 0.4 x 2 mm, 2:48 min.; (C) sagittal T1 FatSat with contrast, 0.3 x 0.4 x 2 mm, 3:47 min.; (D) sagittal 3D FSPGR, 0.5 x 0.5 x 0.5 mm (1 mm), 3:38 min.; (E) sagittal ZTE (DL-MUPA)‡ 0.5 x 0.5 x 0.5 mm (1 mm), 5:07 min.
B
Figure 1.
Case 1, 5-year-old patient with JIA demonstrating thickened synovium and flattened mandibular condyle (arrow). AIR™ Recon DL was used in all sequences shown. (A) Sagittal T2 FatSat, 0.3 x 0.4 x 2 mm, 2:32 min.; (B) sagittal PD, 0.3 x 0.4 x 2 mm, 2:48 min.; (C) sagittal T1 FatSat with contrast, 0.3 x 0.4 x 2 mm, 3:47 min.; (D) sagittal 3D FSPGR, 0.5 x 0.5 x 0.5 mm (1 mm), 3:38 min.; (E) sagittal ZTE (DL-MUPA)‡ 0.5 x 0.5 x 0.5 mm (1 mm), 5:07 min.
C
Figure 1.
Case 1, 5-year-old patient with JIA demonstrating thickened synovium and flattened mandibular condyle (arrow). AIR™ Recon DL was used in all sequences shown. (A) Sagittal T2 FatSat, 0.3 x 0.4 x 2 mm, 2:32 min.; (B) sagittal PD, 0.3 x 0.4 x 2 mm, 2:48 min.; (C) sagittal T1 FatSat with contrast, 0.3 x 0.4 x 2 mm, 3:47 min.; (D) sagittal 3D FSPGR, 0.5 x 0.5 x 0.5 mm (1 mm), 3:38 min.; (E) sagittal ZTE (DL-MUPA)‡ 0.5 x 0.5 x 0.5 mm (1 mm), 5:07 min.
D
Figure 1.
Case 1, 5-year-old patient with JIA demonstrating thickened synovium and flattened mandibular condyle (arrow). AIR™ Recon DL was used in all sequences shown. (A) Sagittal T2 FatSat, 0.3 x 0.4 x 2 mm, 2:32 min.; (B) sagittal PD, 0.3 x 0.4 x 2 mm, 2:48 min.; (C) sagittal T1 FatSat with contrast, 0.3 x 0.4 x 2 mm, 3:47 min.; (D) sagittal 3D FSPGR, 0.5 x 0.5 x 0.5 mm (1 mm), 3:38 min.; (E) sagittal ZTE (DL-MUPA)‡ 0.5 x 0.5 x 0.5 mm (1 mm), 5:07 min.
E
Figure 1.
Case 1, 5-year-old patient with JIA demonstrating thickened synovium and flattened mandibular condyle (arrow). AIR™ Recon DL was used in all sequences shown. (A) Sagittal T2 FatSat, 0.3 x 0.4 x 2 mm, 2:32 min.; (B) sagittal PD, 0.3 x 0.4 x 2 mm, 2:48 min.; (C) sagittal T1 FatSat with contrast, 0.3 x 0.4 x 2 mm, 3:47 min.; (D) sagittal 3D FSPGR, 0.5 x 0.5 x 0.5 mm (1 mm), 3:38 min.; (E) sagittal ZTE (DL-MUPA)‡ 0.5 x 0.5 x 0.5 mm (1 mm), 5:07 min.
A
Figure 4.
Same patient as Figure 3. (A-C) DISCO with HyperSense, navigated, 1.1 x 1.6 x 2.8 mm, approx. 20 min.
B
Figure 4.
Same patient as Figure 3. (A-C) DISCO with HyperSense, navigated, 1.1 x 1.6 x 2.8 mm, approx. 20 min.
C
Figure 4.
Same patient as Figure 3. (A-C) DISCO with HyperSense, navigated, 1.1 x 1.6 x 2.8 mm, approx. 20 min.
A
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown. (A, B) Before treatment,
(A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm, 3:16 min.
C
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown. (A, B) Before treatment,
(A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm, 3:16 min.
D
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown. (A, B) Before treatment,
(A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm, 3:16 min.
F
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown. (A, B) Before treatment,
(A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm, 3:16 min.
B
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown. (A, B) Before treatment,
(A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm, 3:16 min.
E
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown. (A, B) Before treatment,
(A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm, 3:16 min.
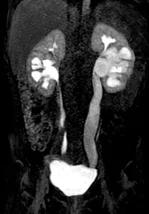
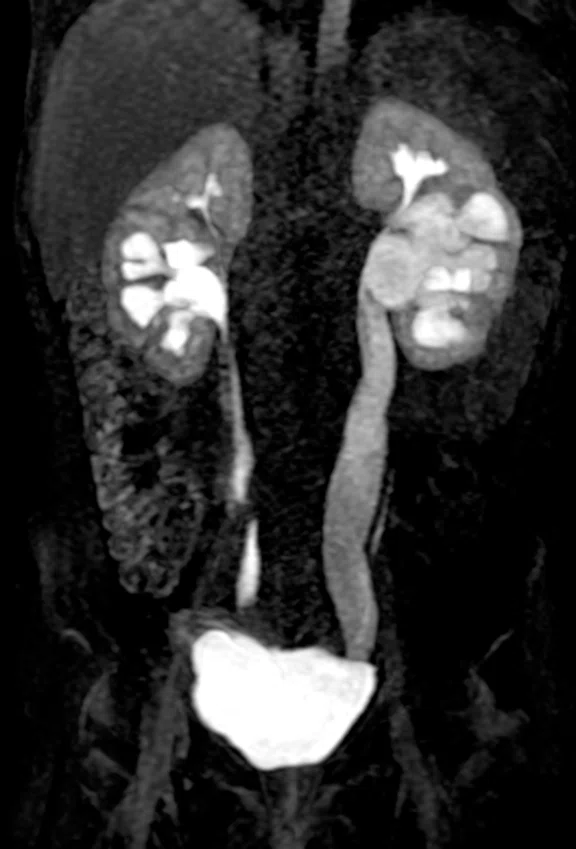
A
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown.
(A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
B
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown.
(A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
C
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown.
(A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
D
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown.
(A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
E
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown.
(A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
3. Vujanić GM, Gessler M, Ooms AHAG, et al. International Society of Paediatric Oncology–Renal Tumour Study Group (SIOP–RTSG). The UMBRELLA SIOP-RTSG 2016 Wilms tumour pathology and molecular biology protocol. Nat Rev Urol. 2018 Nov;15(11):693-701.
A
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown.
(A, B) Before treatment, (A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm,
3:16 min.
c
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown. (A, B) Before treatment, (A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm, 3:16 min.
D
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown.
(A, B) Before treatment, (A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm,
3:16 min.
F
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown.
(A, B) Before treatment, (A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm, 3:16 min.
B
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown.
(A, B) Before treatment, (A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm,
3:16 min.
E
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown.
(A, B) Before treatment, (A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm,
3:16 min.
A
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown. (A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
B
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown. (A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
C
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown. (A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
D
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown. (A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
E
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown. (A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
result


PREVIOUS
${prev-page}
NEXT
${next-page}
Subscribe Now
Manage Subscription
FOLLOW US
Contact Us • Cookie Preferences • Privacy Policy • California Privacy PolicyDo Not Sell or Share My Personal Information • Terms & Conditions • Security
© 2024 GE HealthCare. GE is a trademark of General Electric Company. Used under trademark license.
Case Studies
Rapid MR protocols in complex pediatric brain and abdominal evaluations
Rapid MR protocols in complex pediatric brain and abdominal evaluations
by Christian Kellenberger, MD, Professor of Pediatric Radiology and Radiologist-in-Chief, University Children’s Hospital Zürich, Switzerland
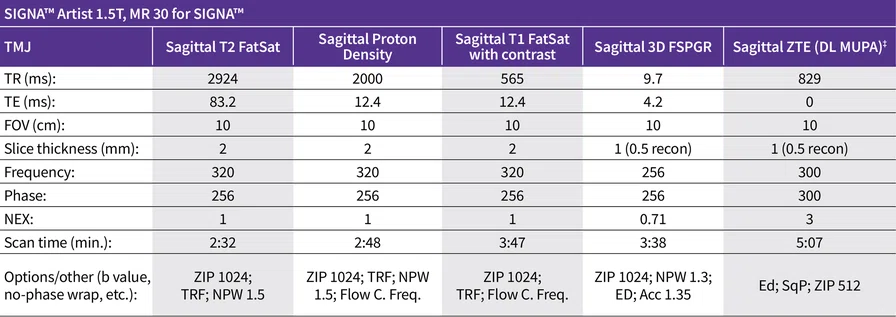
As a leading European pediatric center of excellence, we see a variety of indications and conditions, from complex to routine. MR is an integral tool in the diagnostic workup of many patients and is often the definitive imaging modality for lesion characterization, treatment planning and guiding management.
In pediatric imaging, long MR scan times require longer sedation times or in some cases general anesthesia. Therefore, we utilize any available technologies that can decrease scan and total examination times. Cases that involve abdominal imaging are also susceptible to motion artifacts due to breathing.
Our hospital was one of the first pediatric centers to evaluate and employ AIR™ Recon DL, a deep-learning-based reconstruction technology that allows us to simultaneously improve image quality and shorten scan times. Our MR protocols have been optimized to utilize this technology, including in 3D and PROPELLER sequences with the upgrade to MR 30 for SIGNA™. PROPELLER is an important sequence in abdominal imaging, enabling free-breathing acquisition with reduced motion artifacts. The AIR™ Coils provide the flexibility to adapt to different patient body habitus and sizes with greater patient comfort compared to conventional hard-shell coils. We utilize the AIR™ Anterior Array (AA) Coil and the AIR™ Multi-Purpose (MP) 20-channel and 21-channel coils. The MR table has the embedded 40-channel Posterior Array (PA).
Figure 1.
Case 1, 5-year-old patient with JIA demonstrating thickened synovium and flattened mandibular condyle (arrow). AIR™ Recon DL was used in all sequences shown. (A) Sagittal T2 FatSat, 0.3 x 0.4 x 2 mm, 2:32 min.; (B) sagittal PD, 0.3 x 0.4 x 2 mm, 2:48 min.; (C) sagittal T1 FatSat with contrast, 0.3 x 0.4 x 2 mm, 3:47 min.; (D) sagittal 3D FSPGR, 0.5 x 0.5 x 0.5 mm (1 mm), 3:38 min.; (E) sagittal ZTE (DL-MUPA)‡ 0.5 x 0.5 x 0.5 mm (1 mm), 5:07 min.
Case 1
A 5-year-old patient with juvenile idiopathic arthritis (JIA), polyarticular type, was referred for evaluation of the presence and extent of arthritis and deformations in the temporomandibular joints (TMJ).
Results
Severely flattened articular fossa and severely flattened mandibular condyle. No erosions. Length of the mandibular ramus is 37 mm, asymmetrically shortened. Normal bone marrow signal marrow without increased contrast agent enhancement in the mandibular ramus. Orthotopic centrally thinned articular disk. Somewhat increased intra-articular fluid. Significantly thickened synovium with increased contrast enhancement.
Discussion
The involvement of TMJ in cases of JIA is a marker of disease severity; however, diagnosis can be difficult.1 Acute inflammation of the TMJ is often clinically silent. It is estimated that more than 50% of children with JIA have jaw involvement, resulting in difficulty chewing, brushing or flossing.2 There is also the possibility of dentofacial deformities and in this case we were looking for changes in the bone of the TMJ at the time of JIA diagnosis.
The patient was required to remain still without swallowing during the image acquisition. We were able to use the smaller 20-channel AIR™ Multi-Purpose Coil for coverage of both TMJs, providing greater patient comfort. AIR™ Recon DL and the AIR™ Coil allowed for a shorter imaging study without impacting image quality or diagnostic confidence.
Based on the results of the MR examination, patient was referred
for systemic treatment of JIA.
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown. (A, B) Before treatment, (A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER,
0.9 x 0.9 x 5 mm, 3:16 min.
Figure 2.
Case 2, 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney (arrow). AIR™ Recon DL was used in all sequences shown. (A, B) Before treatment, (A) axial T2 FatSat PROPELLER with respiratory triggering, 0.8 x 0.8 x 5 mm, 2:53 min. and (B) axial T1 PROPELLER, 0.7 x 0.7 x 5 mm, 4:50 min. (C-F) After treatment, (C) coronal STIR with HyperCube and HyperSense, navigated, 1.2 x 1.2 x 1.4 mm (2.8 mm), 3:10 min.; (D) axial T2 FatSat PROPELLER with respiratory triggering, 0.9 x 0.9 x 5 mm, 3:23 min.; (E) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 3:10 min.; and (F) coronal T1 PROPELLER, 0.9 x 0.9 x 5 mm, 3:16 min.
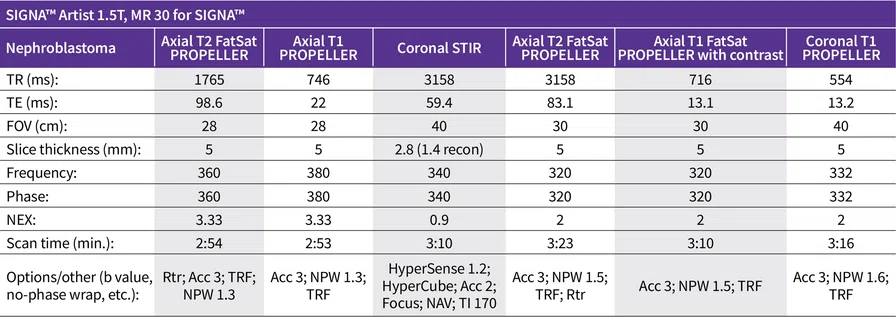
Case 2
A 4-year-old patient with nephroblastoma (Wilms tumor) in the left kidney, initially diagnosed as intermediate risk for relapse. Patient underwent left nephrectomy according to UMBRELLA SIOP-RTSG 2016 (UMBRELLA Protocol)3 and was in the second year of follow-up imaging to look for signs of relapse/recurrence.
Findings
No evidence of a recurrent or second tumor in the remaining right kidney.
Compared to the previous examination, lung nodules in the posterobasal left lower lobe were again better defined, similar to the prior year examination, and therefore, in conjunction with older preliminary examinations, can be assessed primarily as post-inflammatory. Follow-up checks recommended as part of aftercare.
Discussion
Nephroblastoma, or Wilms tumor, is the most common type of pediatric renal and abdominal cancer, with a five-year survival rate of 90%, at which point the patient is considered “cured.”4 It is estimated that approximately 92% of these tumors have favorable histology and are curable; however, anaplasia is recognized as a high-risk tumor feature in nephroblastoma that typically results in a worse prognosis.3 Yearly surveillance with MR is often employed to detect recurrence until the patient reaches the five-year survival rate.
The use of HyperSense, HyperCube and AIR™ Recon DL enabled us to acquire a complete abdominal MR study for evaluation of nephroblastoma in approximately 20 minutes with improved
image quality.
Case 3
A 5-year-old patient with vesicoureteral reflux grade IV to the right ureter and grade III to the left lower pole moiety. Bilateral Cohen ureterocystoneostomy (UCN) was performed when patient was a neonate. Renal scintigraphy performed when patient was 3 years old showed partial kidney function on the left at 52% and on the right at 48%.
Recent follow-up with ultrasound showed increasing pelvicalyceal dilation, suggestive of complicative ureteral obstruction with impaired drainage.
Findings
In the evaluation of both kidneys, the lower pelvicalyceal systems are dilated, with mild dilatation on the right side and moderate dilatation, including the ureter, on the left side. Functional evaluation showed no relevant obstruction after bilateral UCN according to Cohen. Differential renal function: right is 49% (upper pole is 60% and lower pole is 40%) and left is 51% (upper pole is 53% and lower pole is 47%).
Discussion
A high-quality morphological and functional study is essential for patient management decisions in children with congenital anomalies of the kidneys and urinary tracts (CAKUT). MR urography typically suffers from artifacts due to respiration or patient motion if patient is not sedated. Additionally, a high temporal resolution of less than 10 seconds is required for the dynamic functional study.
In this case, the use of HyperCube and AIR™ Recon DL significantly shortened scan times for the T1, T2 and FOCUS DWI sequences, while the use of HyperSense in the DISCO navigated sequence allowed for a comprehensive contrast-enhanced evaluation of the kidneys. Dynamic contrast-enhanced imaging is required for functional MR urography assessing differential renal function (in this case of the upper and lower moieties bilaterally) and drainage of the urinary tracts (obstruction).5
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown. (A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
Figure 3.
Case 3, 5-year-old patient with known congenital anomalies of the kidney and urinary tract (CAKUT) (arrows). AIR™ Recon DL was used in all sequences shown. (A) Coronal T2 FatSat with HyperCube and HyperSense, navigated, 0.8 x 0.8 x 0.8 mm, 4:13 min. with (B, C) multi-planar reconstructions; (D) axial T1 FatSat PROPELLER with contrast, 0.9 x 0.9 x 5 mm, 1:52 min.; and (E) axial FOCUS DWI b800, 1.5 x 1.8 x 5 mm, 4:39 min.
DOWNLOAD ARTICLE HERE